Azathioprine
General Information about Azathioprine
The immune system is the body's natural defense mechanism in opposition to dangerous substances and foreign invaders. However, in sure situations, the immune system can turn on the body's own tissues, inflicting harm and leading to varied autoimmune issues corresponding to rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel illness. In such circumstances, medication like azathioprine are used to suppress the physique's immune response and prevent further injury.
In conclusion, azathioprine is a crucial treatment for patients with autoimmune disorders and these that have received organ transplants. It works by suppressing the immune system, preventing it from attacking the physique's personal tissues or a transplanted organ. While it's an effective remedy, warning have to be taken concerning its unwanted effects and potential interactions. Proper monitoring and close communication with a health care provider are needed for secure and successful treatment.
Women who are pregnant or planning to turn out to be pregnant should use azathioprine with caution as it may possibly harm the growing fetus. It is essential to debate the risks and advantages with a physician earlier than starting the medicine.
Azathioprine, like most drugs, comes with a listing of possible unwanted facet effects. The most typical side effects embrace nausea, vomiting, lack of appetite, diarrhea, and stomach ache. These side effects are usually gentle and go away with continued use of the treatment. However, in some instances, extra severe side effects similar to liver harm, low blood cell depend, and elevated danger of an infection might happen. Therefore, regular blood tests are essential to observe any potential antagonistic effects.
Azathioprine, also called Imuran, is a powerful medicine that belongs to the group of immunosuppressive agents. It is often used within the therapy of varied autoimmune issues, such as rheumatoid arthritis and to stop rejection in sufferers who've acquired organ transplants.
One of the first makes use of of azathioprine is in preventing organ rejection in sufferers who've undergone organ transplants. When a affected person receives a model new organ, the immune system recognizes it as a international body and attacks it. This can result in rejection of the transplanted organ and could be life-threatening. Azathioprine works by suppressing the exercise of immune cells, preventing them from attacking the transplanted organ.
People with a historical past of liver disease or bone marrow problems is most likely not suitable candidates for azathioprine use. It can be essential to tell the physician about another drugs, dietary supplements, or herbal merchandise being taken to keep away from any potential interactions.
The medicine could be taken orally in the type of tablets or given intravenously in hospital settings. The dosage and length of treatment range relying on the situation being handled and the patient's response. It is essential to follow the prescribed dosage and by no means cease or alter the medication with out consulting a doctor.
Azathioprine is also generally used in the treatment of rheumatoid arthritis, a persistent autoimmune disorder that causes irritation and ache in the joints. It works by reducing the exercise of immune cells that assault and damage the joints. Studies have shown that azathioprine can improve symptoms and slow the progression of rheumatoid arthritis, allowing sufferers to steer a greater high quality of life.
An inner layer spasms right side of body generic 50 mg azathioprine mastercard, called the chondrogenic layer, formed by elongated chondrocytes aligned tangentially to the perichondrium of the cartilage. It provides a hydrated gel-like structure that facilitates the loadbearing properties of cartilage. A lack of Sox9 expression prevents the chondrogenic layer to differentiate into chondrocytes (see Box 4-I). We come back to Sox9 to stress its role of enabling mesenchymal stem cells to become preosteoblasts. Elastic cartilage predominates in the auricle of the external ear, a major portion of the epiglottis and some of the laryngeal cartilages. The specialized matrix of the cartilage has remarkable flexibility and the ability to regain its original shape after deformation. Fibrocartilage has great tensile strength and forms part of the intervertebral disk, pubic symphysis, and sites of insertion of tendon and ligament into bone. The fibrocartilage is sometimes difficult to distinguish