Bactroban
General Information about Bactroban
In conclusion, Bactroban is an efficient remedy for various skin infections brought on by micro organism. It is essential to observe the prescribed dosage and instructions, and to report any unwanted side effects to the doctor. With proper use, Bactroban may help clear up pores and skin infections and prevent them from spreading or recurring.
Bactroban shouldn't be used on open wounds or damaged pores and skin, as this will likely enhance the danger of absorption and potential adverse effects. It is also not beneficial to be used on mucous membranes, corresponding to the inside of the nose or mouth. If the infection does not enhance inside three to five days of utilizing Bactroban, the doctor should be notified because the bacteria may be resistant to the medication.
Bactroban, also called mupirocin, is a prescription medication primarily used for treating skin infections brought on by micro organism. It belongs to a class of antibiotics called topical antibiotics, which are utilized directly to the pores and skin. Bactroban is out there within the type of a cream, ointment, or nasal ointment.
As with any antibiotic, it may be very important full the complete course of treatment, even when signs enhance. Stopping the treatment too soon could lead to a recurrence of the infection and can increase the risk of antibiotic resistance.
Aside from impetigo, Bactroban may also be used to deal with different types of pores and skin infections corresponding to folliculitis, an infection of the hair follicles, and folliculitis barbae, an infection of the hair follicles on the face and neck. It is also effective in opposition to methicillin-resistant Staphylococcus aureus (MRSA), a kind of micro organism that is immune to many frequent antibiotics.
When utilizing Bactroban, it is necessary to observe the instructions supplied by the doctor or pharmacist. It must be applied solely to the affected area of the pores and skin and shouldn't be ingested. It is often beneficial to apply a skinny layer of the cream or ointment to the affected area 3 times a day for ten days, or as prescribed by the doctor.
This medicine is usually used for treating impetigo, a highly contagious skin infection commonly seen in young kids. Impetigo is characterized by pink sores on the face, particularly across the mouth and nose, and can also happen on different elements of the physique. Bactroban works by killing the bacteria that cause impetigo, permitting the skin to heal and stopping further spread of the an infection.
Bactroban is generally well-tolerated, but like all treatment, it might trigger side effects in some people. Common unwanted effects embrace burning, stinging, or itching on the site of software. These unwanted effects are usually gentle and go away on their own. In uncommon cases, people could expertise extreme allergic reactions, together with rash, itching, swelling, and issue respiratory. If these symptoms happen, medical consideration ought to be sought instantly.
The potential for serious consequences from misinterpreting normal responses to the rapid adrenocorticotropin test acne reviews bactroban 5 gm with mastercard. The low dose (1 µg) adrenocorticotropin stimulation test in the evaluation of patients with suspected central adrenal insufficiency. Adrenocorticotropin stimulation test: effects of basal cortisol level, time of day, and suggested new sensitive low dose test. The corticotropin-releasing hormone stimulation test: a possible aid in the evaluation of patients with adrenal insufficiency. Corticotropin releasing hormone: relevance to normal physiology and to the pathophysiology and differential diagnosis of hypercortisolism and adrenal insufficiency. Comparison of the low dose short Synacthen test (1 µg), the conventional dose short Synacthen test (250 µg), and the insulin tolerance test for assessment of the hypothalamic-pituitary-adrenal axis in patients with pituitary disease. Optimizing the diagnostic criteria for standard (250-microg) and low dose (1-microg) adrenocorticotropin tests in the assessment of adrenal function. Comparison of low and high dose corticotropin stimulation tests in patients with pituitary disease. Stimulation of angiotensinogen production in primary cultures of rat hepatocytes by glucocorticoid, cyclic adenosine 3,5-monophosphate, and interleukin-6. Effect of glucocorticoids replacement therapy on bone mineral density in patients with Addison disease. Dehydroepiandrosterone replacement in women with adrenal insufficiency: effects on body composition, serum leptin, bone turnover, and exercise capacity. Glucocorticoid