Baclofen
General Information about Baclofen
While baclofen can present vital benefits in the therapy of muscular problems, it's essential to comply with the prescribed dosage and directions carefully. It is finest to begin with a low dose and progressively increase it to realize the specified impact, as this medication can have some unwanted effects, together with dizziness, drowsiness, and weakness. It is advisable to speak with a health care provider if the unwanted aspect effects persist or turn out to be severe.
In addition to treating muscle spasms and clonus, baclofen can be beneficial in managing muscle cramping. This is commonly skilled by people with conditions corresponding to multiple sclerosis or spinal wire accidents. Muscle cramps can be painful and have an result on every day actions, however baclofen has been discovered to supply reduction by enjoyable the affected muscle tissue.
Rigidity of muscles, which is the shortcoming to chill out or loosen muscle tissue, is another situation that's handled with baclofen. This can happen as a result of circumstances like Parkinson's illness, ALS (Lou Gehrig's disease), or cerebral palsy. Baclofen helps to chill out the muscle tissue, reducing rigidity and enhancing movement and suppleness.
Aside from its use in treating muscular disorders, baclofen has also been found to be effective in managing pain caused by situations such as a number of sclerosis and spinal twine injuries. This treatment works by targeting the nerve indicators that transmit ache, providing reduction to those affected by chronic ache.
Baclofen falls underneath the category of muscle relaxants, which work by reducing the activity of the muscular tissues. It is a GABA mimetic drug, which signifies that it acts on the neurotransmitter GABA (gamma-aminobutyric acid) in the mind and spinal cord, inhibiting nerve indicators that trigger muscle spasms.
In conclusion, baclofen is a priceless treatment that has proven to be effective in treating various muscular problems corresponding to spasm, clonus, cramping, rigidity, and pain. It provides aid to individuals suffering from these situations, bettering their total quality of life. If you or a liked one is experiencing any of those symptoms, it is recommended to seek the advice of a physician to see if baclofen could additionally be an acceptable remedy option.
Another common use of this medicine is for muscle clonus, which is a situation characterized by involuntary and fast muscle contractions. Baclofen has shown to be effective in reducing these spasms and enhancing muscle control. It also helps to lower the frequency and depth of the muscle contractions, making actions easier for these with this situation.
Baclofen is a drugs that has been proven to be a useful software within the treatment of various muscular issues. Often prescribed by doctors, it is commonly used to deal with muscle spasm, cramping, and rigidity of the skeletal muscular tissues. This treatment has also shown promising leads to treating pain caused by issues corresponding to a quantity of sclerosis and spinal twine injuries.
One of the first makes use of of baclofen is the remedy of spasm of skeletal muscle tissue. This can happen because of various reasons, including neurological problems, spinal cord injuries, or ailments like a quantity of sclerosis. These spasms can be not solely uncomfortable but additionally debilitating, making it difficult for people to hold out their every day activities. Baclofen helps to loosen up the muscle tissue, providing relief from these spasms and enhancing the quality of life for those suffering from these circumstances.
