Aggrenox
General Information about Aggrenox
The distinctive mixture of these two components produces a stronger antiplatelet effect in comparability with utilizing either one alone. This makes Aggrenox an important treatment for people who have already experienced a stroke or TIA and are in danger for an additional. By stopping blood clots from forming, Aggrenox reduces the likelihood of further problems and improves general quality of life.
Aside from its use in ischemic stroke, Aggrenox has also been discovered to be effective in preventing transient ischemic attacks (TIA), also called mini-strokes. TIAs are just like ischemic strokes however are short-term and don't cause permanent mind injury. However, they're typically a warning sign that a more extreme stroke might happen sooner or later. Aggrenox has been proven to scale back the risk of recurrent TIAs, making it an essential treatment for individuals who have experienced these episodes.
In conclusion, Aggrenox is a strong medicine extensively used for secondary prevention of ischemic stroke and TIA. Its distinctive combination of acetilsalicylic acid and dipiridamol produces a robust antiplatelet effect, making it an effective drug in preventing blood clots. If you have a history of stroke or TIA, it's essential to talk to your healthcare supplier about Aggrenox as it could significantly reduce your threat of experiencing a recurrent episode. However, like several treatment, it's essential to follow your healthcare provider's instructions and report any side effects that you would be expertise.
Aggrenox is a strong medication used for the prevention of strokes and transient ischemic attacks (TIA). It is a combination of two energetic components - acetilsalicylic acid and dipiridamol. This distinctive combination creates a strong antiplatelet impact, making it a helpful treatment for people who have already skilled a stroke or TIA and are in danger for one more.
Aggrenox is out there in capsule form and is often taken twice a day. The dosage might range depending on the person's medical history and the advice of their healthcare provider. While most individuals tolerate Aggrenox properly, some might expertise unwanted side effects corresponding to headache, nausea, and upset abdomen. If these unwanted facet effects turn out to be bothersome, it's essential to speak to a healthcare provider for potential options.
The lively elements in Aggrenox work in numerous ways to prevent blood clots from forming. Acetilsalicylic acid, commonly often identified as aspirin, works by inhibiting the manufacturing of certain enzymes which are involved in clotting. This prevents platelets from sticking together and forming blood clots. On the other hand, dipiridamol works by dilating the blood vessels, allowing extra blood flow, and by inhibiting the production of drugs which may be answerable for selling blood clots.
The main use of Aggrenox is for secondary prevention of ischemic stroke, which is brought on by a blockage in one of many blood vessels supplying blood to the mind. These blockages are often a results of atherosclerosis, a situation by which plaque builds up within the arteries, causing them to slim and restrict blood flow. Ischemic stroke is usually a life-threatening situation, and Aggrenox has been proven to be effective in stopping further episodes.
Early third-trimester ultrasound screening in gestational diabetes to determine the risk of macrosomia and labor dystocia at term symptoms of cheap aggrenox caps american express. Adequate timing of fetal ultrasound to guide metabolic therapy in mild gestational diabetes mellitus. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. A postnatal fasting plasma glucose is useful in determining which women with gestational diabetes should undergo a postnatal oral glucose tolerance test. In addition, we would suggest the following: Theoretical skills · Distinguish between the different causes of hypertension in pregnancy. Practical skills · Know how to manage the woman with severe pre-eclampsia; this will involve detailed knowledge of fluid management, hypertension control, anticonvulsant prophylaxis and anaesthetic issues. The aetiology and management of the three conditions are very disparate, as are implications for future pregnancies. The aetiology and management of chronic hypertension in pregnancy are discussed in Chapter 6. Eclampsia is now rarely associated with mortality, although severe hypertension and cerebral vascular accidents still occur. Worldwide, however, maternal mortality from hypertensive disease accounts for approximately 60 000 deaths per year. Because of concerns about the potential adverse effects of pre-eclampsia, many women who have a normal outcome require intensive surveillance; up to a quarter of antenatal admissions are as a direct result of monitoring and managing women with hypertension. Antenatal care is