treatment in patients with septic shock: effects on vasopressor use and mortality. Corticosteroids block binding of chemotactic peptide to its receptor on granulocytes and cause disaggregation of granulocyte aggregates in vitro. Influence of corticosteroids on human polymorphonuclear leukocyte function in vitro: reduction of lysosomal enzyme release and superoxide production. Anti-inflammatory steroids induce biosynthesis of a phospholipase A2 inhibitor which prevents prostaglandin generation. Corticosteroid treatment for sepsis: a critical appraisal and meta-analysis of the literature. A controlled trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. Detrimental effects of high-dose methylprednisolone sodium succinate on serum concentrations of hepatic and renal function indicators in severe sepsis and septic shock. Low-dose hydrocortisone infusion attenuates the systemic inflammatory response syndrome. Stress doses of hydrocortisone reverse hyperdynamic septic shock: a prospective, randomized, double-blind, single-center study. Plasma cortisol levels before and during "low-dose" hydrocortisone therapy and their relationship to hemodynamic improvement in patients with septic shock. Immunologic and hemodynamic effects of "low-dose" hydrocortisone in septic shock: a double-blind, randomized, placebo-controlled, crossover study. Adjunctive dexamethasone in bacterial meningitis: a meta-analysis of individual patient data. Their presentation is usually dramatic and is often precipitated by a nonthyroidal-related illness or event. Recognition of these disorders requires a high degree of clinical suspicion because thyroid function abnormalities, as well as other biochemical parameters, do not differ significantly from uncomplicated thyrotoxicosis and hypothyroidism. As thyroid storm and myxedema coma are clinical diagnoses, measurement of serum thyroid hormones serve as confirmatory tests in the appropriate setting. In contrast to these dramatic clinical presentations, critical illness also causes multiple nonspecific alterations in thyroid hormone concentrations in patients without intrinsic thyroid dysfunction that relate to the severity of the illness. Since a wide variety of illnesses tend to result in the same changes in serum thyroid hormones, such alterations in thyroid hormone indices have been termed the sick euthyroid syndrome or nonthyroidal illness. This chapter will review normal thyroid physiology, changes in thyroid hormone metabolism seen with critical illness, and the evaluation of thyroid function in critically ill patients. Finally, diagnosis and management of sick euthyroid syndrome, thyroid storm, and myxedema coma will be reviewed. Thyroxine (T4, 65% iodine by weight) is the principal secretory product of the thyroid gland, comprising about 90% of secreted thyroid hormone under normal conditions. D2 is found primarily in the brain, pituitary, and skeletal muscle and is downregulated in hyperthyroidism and upregulated in hypothyroidism. D3 is expressed primarily in the brain, skin, and placental and chorionic membranes. The actions of D3 also include inactivation of T3 to form T2, another inactive metabolite. Under normal conditions, about 41% of T4 is converted to T3, about 38% is converted to rT3, and about 21% is metabolized via other pathways, such as conjugation in the liver and excretion in the bile. Serum levels of T3 are approximately 100-fold less than those of T4, and like T4, T3 is metabolized by deiodination to form diiodothyronine (T2) and by conjugation in the liver. Other serum binding proteins include transthyretin,6 which binds about 15% of T4 but little, if any, T3, and albumin, which has a low affinity, but a very large binding capacity, for T4 and T3. Role of Free Hormone Essential to an understanding of the regulation of thyroid function and the alterations of circulating thyroid hormones seen in critical illness is the "free hormone" concept, which is that only the unbound hormone has metabolic activity.
