Cefaclor
General Information about Cefaclor
In conclusion, cefaclor is a commonly used antibiotic medication that is efficient in the treatment of infections attributable to sure strains of micro organism. It is a broad-spectrum antibiotic that can be utilized to deal with a wide selection of infections, making it a popular selection amongst doctors. However, it could be very important use this medication responsibly and as prescribed by a health care provider, to ensure its effectiveness in the future and to stop the development of drug-resistant bacteria.
Cefaclor, additionally recognized by its commerce name Ceclor, is a widely used antibiotic medication that belongs to the cephalosporin household. It is primarily used in the therapy of varied bacterial infections caused by certain strains of bacteria. Cefaclor works by inhibiting the expansion and copy of micro organism, finally eliminating the infection and offering aid to patients.
One of the advantages of cefaclor is its comparatively low danger of unwanted effects. Common unwanted effects may include nausea, vomiting, and diarrhea, but they're normally mild and subside as the body adjusts to the medication. In uncommon instances, some individuals might develop an allergic reaction to cefaclor, which might vary from gentle pores and skin rash to severe anaphylaxis. It is essential to seek medical attention if any concerning unwanted effects occur.
Cefaclor is usually prescribed by medical doctors to treat a variety of respiratory tract infections, including bronchitis, pneumonia, and sinusitis. It can additionally be used to treat skin and gentle tissue infections, urinary tract infections, and some sexually transmitted illnesses. This medicine is available in the type of capsules, tablets, and suspensions, making it convenient for usage by both adults and youngsters.
In some cases, a doctor may prescribe a mixture of cefaclor with another antibiotic to target a selected infection or to stop the event of resistance. This is usually seen in the therapy of respiratory infections, where cefaclor may be combined with one other antibiotic similar to erythromycin.
As with any antibiotic, it is essential to use cefaclor only when prescribed by a physician and to strictly observe the dosage instructions. Failure to take action could end result within the development of drug-resistant micro organism, making the treatment much less effective in treating infections in the future.
Cefaclor is a broad-spectrum antibiotic, which means it's effective against a wide variety of micro organism. This makes it a preferred alternative for treatment, as it could be used to get rid of multiple kinds of infections. However, it is very important notice that it may not be efficient towards all kinds of micro organism, and a health care provider may have to prescribe a special antibiotic if the infection is brought on by a micro organism that is not prone to cefaclor.
Like with most antibiotics, overuse and misuse of cefaclor can lead to the development of antibiotic-resistant bacteria. It is essential to solely use this treatment as prescribed by a doctor, for the really helpful period of treatment. Stopping the treatment prematurely, even if symptoms have improved, also can contribute to the development of resistant micro organism.
Since herbal substances medicine numbers discount cefaclor 500mg buy online, such as ginseng, ginkgo and soy supplements, may also cause menstrual irregularities, history of intake of such products must also be taken. Menstrual History the history of menstrual cycles before the occurrence of episode of abnormal bleeding, including features such as duration of bleeding, the cycle length, whether cycles were regular or irregular, whether there was pain during cycles, etc. The age of menarche and that at which menopause was attained also needs to be asked. Endometrial cancer is also more common in women who have had early menarche and late menopause. These factors are likely to result in a prolonged or unopposed exposure of the endometrium to estrogen, which may result in an increased risk for development of endometrial cancer. Since nulliparity acts as a risk factor for the development of both endometrial carcinoma and uterine leiomyomas, the two are frequently observed to coexist together. On the other hand, conditions like cervical malignancy are more likely to develop in multiparous women. This is especially important because the triad of obesity, hypertension and diabetes is associated with an increased risk of endometrial cancer. Family History · Personal or family history of endometrial, ovarian or breast cancer is another predisposing factor for development of endometrial cancer. Blood pressure: Increased blood pressure could be related with an increased risk for endometrial cancer. Endocrinopathy: the clinician must look for following signs in order to rule out the presence of an endocrinopathy: · Signs of hyperthyroidism and hypothyroidism. Specific Systemic Examination 265 At the time of systemic examination, efforts must be made to rule out the presence of any systemic anomaly. Per Speculum Examination Per speculum examination helps in identifying any trauma or bleeding causing lesions of vagina, cervix, etc. Pelvic Examination A bimanual examination may reveal enlargement due to uterine fibroids, adenomyosis or endometrial carcinoma. An enlarged uniformly shaped uterus in a postmenopausal patient with