Aldara
General Information about Aldara
Actinic keratosis is a rough, scaly patch of skin that is usually found on areas of the physique which have been uncovered to the sun, such as the face, scalp, ears, and hands. While most AKs are benign, they have the potential to show into squamous cell carcinoma, a sort of skin cancer. Therefore, it is important to treat AKs to prevent them from progressing into something extra critical. Aldara is a topical cream that's utilized on to the affected space, the place it really works to stimulate the physique's immune response and get rid of abnormal cells.
Aldara, also called imiquimod, is a breakthrough therapy for skin circumstances caused by extreme publicity to the sun. It is an immune response modifier, meaning it actually works by stimulating the body's own immune system to fight off abnormal or cancerous cells on the skin. Aldara is primarily used to treat actinic keratosis (AK) and basal cell carcinoma (BCC), two common forms of skin conditions that may be brought on by overexposure to the sun.
One of the significant advantages of Aldara is its effectiveness in treating pores and skin situations without the necessity for surgery or invasive procedures. This makes it an attractive possibility for those who will not be appropriate candidates for surgical procedure, corresponding to older adults or people with different well being conditions. It is also relatively painless, with minimal side effects similar to redness, itching, and swelling on the web site of software.
In conclusion, Aldara is a exceptional treatment for frequent pores and skin circumstances attributable to overexposure to the sun. It is an immune response modifier that works with the physique's natural defenses to eliminate abnormal or cancerous cells. Its effectiveness and minimal side effects make it a popular alternative for sufferers and medical doctors alike. However, it's important to follow your doctor's instructions carefully and report any uncommon unwanted effects to make sure the safe and efficient use of this treatment. With Aldara, you'll be able to effectively deal with pores and skin circumstances and protect your pores and skin from the dangerous results of the solar.
Aldara is a prescription medication and may only be used beneath the steerage of a healthcare skilled. Before utilizing Aldara, it is important to reveal any medical situations or allergic reactions to your doctor to ensure the safe use of this medication. In most cases, Aldara should be used for about two to six weeks, relying on the severity of the condition being handled. The cream should be applied to the skin 3 times every week, for 8-10 hours every time, after which washed off. It is crucial to follow the instructions provided by your doctor rigorously and not to use roughly than the prescribed quantity.
Furthermore, it's also used to treat basal cell carcinoma in patients who aren't able to have surgical procedure to take away the cancer.
In rare circumstances, Aldara could cause extra severe side effects, corresponding to flu-like signs, blistering, or adjustments in skin shade. If you expertise any of those unwanted effects, it's essential to hunt medical consideration immediately. Pregnant or nursing mothers should not use Aldara without consulting their physician first, as its security for these populations has not been established.
Many individuals could additionally be conversant in basal cell carcinoma, the most typical type of skin cancer. This kind of skin most cancers usually seems as a waxy bump or a scar-like lesion on the pores and skin. It is most frequently discovered on areas which might be exposed to the solar, corresponding to the head, neck, or arms. While BCC is usually not life-threatening, it can trigger disfigurement if left untreated. In instances the place surgical removal of BCC isn't attainable, docs may advocate Aldara as an efficient non-invasive remedy choice.