It is more common in Caucasians with an incidence estimated to be 1525 per 100 000 individuals older than 50 years of age44; however muscle relaxant education baclofen 25 mg for sale, an increasing incidence in other races has been reported. The most common presenting symptom is a new headache in an older adult, but a variety of other findings can lead to the diagnosis. Clinical features of temporal arteritis include pulselessness, nodularity or tenderness of the temporal artery, scalp tenderness or necrosis, jaw claudication, fever, anorexia, weight loss, malaise, and polymyalgia rheumatica. Although oral prednisone at an initial dose of 12 mg/kg is commonly used, intravenous administration of steroids is often considered when amaurosis or vision loss has already occurred in one or both eyes. The goal of steroid administration is to try to prevent additional loss of vision. However, it is possible for vision loss to progress despite prompt administration of steroids. Steroid treatment should be initiated promptly upon first suspicion of temporal arteritis because progressive vision loss due to infarction can occur within days or weeks after the initial visual symptoms. When temporal arteritis is suspected as the cause of visual loss, treatment should not be delayed for results of laboratory investigations or biopsy. Histopathological signs of inflammation in the temporal artery biopsy can persist for weeks after initiation of steroid treatment. Symptomatic response to steroids, excluding vision, may be dramatic within 24 h, with relief of headache and malaise. In diabetic patients or patients intolerant to the side effects of steroids, other immunosuppressive drugs, such as methotrexate, can be used in conjunction with or as an alternative to steroids. Patients with visual loss from temporal arteritis must be co-managed with an internist or rheumatologist. It is characterized by an ischemic loss of vision due to optic neuropathy in the absence of optic disk edema. The mechanism of ischemia is presumed to be insufficiency of pial arterial vascular supply to the optic nerve distal to the optic nerve head. The usual presentation is sudden, painless unilateral or bilateral vision loss with a relative afferent pupillary defect in unilateral cases as well as in bilateral cases when the degree of vision loss is unequal between the two eyes. Does optic disc appearance distinguish ischemic optic neuropathy from optic neuritis Roth S, Thisted R, Erickson J, et al: Eye injuries after nonocular surgery: a study of 60,965 anesthetics from 1988 to1992. Purvin V, King R, Kawasaki A, Yee R: Anterior ischemic optic neuropathy in eyes with optic disc drusen. Egan Not infrequently, the ophthalmologist is called on to determine whether or not visual loss is caused by infiltrative or compressive lesions of the anterior visual pathway. This is determined through careful clinical evaluation of the visual acuity, color vision, pupils, visual fields, and fundus. Knowledge of the more common tumors will assist the ophthalmologist in advising patients on a course of action, and deciding which patients should be followed and which require referral to neurosurgeons or radiation oncologists. This article focuses on the two most common types of orbital masses that affect the optic nerve: the optic nerve glioma and the optic nerve sheath meningioma. At this point, the exact mechanism of action of development of these tumors is unknown. An ipsilateral relative afferent pupillary defect is present (unless bilateral), visual acuity is deficient, and there is achromatopsia. However, some tumors are more aggressive, resulting in a rapid increase in ipsilateral proptosis and visual loss. When this occurs, the peripheral tumor cells may resemble those in an optic nerve sheath meningioma and render an incorrect diagnosis unless a deeper specimen is examined. Therefore, in those rare cases in which a biopsy is considered appropriate and vision is irrevocably lost, resection might be performed. The globe need not be enucleated since the eye typically will not become phthisical. When tumors affect the chiasm, chemotherapy should be considered, although this mode of therapy is not necessarily curative. The overall histologic appearance is benign, with a paucity of cellular atypia, mitosis, or tumor necrosis. Often, microcystoid extracellular spaces containing acid mucopolysaccharide produced by astrocytes are encountered. In the glioma of one 4-year-old boy, malignant degeneration of the distal portion of the tumor was encountered in an otherwise typical optic nerve glioma. There is increased T2 signal surrounding the nerve that pathologically is arachnoidal gliomatosis. En bloc resection of intraorbital optic nerve glioma demonstrates fusiform enlargement of the optic nerve without disruption of the dural sheath. The nerve is seen to undulate up and out of the view of the slice and then back into view again. The glioma involves only the orbital segment of the nerve and is confined by the dura. Careful attention to the pituitary axis must be taken since many patients who undergo radiation treatment develop endocrine dysfunction. Gangliogliomas may also present with vision loss when they compress the optic nerve44 or originate within the substance of the optic nerve. The primary variety arises from the cap cells of the intraorbital or intracanalicular optic nerve sheath while the secondary form arises intracranially in the region of the sphenoid wing, tuberculum sella, or olfactory groove. Eye pain or headache may accompany the visual loss and blindness occurs within weeks of onset.