from dense regular connective tissue of some regions of tendons and ligaments. Bone · Genes encoding proteins that turn on (activate) or turn off (repress) other genes are called transcription factors. Therefore, mutations affecting genes encoding transcription factor have pleiotropic effects (Greek pleion, more; trope, a turning toward). For example, Sox9 protein is expressed in the gonadal ridges of both genders but is upregulated in males and down-regulated in females before gonadal differentiation. Diaphysis or shaft Periostium Metaphysis Epiphysis Articular surface bone consists of a network of bony spicules or trabeculae delimiting spaces occupied by the bone marrow. In long bones, such as the femur, the shaft or diaphysis consists of compact bone forming a hollow cylinder with a central marrow space, called the medullary or marrow cavity. The ends of the long bones, called epiphyses, consist of spongy bone covered by a thin layer of compact bone. In the growing individual, epiphyses are separated from the diaphysis by a cartilaginous epiphyseal plate, connected to the diaphysis by spongy bone. A tapering transitional region, called the metaphysis, connects the epiphysis and the diaphysis. Both the epiphyseal plate and adjacent spongy bone represent the growth zone, responsible for the increase in length of the growing bone. The articular surfaces, at the ends of the long bones, are covered by hyaline cartilage, the articular cartilage. Except on the articular surfaces and at the insertion sites of tendons and ligaments, most bones are surrounded by the periosteum, a layer of specialized connective tissue with osteogenic potential. The marrow wall of the diaphysis, the endosteum, and the spaces within spongy bone are lined by osteoprogenitor cells, with osteogenic potential. Lamellar or compact bone, typical of the mature bone, displays a regular alignment of collagen fibers. Woven bone, observed in the developing bone, is characterized by an irregular alignment of collagen fibers. This bone is mechanically weak, is formed rapidly and is then replaced by lamellar bone. The lamellar bone consists of lamellae, largely composed of bone matrix, a mineralized substance deposited in layers or lamellae, and osteocytes, each one occupying a cavity or lacuna with radiating and branching canaliculi that penetrate the lamellae of adjacent lacunae. The osteons or haversian systems, formed by concentrically arranged lamellae around a longitudinal vascular channel. The interstitial lamellae, observed between osteons and separated from them by a thin layer known as the cement line. The outer circumferential lamellae, visualized at the external surface of the compact bone under the periosteum. The inner circumferential lamellae, seen on the internal surface subjacent to the endosteum. The vascular channels in compact bone have two orientations with respect to the lamellar structures: 1. Periosteum and endosteum During embryonic and postnatal growth, the periosteum consists of: 1. An inner layer of preosteoblasts (or osteoprogenitor cells), in direct contact with bone. In the adult, the periosteum contains quiescent connective tissue cells that retain their osteogenic potential in case of bone injury and repair. Haversian system or osteon Collagen fibers alternate in helical orientations in successive lamellae of the haversian system. Alternate direction of collagen fibers in successive lamellae of the outer circumferential lamellar system. Haversian system or osteon Inner circumferential lamellar system Spongy bone (also called trabecular or cancellous spongy bone). The cavities of the spongy bone are continuous with the bone marrow cavity of the diaphysis. In the adult, these cells can become osteoblasts during conditions requiring bone repair, such as bone fracture. Haversian canal Ground dry bone Canaliculi, where cytoplasmic processes of osteocytes were housed Concentric lamella Scanning electron micrograph courtesy of Richard G. Kessel, Iowa City, Iowa Lacuna, where an osteocyte resided that penetrate the outer circumferential lamellae. It consists of osteoprogenitor cells, reticular stromal cells of the bone marrow and connective tissue fibers. As discussed in Chapter 6, Blood and Hematopoiesis, preosteoblasts and osteoblasts in the endosteum contribute hematopoietic cytokines to the bone marrow microenvironment, the endosteal niche, essential for hematopoietic stem cell proliferation and maturation. Bone matrix the bone matrix consists of organic (35%) and inorganic (65%) components.