Furthermore acne refresh 080 5 percent aldara order overnight delivery, where patients were admitted for community acquired pneumonia and treated with ceftriaxone, doxycycline use protected against C. Doxycycline has a lesser potential for staining of teeth and bone than other tetracyclines that have greater avidity for calcium. Teeth staining is due to the formation of tetracycline calcium orthophosphate complexes that darken on exposure to sunlight. Awareness of this complication in nonpermanent dentition is the major reason tetracyclines are infrequently prescribed to children. Recent data indicate that teeth staining does not occur after short courses of doxycycline. Teeth staining is a lesser problem with doxycycline than tetracycline because it binds less avidly to calcium. Discoloration of permanent adult dentition following doxycycline administration may occur, especially in the presence of poor dental hygiene and with marked sunlight exposure (Ayaslioglu et al. Black pigmentation of the thyroid was observed at thyroidectomy in one patient who had been taking doxycycline for a short time preoperatively (Miller et al. In a large survey of 18,515 pregnancies, doxycycline was associated with a small increase in major fetal abnormalities (odds ratio 1. There was no significant increase in fetal abnormalities if doxycycline was taken by the mother during fetal organogenesis (Czeizel and Rockenbauer, 1997). Another study of 1795 doxycycline-exposed pregnancies concluded that there was no increase in the risk of fetal malformations (Rosa, 2002). Animal studies involving mice, monkeys, and rabbits have shown no teratogenic effects of doxycycline (Nahum et al. Photosensitivity Photosensitivity is the second most frequent side effect (after esophageal irritation) related to doxycycline therapy. The photosensitive rash associated with doxycycline therapy consists of erythema in sun-exposed areas, which, if severe, may be associated with edema, papules, vesiculation, and ony- 6d. Hypersensitivity reactions Hypersensitivity reactions are uncommon, and usually take the form of urticaria, asthma, or facial edema. Rare cases of acute anaphylaxis due to tetracyclines other than doxycycline have 1212 Doxycycline occurred (Fellner and Baer, 1965; Furey and Tan, 1969). Two cases of StevensJohnson syndrome due to doxycycline have been reported in the English language medical literature (Cac et al. JarischHerxheimer reactions may occur when doxycycline is used to treat spirochetal infections, such as leptospirosis and Borrelia recurrentis. Hepatotoxicity Doxycycline does not cause the severe hepatitis associated with tetracycline and minocycline usage, as far as presently known. Despite its very low incidence (10 cases reported in the literature) (Friedman, 2005), this side effect comes up frequently in discussions of doxycycline use. Doxycycline-induced intracranial hypertension occurs at any age, without any sex predilection or association with obesity, unlike the nondrug induced idiopathic intracranial hypertension that occurs in obese women. Symptoms of raised intracranial pressure may become apparent between 2 weeks and 1 year after the start of doxycycline therapy (Chiu et al. Management