Bernstein E muscle relaxant drug test order 25 mg baclofen with amex, Dilley R: Late results after carotid endarterectomy for amaurosis fugax. Moore W, Boren C, Malone J, et al: Natural history of nonstenotic aymptomatic ulcerative lesions of the carotid artery. Dixon S, Pais O, Raviola C, et al: Natural history of nonstenotic, asymptomatic ulcerative lesions of the carotid artery. Chikos P, Fisher L, Hirsch J, et al: Observer variability in evaluating extracranial carotid artery stenosis. Mouradian M, Wijmann C, Tomasian D, et al: Echocardiographic findings of patients with retinal ischemia or embolism. Di Tullio M, Sacco R, Gersony D, et al: Aortic atheromas and acute ischemic stroke: a transesophageal echocardiographic study in an ethnically mixed population. Romano J, Babikian V, Wijman C, Hedges T: Retinal ischemia in aortic arch atheromatous disease. Werner M, Burger P, Heinz E, et al: Intracranial atherosclerosis following radiotherapy. Huang Y, Gad S, Li S, et al: Vascular lesions in Chinese patients with transient ischemic attacks. Benavente O, Eliasziw M, Streifler J, et al: Prognosis after transient monocular blindness associated with carotid-artery stenosis. Wijman C, Gomes J, Winter M, et al: Symptomatic and asymptomatic retinal embolism have different mechanisms. Nutio K, Lindsberg P, Carpen O, et al: Adhesion molecule expression in symptomatic and asymptomatic carotid stenosis. Streifler J, Eliasziw M, Benavente O, et al: the risk of stroke in patients with first-ever retinal vs hemispheric transient ishcemic attacks and high-grade carotid stenosis. Wilterdink J, Easton J: Vascular event rates in patients with atherosclerotic cerebrovascular disease. Rokey R, Rolak L, Harati Y, et al: Coronary artery disease in patients with cerebrovascular disease: a prospective study. Pfaffenbach D, Hollenhorst R: Morbidity and survivorship of patients with embolic cholesterol crystallization in the ocular fundus. The effect of lowdose warfarin on the risk of stroke in patients with non-rheumatic atrial fibrillation. Hobsob R, Weiss D, Fields W, et al: Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. Taylor D, Barnett H, Haynes R, et al: Lowdose and high-dose acetylsalicylic acid for patients undergoing carotid endarterectomy: a randomised controlled trial. Rothwell P, Eliasziw M, Gutnikov S, et al: Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Wilson S, Mayberg M, Yatsu F, et al: Crescendo transient ischemic attacks: a surgical imperative. Ferguson G, Eliasziw M, Barr H, et al: the North American Symptomatic Carotid Endarterectomy Trial: surgical results in 1415 patients. Winslow C, Solomon D, Chassin M, et al: the appropriateness of carotid endarterectomy. Report of the American Academy of Neurology T, and Technology Assessment Subcommittee: Interim assessment: carotid endarterectomy. Rossouw J, Lewis B, Rifkind B, et al: the value of lowering cholesterol after myocardial infarction. Yatsu F, Fisher C: Atherosclerosis: current concepts on pathogenesis and interventional therapies. Caplan L, Meyers P, Schumacher H: Angioplasty and stenting to treat occlusive vascular disease. Cao P, De Rango P, Verzini F, et al: Outcome of carotid stenting versus endarterectomy: a case-control study. Wilentz J, Chati Z, Krafft V, Amor M: Retinal embolization during carotid angioplasty and stenting: mechanisms and role of cerebral protection systems. A multidisciplinary consensus statement from the ad hoc Committee, American Heart Association. Andaluz N, Zuccarello M: Place of drug therapy in the treatment of carotid stenosis. Bornstein N, Kareprov V, Aronovich B, et al: Failure of aspirin treatment after stroke. Helgason C, Tortorice K, Winkler S, et al: Aspirin response and failure in cerebral infarction. Hass W, Easton J, Adams H, et al: A randomized trial comparing ticlopidine hydrochloride with aspirin for the prevention of stroke in high-risk patients. Skalen K, Gustafsson M, Rydberg E, et al: Subendothelial retention of atherogenic 68. Tzourio C, Anderson C, Chapman N, et al: Effects of blood pressure lowering with peridopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Von Graefe A: Ueber Embolie der arteria centralis retinae als Ursache plotzlicher Erblindung. Hayreh S, Kolder H, Weingeist T: Central retinal artery occlusion and retinal tolerance time.