Pepsinogen spasms kidney stones order 50 mg azathioprine visa, a proenzyme stored in the zymogen granules, is released into the lumen of the gland and converted in the acid environment of the stomach to pepsin, a proteolytic enzyme capable of digesting most proteins. Parietal cells predominate near the neck and in the upper segment of the gastric gland and are linked to chief cells by junctional complexes. Parietal cells produce the hydrochloric acid of the gastric juice and intrinsic factor, a glycoprotein that binds to vitamin B12. Vitamin B12 binds in the stomach to the transporting binding protein intrinsic factor. In the small intestine, the vitamin B12intrinsic factor complex binds to intrinsic factor receptor on the surface of enterocytes in the ileum and is transported to the liver through the portal circulation. Destruction of parietal cells causes a reduction in hydrochloric acid in the gastric juice (achlorhydria) and a lack of synthesis of intrinsic factor. The resulting vitamin B12 deficiency disrupts the formation of red blood cells in the bone marrow, Parietal cells produce an acidic secretion (pH 0. The release of H+ ions and Cl by the parietal cell involves the membrane fusion of the tubulovesicular system with the secretory canaliculus. Histamine potentiates the effects of acetylcholine and gastrin on parietal cell secretion after binding to the histamine H2 receptor. Cimetidine is an H2 receptor antagonist that inhibits histaminedependent acid secretion. K+ and Na+ are recycled back into the cell by separate pumps once H+ has taken their place. Pathology: Helicobacter pylori infection the gastric juice is a combination of two separate secretions: 1. An alkaline mucosal gel protective secretion, produced by surface mucous cells and mucous neck cells. The aggressive secretion is facultative because hydrochloric acid and pepsin levels increase above basal levels after food intake. The viscous, highly glycosylated gastric mucus blanket, produced by surface mucous cells and mucous neck cells, maintains a neutral pH at the epithelial cell surfaces of the stomach. However, the mucus blanket lining the gastric epithelium, in particular in the pyloric antrum, is the site where the flagellated bacterium Helicobacter pylori resides in spite of the hostile environment. Its presence has been associated with acid peptic ulcers and adenocarcinoma of the stomach. An active phase, in which motile bacteria increase the gastric pH by producing ammonia through the action of urease. A stationary phase, consisting in the bacterial attachment to fucose-containing receptors on the surface of mucous surface cells of the pyloric region. Both ammonia production and cytotoxic proteases correlate with the development of peptic ulcers of the pyloric mucosa. Intense, sudden, persistent stomach pain (relieved by eating and antacid medications), hematemesis (blood vomit), or melena (tarlike black stool) are clinical symptoms in some patients. Increasing evidence for the infectious origin of acid peptic disease and chronic gastritis led to the implementation of antibiotic therapy for all ulcer patients shown to be infected with H. Helicobacter pylori and chronic gastric inflammation and ulcers 1 Ammonia produced by H. Regeneration of epithelial cells of the gastric mucosa Stem cells are mitotic-dividing cells present adjacent to the neck region of the gastric gland and are responsible for the continuous renewal of the gastric mucosa. Daughter cells derived from the stem cell migrate either upward to replace surface mucous cells, or downward to differentiate into parietal cells, chief cells, and gastroenteroendocrine cells. Surface mucous cells have a life span of about 3 days; parietal and chief cells have a life span of more than 190 days. Partial gastrectomy was carried out because of a bleeding vessel in the base of the ulcer caused hematemesis. Amines are part of polypeptide hormones that can stimulate or inhibit target cell function. Gastrin releasing peptide 3 Postsynaptic neuron To target cell Vagus nerve 4 Vagal stimulation of the pyloric antrum causes the release of gastrin-releasing peptide from postsynaptic neurons that stimulate directly the release of gastrin from G cells present in the antrum. Histamine potentiates the effect of acetylcholine and gastrin on the secretion of hydrochloric acid by parietal cells. The objective is to prevent binding of pathogenic bacteria without interfering with the endogenous bacterial flora by the use of antibiotics. Gastroenteroendocrine cells the function of the alimentary tube is regulated by peptide hormones, produced by gastroenteroendocrine cells, and neuroendocrine mediators, produced by neurons. Peptide hormones are synthesized by gastroenteroendocrine cells dispersed throughout the mucosa 492 15. The population of gastroenteroendocrine cells is so large that the gastrointestinal segment is regarded as the largest endocrine organ in the body. Peptide hormones produced by gastrointestinal endocrine cells have the following general functions: 1. Secretin is released by cells in the duodenal glands of Lieberkühn when the gastric contents enter the duodenum. Three forms of gastrin have been described: little gastrin, or G17 (which contains 17 amino acids), big gastrin, or G34 (which contains 34 amino acids), and minigastrin, or G14 (which consists of 14 amino acids). The neuroendocrine mediator gastrin-releasing peptide regulates the release of gastrin. Gastrin has a trophic effect on the mucosa of the small and large intestine and the fundic region of the stomach.