directed towards identifying women with hypertension Incidence 185 and proteinuria. Day units reduce the need for inpatient management, but current methods for screening women at risk are poor and the onset and progression of the disease are unpredictable. As delivery is the only cure, the hypertensive diseases of pregnancy have become the most common cause of iatrogenic preterm birth. They account for 15 per cent of all preterm births, but up to a quarter of very low birth weight infants. Maternal disease severity and fetal involvement do not always correlate; for example, the babies of women who have eclampsia at term often have normal birth weight. Gestational hypertension and/or proteinuria developing during pregnancy, labour or the puerperium in a previously normotensive non-proteinuric woman 1. Chronic hypertension (before the 20th week of pregnancy) and chronic renal disease (proteinuria before the 20th week of pregnancy) 1. Blood pressure and proteinuria define pre-eclampsia, but they are not fundamental to the aetiology and are more indicative of end-organ damage. In clinical practice, the threshold of abnormality is set low to identify at-risk cases, but this results in many women being identified with hypertension and/or proteinuria who are not at increased risk. If any organ system known to have the potential to be affected by pre-eclampsia is involved, the possibility of the disease must be suspected; hypertension and proteinuria cannot be relied upon to define the disease. Tests for liver, kidney, blood and placental involvement should always be sought if pre-eclampsia is suspected (see below). In the United States, the incidence of pre-eclampsia has been reported to be slightly higher, possibly because of the high-risk status of the populations studied (usually primiparous women at large teaching centres). The incidence of Antenatal complications: maternal 186 Pre-eclampsia and non-proteinuric pregnancy-induced hypertension pre-eclampsia in women with a single risk factor is approximately 15 per cent. Although the inheritance of pre-eclampsia has yet to be characterized, there is a strong familial predisposition: a family history in either mother or sister increases the risk of pre-eclampsia four- to eight-fold. This genetic predisposition leads to a faulty interplay between the invading extravillous trophoblast cells (of fetal origin) and the maternal immunologically active decidual cells. The faulty interplay results in a failure of trophoblast invasion into the myometrium and the maternal spiral arteries do not undergo their physiological vasodilatation. This inadequate trophoblast invasion is also seen in pregnancies complicated by fetal growth restriction (without pre-eclampsia), demonstrating that the maternal syndrome of pre-eclampsia must be related to additional factors. The diminished dilatation of the spiral arteries, associated increased resistance in the uteroplacental circulation and an impaired intervillous blood flow probably result in an inadequately perfused placenta. Ischaemia or ischaemia/ reperfusion in the second half of gestation produces reactive oxygen species and oxidative stress in the placenta. Pre-eclampsia is associated with lipid changes (there is a two-fold increase in triglycerides and free fatty acids), and an increase in lipid peroxidation, both in the placenta and systemically, suggests that oxidative stress (an imbalance between free radical synthesis and antioxidant defence) may be involved in the endothelial cell changes. A family history in a first-degree relative increases the risk of pre-eclampsia four- to eight-fold, illustrating the strong genetic influence [D]. A woman has double the risk of pre-eclampsia if pregnant by a partner who had previously fathered an affected pregnancy [D]. An immunological element to the disease process is evidenced by the effect of exposure to the paternal antigen, via either the fetus or the partner. Pre-eclampsia occurs more commonly in first pregnancies; miscarriages or terminations of pregnancy provide some reduction in risk in subsequent pregnancies [D]. However, in women with chronic hypertension, a prior miscarriage is a risk factor for progression to pre-eclampsia. A new partner increases risk, whereas non-barrier methods of contraception and increased duration of sexual cohabitation reduce risk [D]. Teenage mothers and pregnancies conceived by donor insemination have increased risk of preeclampsia, presumably due to the lack of exposure to such antigens [D]. Underlying medical disorders, particularly those involving vascular disease such as chronic hypertension increase the risk of pre-eclampsia (to over 20 per cent); this highlights the importance of the maternal susceptibility, as well as the placental aetiology in the disease process. All forms of glucose intolerance, including gestational diabetes, are associated with an increased risk [D].