Their final recommendation was to proceed with active management of the third stage of labor with controlled cord traction until the placenta is removed skin care companies discount bactroban uk. Oxytocin can be given either before or after placental delivery to facilitate uterine contractions. Emergency postpartum hysterectomy for uncontrolled postpartum bleeding: a systematic review. The objective of this review was to describe factors leading to and outcomes after emergency postpartum hysterectomy for uncontrolled postpartum hemorrhage. Twenty-four articles that included 981 cases of emergency postpartum hysterectomy were reviewed. Their findings showed that women at highest risk of emergency hysterectomy are those who are multiparous, had a cesarean delivery in either a previous or the present pregnancy, or had abnormal placentation. A randomized controlled trial comparing oxytocin administration before and after placental delivery in the prevention of postpartum hemorrhage. Massive post-partum haemorrhage and management of disseminated intravascular coagulation. International Confederation of Midwives; International Federation of Gynaecologists and Obstetricians. Joint statement: management of the third stage of labour to prevent post-partum haemorrhage. Prevention of postpartum hemorrhage by uterotonic agents: comparison of oxytocin and methyl ergometrine in the management of the third stage of labor. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women not exposed to oxytocin during labour: a double-blind, randomized, non-inferiority trial. Use of Sengstaken-Blakemore tube in massive postpartum hemorrhage: a series of 17 cases. Impact of pelvic arterial embolization for intractable postpartum hemorrhage on fertility. Prophylactic perioperative hypogastric artery balloon occlusion in abnormal placentation. Prophylactic hypogastric artery ballooning in a patient with complete placenta previa and increta. Bilateral uterine artery ligation plus B-Lynch procedure for atonic postpartum hemorrhage with placenta accreta. Ten year follow-up of the effect of the B-Lynch uterine compression suture for massive postpartum hemorrhage. California Maternal Quality Care Collaborative Toolkit to Transform Maternity Care. Developed under contract #11-10006 with the California Department of Public Health; Maternal, Child and Adolescent Health Division. Vespa ne of the most challenging critical care situations is the care of a pregnant patient who develops critical illness. Although many potential critical illnesses may occur during pregnancy, we focus our discussion on neurocritical illness that may arise, leading to an intensive care admission in this chapter. We further focus on the ongoing developments in this topical area and on the critical care aspects of care, most typical of late-term pregnancy. The main points to emphasize in this chapter are as follows: (1) Pregnancy creates a condition prone to inflammatory and thrombotic disease in the brain. There are three main diagnoses or conditions that complicate pregnancy and lead to neurologic emergencies. These are myasthenic crisis, preeclampsia/eclampsia with seizures, and ischemic or hemorrhagic stroke. We explore the important critical care bedside considerations and treatment approaches to each of these conditions and focus on decision making and integration with general critical care goals. For general myasthenic care, consultation with a neurologist should be done, as standard treatments such as steroids may entail an increased risk of birth defects. For the 30% of patients who demonstrate myasthenic crisis, some are in the postpartum period. Myasthenic crisis can be complicated by acute respiratory failure due to diaphragm fatigability. Monitoring of vital capacity and negative inspiratory force is desirable as additional diagnostics. The respiratory mechanics, criteria for intubation, and methods of mechanical ventilation are similar to those of nonpregnant patients. However, a few special considerations of plasmapheresis during pregnancy include an increased risk of perinatal bleeding because of depletion of coagulation factors. Positioning of the mother on her left side during apheresis is a specific precaution to avoid compression of the vena cava. Monitoring of circulating blood volume and avoidance of hypovolemia are other unique precautions. This is usually short-lived but requires supportive care for a short duration, usually 12 to 24 hours. The important steps are as follows: (1) Obtain a detailed history of the timing and specifics of the neurologic deterioration. This is in contrast to our routine practice in critical care of assessing a brief synopsis of the presentation.
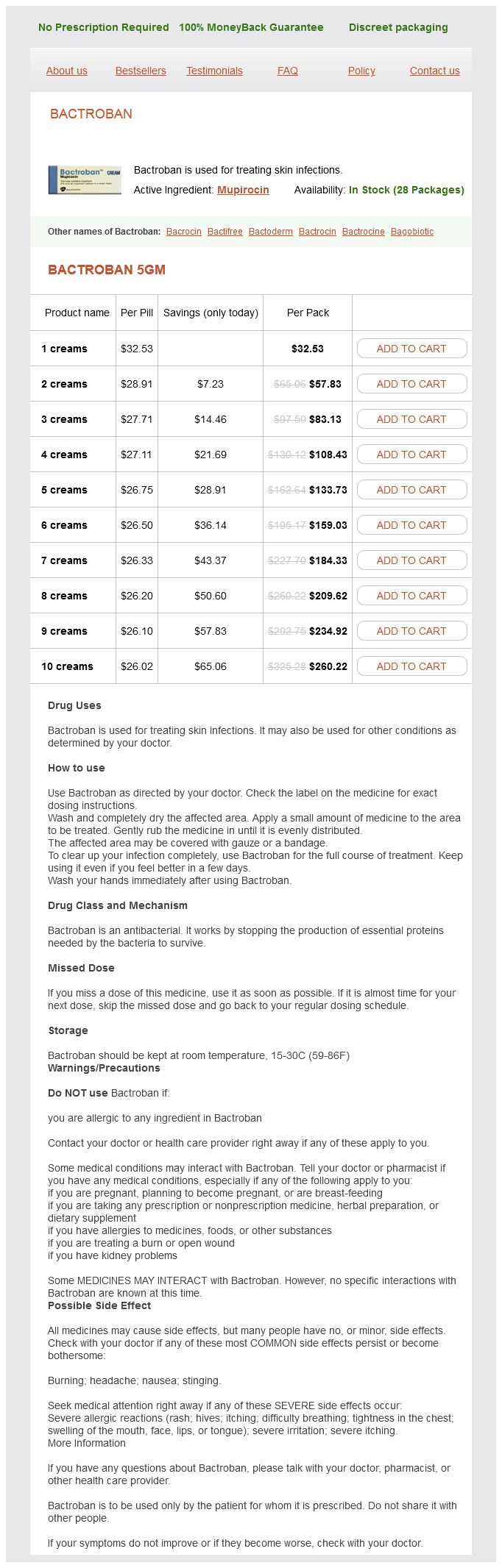
Bactroban Dosage and Price
Bactroban 5gm
- 1 creams - $32.53
- 2 creams - $57.83
- 3 creams - $83.13
- 4 creams - $108.43
- 5 creams - $133.73
- 6 creams - $159.03
- 7 creams - $184.33
- 8 creams - $209.62
- 9 creams - $234.92
- 10 creams - $260.22