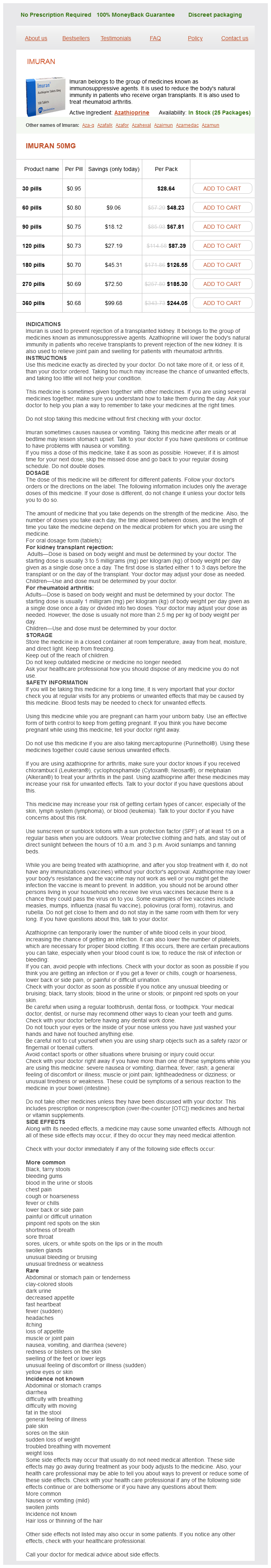
Azathioprine Dosage and Price
Imuran 50mg
- 30 pills - $28.64
- 60 pills - $48.23
- 90 pills - $67.81
- 120 pills - $87.39
- 180 pills - $126.55
- 270 pills - $185.30
- 360 pills - $244.05
Endothelin 1 (vasoconstrictor) Nitric oxide (vasodilator) Smooth muscle cell Interleukin-1 Tumor necrosis factor ligand Vascular lumen E-selectin Carbohydrate ligand Endothelial cells regulate the traffic of inflammatory cells 4 Endothelial cells facilitate transendothelial migration of cells involved in an inflammatory reaction (for example muscle relaxant vitamins generic azathioprine 50 mg buy, neutrophils) in the surrounding extravascular connective tissue. Activated macrophages secrete tumor necrosis factor ligand and interleukin-1, which induce the expression of E-selectin by endothelial cells. Endothelin 1 is a very potent vasoconstrictor peptide produced by endothelial cells. Prostacyclin also prevents platelet adhesion and clumping leading to blood clotting. We discuss later in this chapter how endothelial cell dysfunction can contribute to thrombosis, a mass of clotted blood formed inside a blood vessel due to the activation of the blood coagulation cascade. The endothelium has a passive role in the transcapillary exchange of solvents and solutes by diffusion, filtration, and pinocytosis. The thrombogenic potential of the plaque, resulting from the production of procoagulant tissue factor by macrophages, causes thrombosis leading to the obstruction or occlusion of the arterial lumen. Fibrous cap Atheroma core Extracellular cholesterol Photographs from Damanjov I, Linder J: Pathology: A Color Atlas, St. The endothelial cells at the venous end are more permeable than those at the arterial end. Finally, recall the significance of endothelial cells in the process of cell homing and inflammation. Pathology: Atherosclerosis Atherosclerosis is the thickening and hardening of the walls of arteries caused by atherosclerotic plaques of lipids, cells, and connective tissue deposited in the tunica intima. Atherosclerosis is frequently seen in arteries sustaining high blood pressure, it does not affect veins and is the cause of myocardial infarction, stroke, and ischemic gangrene. Atherosclerosis is a chronic inflammatory disease driven by the accumulation of cholesterol-laden macrophages in the artery wall. The atheroma core continues to enlarge and smooth muscle cells of the tunica muscularis migrate to the intima forming a collagencontaining fibrous cap overlying the atheroma core. An enlarging thrombus will eventually obstruct or occlude the lumen of the affected blood vessel. As you can see, the clearance of lipoproteins by macrophages appears initially beneficial but, with time, the macrophage function is compromised and starts to contribute to the inflammatory response through the secretion of pro-inflammatory mediators and extracellular matrix proteases. With time, dying macrophages release their lipid contents, which leads to the enlargement of the atheroma core. The major blood vessels involved are the abdominal aorta and the coronary and cerebral arteries. Coronary arteriosclerosis causes ischemic heart disease and myocardial infarction occurs when the arterial lesions are complicated by thrombosis. Atherothrombosis of the cerebral vessels is the major cause of brain infarct, so-called stroke, one of the most common causes of