consists of cessation of doxycycline therapy and institution of medical therapy with acetazolamide or other diuretic agent, if intracranial hypertension is persistent. Nosocomial infections Doxycycline may be required for therapy of multiresistant organisms such as Acinetobacter baumanii. Although data are limited, retrospective, and tend to focus on microbiological outcomes, when doxycycline is combined with another antibiotic agent such as colistin, tigecycline, or a beta-lactam (or beta-lactamase inhibitor combination drugs), there are response rates of 4080%, particularly for respiratory tract infections (Falagas et al. However, minocycline and tigecyclin are usually preferred (see Chapter 69, Minocycline, and Chapter 70, Tigecycline). Doxycycline, along with macrolides and quinolones, is concentrated within alveolar macrophages, potentiating its anti-Legionella activity (Cunha, 1991). Use of a loading dose regimen of high dose doxycycline (200 mg twice daily for 72 hours before reverting to 100 mg twice daily) has been suggested for moderate to severe legionellosis (Cunha, 2006; Klein and Cunha, 1998). Azithromycin or respiratory quinolones are now widely used as Legionella treatment because of their superior in vitro activity and long intracellular half-lives. Nonetheless, a combination of penicillin and doxycycline (100 mg twice daily) is appropriate therapy for inpatient treatment of moderately severe community acquired pneumonia with empiric anti-Legionella cover (Mandell et al. Doxycycline is as effective as erythromycin in the treatment of macrolide-susceptible M. Persistent symptoms of bronchitis may occur in some patients, associated with cultures 6f. Effects on immune response In various experimental systems, doxycycline can be shown to alter the two separate arms of the immune system. Doxycycline can depress leukocyte migration (Forsgren and Schmeling, 1977; Belsheim et al. With high concentrations of doxycycline, chemiluminescence and glucose oxidation of polymorphonuclear leukocytes are impaired. The abilities of various human leukocytes to phagocytose yeasts and bacteria are decreased by doxycycline; this effect may be related to an altered surface morphology of polymorphs incubated with tetracyclines (Forsgren and Gnarpe, 1982). Proinflammatory cytokine release is decreased by tetracycline in lipopolysaccharide-challenged mice, protecting against shock in that experimental model (Shapira et al. Doxycycline has been shown to have variable effects on different vaccines given to experimental mice (Woo et al. While some of these same effects could potentially be deleterious in immunosuppressed patients, this has not been apparent in clinical environments to date. Conversely, beneficial immunomodulatory effects are being explored in novel applications that rely on these diverse effects of doxycycline. Indication Randomized controlled trials Non-gonococcal urthethritis Pelvic inflammatory disease Brucellosis Lyme disease Leptospirosis Q-fever endocarditis Malaria prophylaxis Doxy for 1 week equivalent to 1 dose azithromycin, cure C. Doxycycline, along with erythromycin and co-trimoxazole, has been shown to be of benefit in treating acute bronchitis in otherwise well adults.