Skin allografts 177 Chapter 15 Transplantation plete by day 14 when the graft takes on a black and shrunken appearance medications narcolepsy generic aggrenox caps 25/200mg amex. These immunoglobulins, working in conjunction with complement, neutrophil polymorphs or other Fc receptor-bearing cells can then mediate lysis of donor cells. A major advance in recent years has been the realization that much of the immunogenicity of grafted tissues is due to the presence of donor antigenpresenting cells originally referred to as passenger leucocytes but now known to be dendritic cells (p. Indirect recognition involves processing and presentation of donor alloantigenic peptides. Very few donor dendritic cells are required to elicit an allograft response by direct recognition and if they are removed prior to grafting so that induction of the allograft response has to occur via indirect recognition then the response is very much weaker and less immunosuppressive therapy is required to prevent rejection. Ways of modifying the rejection process Patients afflicted with end-stage organ failure are terminally ill or severely disabled, and when the kidneys are involved, face the prospect of regular dialysis for the rest of their lives. The realization that patients in this category can be restored to a healthy and useful life following organ transplantation has stimulated the search for ways of ameliorating the normal allograft response (Table 15. The balance between T cell and antibody-mediated effects varies according to the circumstance. However, the deleterious effect of mismatched grafts has diminished following the addition of ciclosporin to modern immunosuppressive regimens and the urgent need of individual patients and the difficulties of finding perfect matches means that mismatched grafts are often used in renal transplantation. Selection and preparation of the recipient Many patients awaiting renal transplantation develop cytotoxic antibodies reactive with lymphocytes or endothelium following previous transfusion, grafting, pregnancy or infection. Soon after renal transplantation began it was noticed that the strict avoidance of blood transfusion to prevent presensitization increased the chances of graft rejection and a protocol of pregraft exposure to allogeneic blood was introduced in most renal transplant centres (see p. Source and preparation of the graft Most renal allografts are obtained from unrelated cadaveric donors and are often transported considerable distances in order to provide a satisfactory match between donor and recipient. The period of time during which the kidney is not perfused with an oxygenated blood supply (ischaemia time) is critical and should not exceed 45 minutes at 37 C or 24 hours at 4 C. Living related donors are sometimes used in renal transplantation and in this situation it is possible to match entire haplotypes. Living donors are the normal source of bone marrow or haematopoietic stem cells for transplantation and can donate on successive occasions. Purging of bone marrow to remove T lymphocytes is now widely used as a means of reducing the incidence and severity of Monitoring the allograft response Allograft rejection conjures up a dramatic picture of immunological events, which should be eminently suitable to monitoring by the examination of peripheral blood for changes in antibody or lymphocyte characteristics. Many attempts, involving a wide range of antibody and lymphocyte assays, have failed to provide a clinically useful means of distinguishing rejection episodes from other events such as infection, or one that gives sufficient warning to be able to modify the outcome by therapeutic intervention. This is due to the fact that the specific cells and antibodies of interest are mostly preoccupied within the graft and thus not available for peripheral sampling. Fine needle aspiration biopsy enables samples (10 l) of renal grafts to be removed on alternate days without significant damage to the 181 Chapter 15 Transplantation graft. The nature of the cellular infiltrate is a useful guide to the development of rejection and its severity: the presence of T and B cell blasts occurs early in the rejection process, and infiltration with monocytes indicates severe and possibly irreversible change. Otherwise, one is left with the non-immunological observation of graft function, using physical, biochemical, isotopic or electrocardiographic techniques and these changes can be very non-specific. Infertility Hair loss Cystitis Non-specific