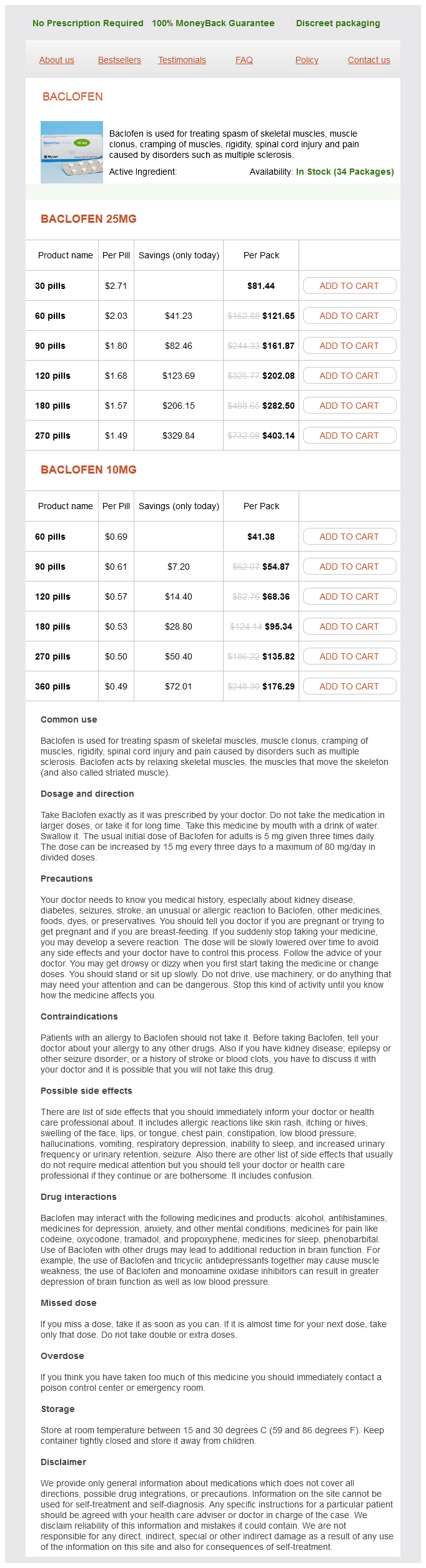
Baclofen Dosage and Price
Baclofen 25mg
- 30 pills - $81.44
- 60 pills - $121.65
- 90 pills - $161.87
- 120 pills - $202.08
- 180 pills - $282.50
- 270 pills - $403.14
Baclofen 10mg
- 60 pills - $41.38
- 90 pills - $54.87
- 120 pills - $68.36
- 180 pills - $95.34
- 270 pills - $135.82
- 360 pills - $176.29
Faerman I muscle spasms 9 weeks pregnant purchase baclofen online pills, Faccio E, Milei J, et al: Autonomic neuropathy and painless myocardial infarction in diabetic patients: histologic evidence of their relationship. Gaede P, Vedel P, Larsen N, et al: Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. Bolli G, DeFeo P, Campugnucci P, et al: Abnormal glucose counterregulation in insulin-dependent diabetes mellitus: interactin of anti-insulin antibodies and impaired glucagons secretion. Reaven G, Dray J: Effect of chlorpropamide on serum glucose and immunoreactive insulin concentrations in patients with maturity-onset diabetes mellitus. Stumvoll M, Nurjhan N, Perriello G, et al: Metabolic effects of metformin in noninsulin dependent diabetes mellitus. Aranoff S, Rosenblatt S, Braithwaite S, et al: Pioglitazone hydrocholoride monotherapy improves glycemic control in the treatment of patients with type 2 diabetes. Yang W-S, Jeng C-Y, Wu T-J, et al: Synthetic peroxisome proliferatorsactivated receptor-g agonists, rosiglitazone, increases plasma levels of adiponectin in type 2 diabetic patients. Imano E, Kanada T, Naktani Y, et al: Effect of troglitazone on microalbuminuria in patients with incipient diabetic nephropathy. Mu J, Woods J, Zhou Y-P, et al: Chronic inhibition of dipeptidyl peptidase-4 with a sitagliptin analog preserves pancreatic b-cell mass and function in a rodent model of type 2 diabetes. Raz I, Hanefeld M, Xu L, et al: Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy in patients with type 2 diabetes mellitus. The Kroc Collaborative Study Group: Diabetic retinopathy after two years of intensified insulin treatment: Follow-up of the Kroc Collaborative Study. Chronic uveitis is often asymptomatic in children, producing insidious, "silent," progressive loss of vision and eventual damage to retina, optic nerve, ciliary body, and/or outflow structures that can result in blindness. A thorough history (with special emphasis on comprehensive review of systems), slit-lamp examination, dilated ophthalmoscopic examination, medical evaluation, and appropriate ancillary laboratory testing are indicated in every case of pediatric uveitis. In addition, we suggest that the reader review Chapter 92 for a detailed overview of our philosophy about the diagnosis and treatment of uveitis in general. The coexistence of uveitis and arthritis in childhood does not provide a specific diagnosis, and yet the potential morbidity and mortality resulting from uveitis, joint destruction, and systemic lesions underscore the need for precise diagnosis. Three major subtypes described by the American College of Rheumatology are shown in Table 322. Relative frequencies of these diseases are derived from large series reported by Kanski and Shun-Shin,4 Kanski,7 