A smaller dose of 500 mg may suffice for dialysis patients skin care for winter aldara 5 percent purchase, considering that hemodialysis was not an important route of elimination for dalbavancin (Marbury et al. Newborn infants and children To date, there has been a single dalbavancin phase I study in children (Bradley et al. Currently, no dalbavancin dose adjustments are recommended for patients with mild, moderate, or severe hepatic impair ment (Marbury et al. Pharmacokinetic parameters were similar to subjects with normal hepatic function on a 1000mg dose followed by 500 mg 7 days later (Marbury et al. It should be used in pregnancy only if the benefit justifies the potential risk to the fetus. In pregnant rats and rabbits, there were no treatmentrelated malformations or embryofetal toxicity at clinically relevant dalbavancin exposures. It is unknown whether dalbavancin or its metabolite is excreted in human milk (Durata, 2015). The efficacy and tolerability of dalbavancin were similar to comparator regardless of age (Durata, 2015; Dunne et al. Total protein binding of dalbavancin is concentration independent, reversible, and estimated to be 93%. Yet the small free fraction left over is capable of bactericidal activity (Cavaleri et al. The plasma concentra tiontime profile of dalbavancin initially has a steep decline during the 24 to 48hour distribution phase, which slopes down into a slower terminal elimination phase, extending out to 600800 hours (Cavaleri et al. Drug distribution Dalbavancin exhibits linear, doseproportional pharmaco kinetics with a t1/2 of approximately 7 days (Leighton et al. Pharmacokinetic parameters of dalbavancin in healthy volunteers after administration of single and multiple i. A phase I ran domized doubleblind study examined escalating dosages of dalbavancin as a single and multipledose (loading dose and maintenance dose in 10:1 ratio) regimen. Single doses (140, 350, 500, 630, 840, and 1120 mg) were administered once, and multiple doses were given daily for 7 days (300 and 30; 400 and 40; 600 and 60; 800 and 80; and 1000 and 100 mg) with the loading dose administered in equal doses divided by 12 hours. The Cmax of dalbavancin was found to increase in propor tion to the dose, rising from 40. Similar results were seen in the multiple dose group, in which the design of 10:1 ratio for loading dose to maintenance dose generated steady state within 23 days after administration of the first dose. The t1/2 did not change in regard to dose and ranged from 149 to 204 hours, thereby suggesting that onceweekly therapy is suitable. Although its t1/2 is approximately 1 week, it appears that dalbavancin can reside in the body for months after a single dose. In a tissue distribution study in rats, 20 mg/kg of radio active dalbavancin was widely distributed to 40 different this sues and fluids, with the highest concentrations found in the kidney and liver (Cavaleri et al. However, dalbavancin is not exclusively retained by one par ticular tissue, because all tissues experienced a loss of con centration to < 5% of the dose by day 5. By day 14, dalbavancin was still present in kidneys, liver, brown fat, skin, and skeletal muscle at > 1%. At day 70 when the animals were sacrificed, there was still < 5% of dalbavancin remaining in an entire carcass. A dose of 20 mg/kg, which simulated total plasma concentrations in humans, revealed drug concentrations that were three times higher in bone marrow than in plasma at day 3 (12. Pharmacokinetics and pharmacodynamics 923 dalbavancin concentrations in cortical bone 12 hours after a single 1000mg i. This study also suggested that a regimen of 1500 mg given on day 1 and again on day 8 will result in dalbavancin exposure at or above the S. Dalbavancin has moderate penetration into macrophages, where the intracellular concentration increases with growing extracellular concentrations (Bulgheroni et al. In com parison with vancomycin and teicoplanin, dalbavancin has better penetration into these cells, although its intracellular concentration is still considerably lower than oritavancin. Like vancomycin and teicoplanin, dalbavancin is slower in reach ing its bactericidal activity and generally requires 24 hours to achieve the requisite bactericidal kill of 3 logs (Lin et al. Blood samples taken from subjects who received single doses 500 mg or any multiple doses revealed reciprocal serum bactericidal activity titers that increased along with plasma drug concen trations. It appears that drug concentrations 20 mg/l in plasma yield detectable bactericidal titers. It seems that dalbavancin has a high capacity but a low affinity for human plasma proteins. Its high protein capacity is responsible for creating high concentrations of dalbavan cin and for its long t1/2, but the low affinity for protein allows enough unbound dalbavancin to be present to generate bac tericidal activity in vitro. In another timekill study, dalbavancin was determined to be bacterio static (0 to 1. In murine thigh and lung infection models studying multiple doses of dalbavancin (twofold increasing total doses divided into 2, 4, 6, or 12 doses over a period of 6 days), high doses given less fre quently were the most effective regimens in producing the greatest bacterial kill. These findings sug gest that the current human dosing regimen could achieve a 1log kill for S. In population parametric models, the standard dose of dalbavancin demonstrated that the free plasma concentrations of dalbavancin remain above 1 mg/l for 14 days (Dowell et al. A similar finding was demonstrated in a recent study with 10,000 Monte Carlo simulations of dalbavancin, 1000 mg, followed by 500 mg 1 week later. A pharmacokinetic analysis of a single dalbavancin dose (1000 mg if > 60 kg or 15 mg/kg if < 60 kg) in children 1217 years of age demonstrated dose proportionality, with similar t1/2 and plasma exposures between the two doses (Bradley et al. Excretion In a phase I study, nearly 34% of dalbavancin was excreted unchanged in the urine, suggesting that nonrenal methods of elimination play an important role in the metabolism of dalbavancin (Leighton et al.