neurologic disease. Arteriosclerosis of the abdominal aorta leads to abdominal aortic aneurysm, a dilation that sometimes ruptures to produce massive fatal hemorrhage. A genetic defect in lipoprotein metabolism (familial hyper-cholesterolemia) is associated with atherosclerosis and myocardial infarction before patients reach 20 years of age. Pathology: Vasculogenesis and angiogenesis After birth, angiogenesis contributes to organ growth. Proliferation in the dermis of jagged thin walled vascular channels lined by endothelial cells. Angiogenesis Vasculogenesis (from angioblasts in the embryo) In the embryo, blood vessels provide the necessary oxygen, nutrients, and trophic signals for organ morphgogenesis. Development of an endothelial capillary tube Angioblasts (endothelial cell precursors) proliferate and form endothelial capillary tubes. Neovascularization during pathologic conditions Basal lamina 5 Tie2 receptor (a receptor Angiopoietins (Ang1 and Ang2) tyrosine kinase) the formation of a blood vessel from a preexisting vessel, a process known as neovascularization, is relevant to chronic inflammation, development of collateral circulation, and tumor growth. Ang2, another angiopoietin, interacts with Tie2 to induce the loss of contact of endothelial cells with the extracellular matrix. The role of Ang2 in tumor angiogenesis is emerging as a target for cancer treatment. Smooth muscle cell Vascular smooth muscle layer Mature blood vessel In the adult, most blood vessels remain stable and angiogenesis occurs in the endometrium and ovaries during the menstrual cycle, and in the placenta during pregnancy. Under pathologic conditions, angiogenesis is excessive during malignant (see Box 12-C), ocular (age-related macular degeneration), and inflammatory conditions. An understanding of vasculogenesis and angiogenesis is relevant to developing therapeutic strategies to produce revascularization of ischemic tissues or inhibit angiogenesis in cancer, ocular, joint, or skin disorders. Vasculogenesis, a process initiated by the coalescence of free and migratory vascular endothelial progenitors, or angioblasts, during embryogenesis to form a primitive vascular network in the yolk sac and trunk axial vessels. Angiogenesis, a process initiated in a preexisting vessel and observed in the embryo and adult. However, although tumor antiangiogenic targeted drugs inhibit primary tumor growth, they promote tumor invasion and metastasis. The mechanism of tumor hypoxia, caused by oxygen deprivation resulting from blocking tumor angiogenesis, could explain the selective switch of tumor cells into an invasive and metastatic program. Hypoxia generated by tumor angiogenesis inhibition triggers pathways that make tumor cells aggressive and metastatic. The phosphorylated receptor interacts with a variety of cytoplasmic signaling molecules leading to angiogenesis involving the proliferation and differentiation of endothelial cells. We discuss below that tumor angiogenesis is a specific form of angiogenesis with important clinical implications. Endothelial cells migrate, proliferate, and assemble into tubes to contain the blood. Periendothelial cells (smooth muscle cells, pericytes, and fibroblasts) are recruited to surround the newly formed endothelial tubes. Tie2, a receptor tyrosine kinase that modulates a signaling cascade required for the induction or inhibition of endothelial cell proliferation.