Metabolic alkalosis involving the loss or excess secretion of chloride is termed chloride-responsive skin care lines for estheticians generic 5 gm bactroban with amex. Treatment for metabolic alkalosis involves treating the underlying cause by administering intravenous 0. Hemofiltration in sepsis and systemic inflammatory response syndrome: the role of dosing and timing. This disorder can not only result in life-threatening acidemia but also, as a result of malnutrition, causes life-threatening hypophosphatemia. This scholarly review explains the pathophysiology and provides a basis for appreciation of the clinical syndrome. The reported incidence probably underestimates the actual occurrence of lactic acidosis in such patients, especially because recognition may be difficult because many patients remain asymptomatic. Unexplained metabolic acidosis in critically ill patients: the role of pyroglutamic acid. This paper by the same senior author who performed the first controlled clinical trial of dichloroacetate for treatment of lactic acidosis in adults demonstrates that the maximum lactate-lowering effect of dichloroacetate is dose dependent but independent of time after administration. The study suggests that dichloroacetate could be effective in reducing lactate levels in patients with mild hyperlactatemia. This may be an important observation for ongoing investigation in low-level hyperlactatemia as it applies to a number of clinical circumstances. The serum anion gap in the evaluation of acid-base disorders: what are its limitations and can its effectiveness be improved Lactate versus non-lactate metabolic acidosis: a retrospective outcome evaluation of critically ill patients. Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study. Low sensitivity of the anion gap as a screen to detect hyperlactatemia in critically ill patients. Mild hyperlactatemia in stable septic patients is due to impaired lactate clearance rather than overproduction. Impaired hepatic extraction and increased splanchnic production contribute to lactic acidosis in canine sepsis. Evidence for a detrimental effect of bicarbonate therapy in hypoxic lactic acidosis. A comparative study of sodium bicarbonate and carbicarb in the treatment of metabolic acidosis induced by hemorrhagic shock. Effect on arterial blood gases, lactate concentrations, hemodynamic variables, and myocardial intracellular pH. Safety and efficacy of intravenous Carbicarb in patients undergoing surgery: comparison with sodium bicarbonate in the treatment of mild metabolic acidosis. A controlled clinical trial of dichloroacetate for treatment of lactic acidosis in adults. A review of clinical presentation, biochemical features, and pathophysiologic mechanisms. Alcoholic ketoacidosis: clinical and laboratory presentation, pathophysiology and treatment. Acetaminophen-induced anion gap metabolic acidosis and 5-oxoprolinuria (pyroglutamic aciduria) acquired in hospital. Increased anion gap metabolic acidosis as a result of 5-oxoproline (pyroglutamic acid): a role for acetaminophen. Differential diagnosis of nongap metabolic acidosis: value of a systematic approach. Metabolic alkalosis in a hemodialysis patientsuccessful treatment with a proton pump inhibitor. Cimetidine in the management of metabolic alkalosis induced by nasogastric drainage. Continuous renal replacement therapy: cause and treatment of electrolyte complications. Continuous veno-venous hemofiltration using a phosphatecontaining replacement fluid in the setting of regional citrate anticoagulation. Treatment of metabolic alkalosis with intravenous infusion of concentrated hydrochloric acid. The role of the anion gap in detecting and managing mixed metabolic acid-base disorders. Ingested water, plus water produced endogenously, must be appropriately excreted to maintain homeostasis. In the human body, water has many functions: intracellular, intravascular, and extracellular carrier of essential substances; body coolant; lubricant; reactant and product in metabolic reactions; and shock absorber. In critically ill patients, water metabolism and balance present special challenges. Because fat has a lower percentage of water and women tend to have more fat, their proportion of water is lower (52%-55%) than that of men (60%). A 70-kg man has ~40 L of water: ~25 to 27 L intracellularly, ~7 L extracellularly, and ~4 L intravascularly. Therefore, the body defends fluid volume and osmolarity within very narrow ranges. Although more water molecules are produced per mole of fat than per mole of glucose (129 vs. Renal Function: Renal function, the major mechanism defending against disordered water balance, protects blood osmolarity within a narrow range by altering urine osmolarity over a wide range (501200 mOsm). Concentrated urine is formed by creating an osmotic gradient that progressively increases from the corticomedullary border to the tip of the inner medulla.