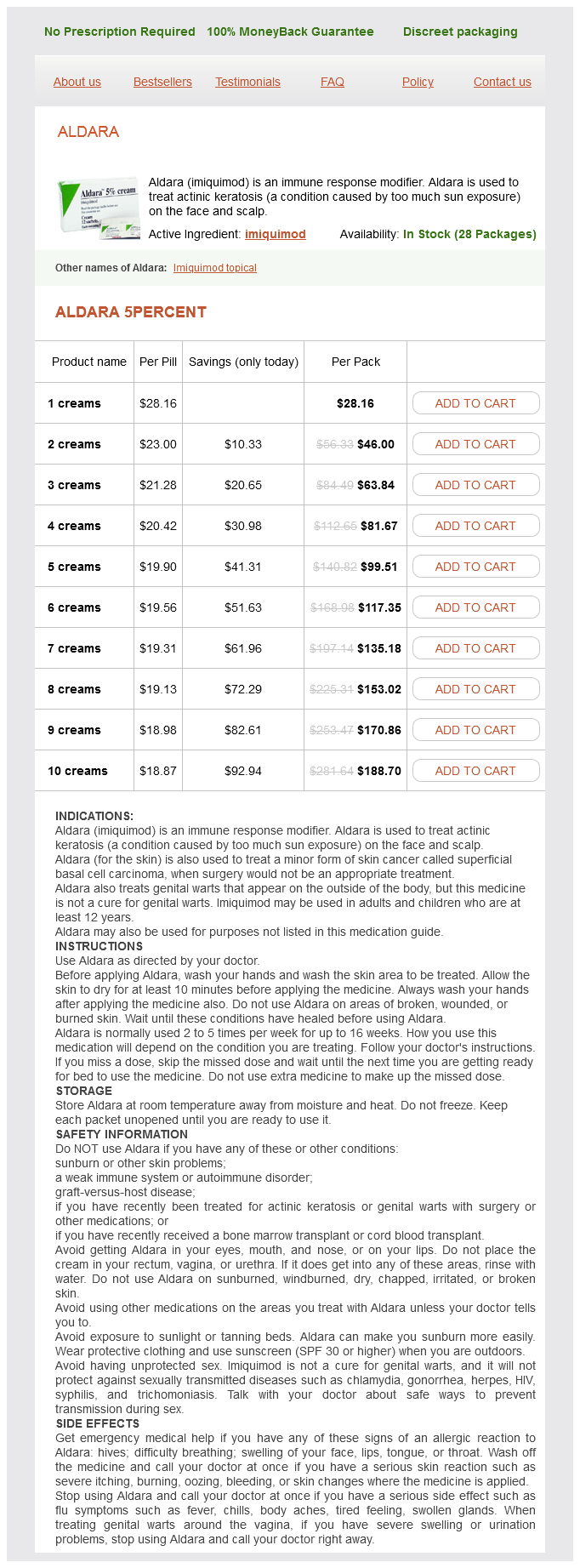
Aldara Dosage and Price
Aldara 5percent
- 1 creams - $28.16
- 2 creams - $46.00
- 3 creams - $63.84
- 4 creams - $81.67
- 5 creams - $99.51
- 6 creams - $117.35
- 7 creams - $135.18
- 8 creams - $153.02
- 9 creams - $170.86
- 10 creams - $188.70
Despite previous descriptions of cardiovascular malformations after clarithromycin exposure in the first trimester and pyloric stenosis after exposure in the third trimester acne gluten purchase aldara 5 percent amex, three large population-based recent studies did not show an increase in cardiovascular malformations or pyloric stenosis after clarithromycin exposure (Bahat Dinur et al. Like erythromycin, clarithromycin has been shown to inhibit contractions of human myometrium independently of dose in in vitro studies (Celik and Ayar, 2002). Hematologic toxicity Leukopenia (white blood cell count < 2 × 109/l) or thrombocytopenia (platelet count < 75 × 109/l) develop in 23% of patients (Price and Tuazon, 1992; Abbott Australasia, 2016). There have also been some case reports of thrombocytopenic purpura developing in patients taking clarithromycin (Oteo et al, 1994; Alexopoulou et al. Other clinical indications for clarithromycin include chlamydiall infections, leprosy, Q fever, and Lyme disease. A comparison of the clinical uses of clarithromycin compared with those of other macrolides is summarized in Table 61. Neurotoxicity Headache occurs in approximately 2% of adults and children (Craft, 1993; Guay et al. Clarithromycin has been associated with transient neurologic effects such as anxiety, confusion, insomnia, psychosis, tremor, dizziness, vertigo, convulsions, and disorientation (Abbott Laboratories, 2000; 7. Potential clinical indications for various macrolides in settings where macrolide susceptibility is likely. Organism or disease Otitis media Pharyngitis Sinusitis Acute infective exacerbation of chronic bronchitis Community-acquired pneumonia Legionella spp. Macrolides have long been considered an alternative to beta-lactams for the treatment of respiratory tract infections. The immediate-release and extended-release formulations of clarithromycin are approved for the treatment of communityacquired respiratory infections, with success rates similar to those of beta-lactams in some studies (Darkes and Perry, 2003). However, the increasing rates of resistance among many respiratory pathogens to macrolides (in particular S. In recent years, macrolides have gained recognition as immunomodulatory agents, particularly in the treatment of bronchiectasis. Large, randomized, controlled trials have shown clinical cure rates of 8194% (McCarty et al. Clarithromycin appears to be as effective as phenoxymethylpenicillin in the eradication of streptococci from the nasopharynx. However, penicillin remains the usual drug of choice in the treatment and prevention of streptococcal infections. Substantial data establishing the efficacy of clarithromycin in preventing the development of rheumatic fever are not available at present. Clarithromycin has been shown to reduce mucus secretion in patients with purulent rhinitis as well as control subjects (Rubin et al. Clinical cure rates of 7994% and radiologic cure rates of 9096% have been shown in clinical trials (Adelglass et al. In a study comparing immediate-release and extended-release