and Giles. Smaller series and case reports of entities that may present as anterior uveitis are also included in Table 322. The estimated prevalence is 113 per 100 000, with an incidence of 14 cases per 100 000 in the United States per year. Only 66% of the patients were employed, and clinical depression was common, in direct proportion to the degree of disability. Because the likelihood of developing uveitis is different for each of these subtypes, recognition of each and the implications for slit-lamp biomicroscopic screening frequency is of substantial importance to the ophthalmologist. The systemic disease is characterized by symmetric polyarthritis with associated fever, rash, leukocytosis, lymphadenopathy, and hepatomegaly. Pericarditis, pleuritis, splenomegaly, and abdominal pain are less frequently observed. If uveitis is detected at any point, of course, the monitoring becomes much more frequent. The small joints of the hand are characteristically inflamed, although larger joints of the wrist, ankle, or knee may also become involved. Therefore, vision testing and slit lamp biomicroscopy are indicated for this subgroup of patients three times a year for 7 years. Advanced stages of uveitis at presentation are correlated with increased severity of visual loss and higher rates of ocular complications. It is chronic; 60% of cases have a relapsing and remitting course, 20% have an unremitting chronic course, and 20% have a single episode of uveitis. Anterior chamber cells and flare are typical, of course, as are cells in the anterior vitreous. The cellular reaction fluctuates; flare becomes chronic, eventually, as a result of vascular damage and generally should not be used as an indicator of inflammatory activity or need for treatment. No temporal relationship exists between joint inflammation and exacerbations of uveitis. Chronic or recurrent uveitis (even lowgrade, 1+ uveitis) eventually causes the vision-robbing complications of cataract, glaucoma, hypotony, vitreal organization, optic neuropathy, and/or macular edema. Difficulties in diagnosis make the actual incidence and prevalence of juvenile spondylitis hard to determine. A pauciarticular pattern is observed in ~74%, with 20% having a polyarticular presentation and 6% showing a systemic onset. Presentation with back pain, characteristically of the lumbosacral spine or sacroiliac joints, along with cervical or thoracic spinal arthritis (6780%) 2. Presentation with asymmetric peripheral pauciarticular inflammation that involves the hips, knees, ankles, or heels (2030%) 3. Presentation with acute anterior uveitis (23%) this research team described 22 children with ankylosing spondylitis whom they observed for 20 years. Sacroiliac radiographic abnormalities were not visible within the first year of diagnosis in three-fourths of these patients. Initial presentation with inflammation in a lower limb peripheral joint may be consistent with subsequent development of juvenile spondyloarthropathy. Juvenile inflammatory bowel disease-associated arthritis Arthritis associated with inflammatory bowel disease is infrequent in children.