immunosuppression the potency of the anti-allograft response is such that none of the factors cited thus far is sufficient to achieve graft survival without the administration of drugs, which suppress the immune system non-specifically. In allotransplantation most rejection episodes occur during the first 3 months but a reduced level of immunosuppressive treatment is required indefinitely in most cases. In the early days of renal transplantation, immunosuppression was usually achieved using the antiproliferative drug, azathioprine (in a dose of c. The introduction of ciclosporin a fungal metabolite in the early 1980s had a major impact on graft survival and the combination of low-dose ciclosporin with azathioprine and prednisolone is still used in many centres. It can cause bone marrow aplasia and frequent monitoring of the white cell count is required. Corticosteroids probably have an effect on T-cell function 182 Osteoporosis Avascular bone necrosis Cataracts Myopathy Hypercholesterolaemia Hypertension Hepatotoxicity in addition to their anti-inflammatory effect on phagocytic cells. It does, however, have several important side effects including nephrotoxicity, hirsutism, gum hypertrophy, hypercholesterolaemia, hypertension and hepatotoxicity, most of which are dose-related. It has similar side effects to cyclosporin with the exception of hirsutism and gum hypertrophy. Mycophenolate mofetil is gradually replacing azathioprine in immunosuppressive regimens as it is more effective in preventing acute rejection and is less toxic than azathioprine. It is a more specific and potent inhibitor of T and B cell proliferation due to its inhibition of purine biosynthesis. However, serious infection has been a problem in some patients treated with these preparations and this emphasizes the overall limitation of non-specific immunosuppression. Opportunistic infection is still a major cause of death in most transplantation programmes and emphasizes the need for more sophisticated forms of immunosuppression. The small but significant increase in the incidence of lymphomas and skin tumours is due to impaired immunity to oncogenic viruses. The subject of secondary immunodeficiency is discussed in more detail in Chapter 11. Specific immunosuppression the prospect of inducing antigen-specific immunosuppression at will in the adult animal has been the goal of transplantation immunology since the 1950s when Medawar and his colleagues were able to induce a similar state in neonatal mice. Experiment 2 shows that if cells from strain A mice are inoculated into newborn mice of strain B then the latter animals accept skin grafts derived from strain A throughout their adult life having become specifically tolerant of this histocompatibility type. That the tolerant animals are immunologically normal apart from their specific unresponsiveness to allografts from strain A is demonstrated in experiment 3 in which the natural tendency to reject the strain A graft the animal already bears is restored by the infusion of cells from a strain B animal that has not been pretreated with strain A cells when newborn. Many other attempts have been made to induce immunological tolerance in adult animals and often with considerable success but the means by which graft acceptance has been achieved have not usually been clinically applicable or acceptable. It has been known for many years that the administration of graft-specific antibody can promote graft acceptance although there is always a risk of hyperacute rejection. This phenomenon of antibody-mediated enhancement has been studied extensively and, at one stage, received limited clinical application for renal transplantation.
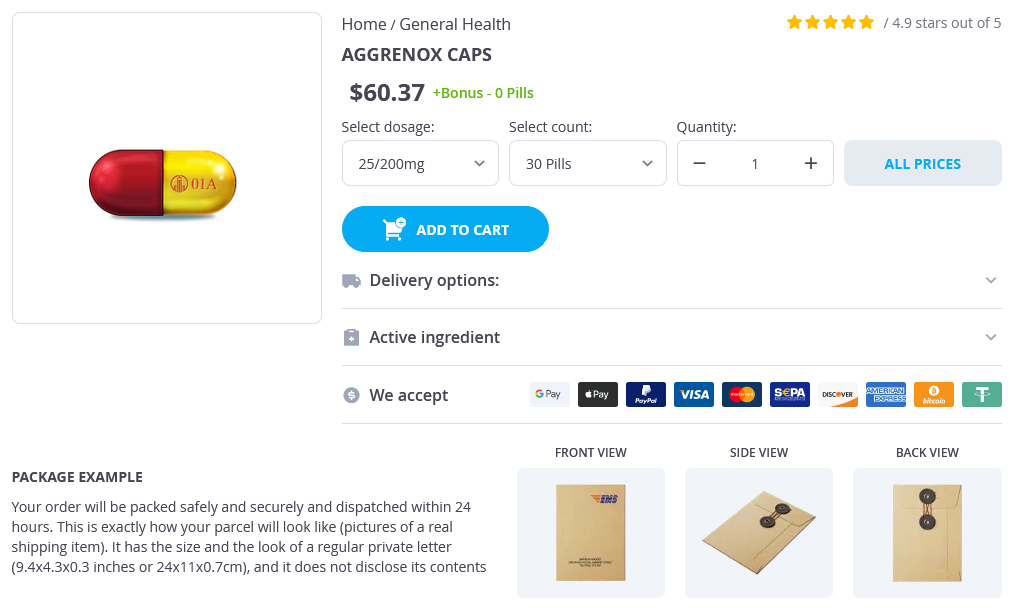
Aggrenox Dosage and Price
Aggrenox caps 25/200mg
- 30 pills - $67.08
- 60 pills - $115.09
- 90 pills - $148.06
- 120 pills - $177.03
- 180 pills - $229.05