formulations of clarithromycin, clinical cure rates were similar (Murray et al. The dosage recommended for this indication is 250 mg immediate-release preparation or 500 mg extended-release preparation twice Clarithromycin has also been shown to be useful in the treatment of otitis media (Aspin et al. A recent meta-analysis showed an increased incidence of treatment failure with macrolides versus amoxicillin with or without clavulanic acid in the treatment of acute otitis media (Courter et al. In addition, the reliance on antibiotic therapies in the treatment of otitis media has been questioned, since the condition is so frequently a result of viral infection. However, the same issues of emerging resistance as described above are also likely to affect its clinical use in this area. For this reason, clarithromycin and other macrolides are proposed as first-line therapy of community-acquired pneumonia only in previously healthy patients with no risk factors for drug-resistant S. As with azithromycin (see Chapter 59, Azithromycin), a combination of clarithromycin with amoxicillin(clavulanate) is recommended in countries with high rates of macrolide-resistant pneumococci when treatment for "atypical" pathogens is required (García Vázquez et al. Doses used are similar: 500 mg orally twice daily for the immediate-release formulation and 1000 mg orally daily for the extendedrelease formulation (Allin et al. Clarithromycin has been shown to have efficacies similar to those of other antibiotics in the treatment of communityacquired pneumonia. A study of dual therapy with clarithromycin and cefuroxime versus clarithromycin alone for treatment of community-acquired pneumonia in outpatient settings did not show the dual therapy as having any additional benefits (Rovira et al. Clarithromycin has greater side effects, particularly gastrointestinal side effects, compared with azithromycin, and hence azithromycin is often preferred (Sopena et al. If hospitalization is required, therapy should consist of azithromycin or another suitable macrolide drug given parenterally (Amsden, 2005). It has been suggested that fluoroquinolones may produce a better response in the treatment of Legionella pneumonia, although in recent studies this superior response has been described as a nonsignificant trend (Griffin et al. Clarithromycin is not recommended for infants less than one month of age, as safety data are unavailable. In particular, it is unknown if, as with erythromycin, clarithromycin is associated with infantile hypertrophic pyloric stenosis. Microbiologic eradication of the pertussis organism was achieved in 100% of cases, with clarithromycin 10 mg/kg daily (maximum 400 mg) given to nine children for 7 days (Aoyama et al. A larger study of 76 children in Canada had similar results, with clarithromycin 7. Skin infections Clarithromycin can be used for noncomplicated skin and skin-structure infections caused by susceptible S. In this context clarithromycin has similar clinical efficacy to that of erythromycin (Northcutt et al. Results of early studies of clarithromycin 250 mg given twice daily compared favor- 7. Clinical uses of the drug 1109 ably with those of cefadroxil 500 mg also given twice daily: 89% versus 92% organism eradication, respectively, and 77% versus 79% clinical cure rates, respectively (Clarithromycin Study Group, 1993).