The test should be performed once the infant has been established on feeds for a few days treatment of criminals 25/200 mg aggrenox caps purchase amex. Sacral dimples Sacral dimples are a common finding, usually at the base of the spinal column. It is also important to ask about bowel actions and urine excretion and to check the lower limbs for normal movements and power. Assuming the base is easily seen and there are no other abnormalities, simple reassurance is all that is required. The most commonly associated problem is tethering of the spinal cord, which usually presents later in life. Acute haemolytic disease usually presents within the first 2448 hours of life, thus any baby appearing jaundiced within this time must be investigated. The most important reason for treating jaundice is to prevent kernicterus, which is associated with severe unconjugated hyperbilirubinaemia and may result in death or major neurological sequelae. Most infants can be treated with simple phototherapy, although for more serious cases exchange transfusions are needed. As a general rule, any term infant with evidence of jaundice beyond 1014 days of age, or a preterm infant after 3 weeks of age, should be considered as having prolonged jaundice. It is particularly important to exclude a Postpartum complications: neonatal 480 Common neonatal problems conjugated hyperbilirubinaemia, as this may be due to obstruction. The severity varies from mild respiratory symptoms, requiring minimal input, to severe respiratory failure, requiring full intensive care and complex ventilator strategies. Respiratory distress syndrome can either recover or develop into chronic lung disease (bronchopulmonary dysplasia). Other complications include pulmonary interstitial emphysema and other airleak syndromes. Premature infants are at risk of cardiovascular instability and hypotension requiring treatment. They are susceptible to cerebral insults, especially intraventricular haemorrhage and periventricular leukomalacia (the development of cysts in the periventricular areas at a few weeks of age) due to ischaemic injury. They easily become anaemic, due to marrow immaturity, as well as the need for frequent phlebotomy. They often show feed intolerance initially, and there is a high risk of necrotizing enterocolitis. The newborn examination is a clinical screening test, and as such its limitations should be borne in mind. Risk factors for the development of respiratory distress syndrome and transient tachypnoea in newborn infants. Routine examination of the newborn and maternal satisfaction: a randomised controlled trial. System-based approach to management of neonatal jaundice and prevention of kernicterus. It concentrates on common acute problems occurring in the delivery suite shortly after birth and subsequently on common concerns that subsequently present on the postnatal wards. Practical skills · Recognize that reducing perinatal mortality requires practical obstetric skills. Perinatal mortality, however, is strictly defined as stillbirths and deaths of babies in the first week of life. Nevertheless, perinatal mortality includes a wide range of conditions from preterm labour to sudden infant death syndrome with a wide range of underlying causes. Death of a liveborn infant occurring less than 7 completed days (168 hours) from the time of birth. The number of stillbirths and early neonatal deaths (those occurring in the first week of life) per 1000 live and stillbirths. Death in the first year following live birth, on or before the 365th day of life (366th in a leap year). Infant deaths therefore include early and late neonatal deaths and post-neonatal deaths. The dividing line between miscarriage and stillbirth, however, is arbitrary and may vary from country to country. In the United States, for example, there is no single definition used in all states, although guidelines recommend reporting deaths after 20 weeks gestation. When it was lowered to 24 weeks, the official stillbirth rate rose by nearly 30 per cent. The change was made because, with modern neonatal care, many fetuses born alive at under 28 weeks can now survive. In all countries, if a baby is born alive and dies soon after delivery, this is classified as a neonatal death irrespective of the gestation. Although these developments produced a bewildering proliferation of acronyms, the basic aims have not changed. Every year in England, Wales and Northern Ireland, there are over 5000 perinatal deaths, compared with about 100 maternal deaths. Data are cross-checked with registration data from the Office of National Statistics and missing cases are tracked down. One is the Child Health Enquiry, which began in 2004 and examines health outcomes for children aged from 28 days to 18 years. Its first project was a review Ae tiology 483 of child deaths occurring in 2006 and its current study, on head injury, will run until 2012. The underlying reason is often malnutrition, which makes children more susceptible to infection and affects particularly those born into large and poorly spaced families. Perinatal post-mortem examination the enquiry does not depend on post-mortem results.