bleeding suggests endometrial cancer until proven otherwise. Presence of endometrial hyperplasia/malignancy must be ruled out in all postmenopausal women presenting with bleeding, especially those having risk factors for endometrial malignancy. Cervical cytology (Pap smear) is helpful in diagnosis of cervical malignancy, whereas endometrial studies are required to rule out endometrial malignancies. What is the most common type of endometrial cancer on histopathological diagnosis? The endometrioid type of adenocarcinoma accounts for about 80% of endometrial cancers. The endometrial cancers can be of different grades (G1, G2 and G3) based on the degree of cellular differentiation, anaplasia and glandular architecture, with higher grade of tumor associated with a worse prognosis. In case of severe acute bleeding, the aim of management is to stabilize the patient by maintaining the airway, breathing and circulation. Histopathological examination is especially important in these cases to rule out endometrial hyperplasia, atypia and carcinoma. Endometrial sampling can be performed in an outpatient setting, most commonly using a pipelle device, without any requirement for anesthesia and is a noninvasive procedure. Endometrialhyperplasia, especially that associated with atypia could act as a precursor of endometrial carcinoma in the long run. Some histological findings which can be observed on endometrial biopsy are as follows: Endometrial hyperplasia: Chronic proliferation of the endometrium results in the development of hyperplasia (first simple hyperplasia, followed by atypical hyperplasia), leading can be done through administration of conjugated estrogen. Once the bleeding has been controlled, steps must be taken to identify the underlying organic causes. Bleeding could be related to pregnancy complications including threatened abortion, incomplete abortion or ectopic pregnancy. Therefore, pregnancy should be the first diagnosis to be excluded in women of reproductive age group before instituting further testing or medications. These tests are not routinely ordered because they are expensive and the bleeding disorders are rarely encountered. Thyroid testing should only be carried out when the patient shows signs and symptoms, suggestive of thyroid disease. Liver function tests are ordered when liver disease is suspected, such as in persons with alcoholism or hepatitis. It helps in delineating the presence of an enlarged uterine cavity and/or presence of cystic/solid spaces within the uterine cavity. Transvaginal ultrasound is especially indicated in the women at high risk for endometrial cancer. Endometrial hyperplasia usually results from unopposed estrogen production, regardless of the etiology. If a woman takes unopposed estrogen (without progesterone), her relative risk of developing endometrial cancer is 2. Endometrial hyperplasia can be classified as simple (cystic) or complex (adenomatous), with or without cytological atypia. Simple endometrial hyperplasia: this type of endometrial hyperplasia is associated with an increase in the number of glands and endometrial stroma. Simple endometrial hyperplasia with atypia: Endometrial hyperplasia with cytological atypia has high chance for progression into adenocarcinoma, if left untreated. Atypical lesions are distinguished from invasive cancer by the absence of stromal invasion.
If patients are convinced that the symptoms are linked to statin use treatment broken toe 500 mg cefaclor buy fast delivery, then it is worth trying another statin. Moreover, several large trials of fibrates have shown that although non-fatal cardiovascular events are decreased, total mortality increases. Combination treatments In patients who do not achieve target cholesterol levels when they are taking statins, combination treatment can be used. Currently large randomised controlled trials are looking at whether statins and fibrates combined are more beneficial than statins alone. Combination treatments are associated with more side effects and must be used with caution. Gemfibrozil, in particular, interferes with the conjugation of statins, increasing the chances of myositis, and it should not be combined with statins. Combinations of statins with fibrates or nicotinic acid should not be used in secondary hyperlipidaemia, elderly people, or those being treated long term with ciclosporin, tacrolimus, macrolide antibiotics, or antifungals. Lipid lowering drugs should be stopped at least three months before a woman plans to conceive because of potential teratogenicity. Fluctuations in alanine aminotransferase may create the impression that it has risen as a result of statin treatment. Serum cholesterol concentration and coronary heart disease in population with low cholesterol concentrations. A summary of the evidence relating dietary fats, serum cholesterol, and coronary heart disease. A joint statement by the American Heart Association and the National Heart, Lung, and Blood Institute. Disorders of the biogenesis and secretion of lipoproteins containing the B apolipoproteins. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Cardiovascular risk factors in confirmed prediabetic individuals: does the clock for coronary disease start ticking before the onset of clinical diabetes? Outcome of case finding among relatives of patients with known heterozygous familial hypercholesterolaemia. Indications for cholesterol lowering medication: comparison of risk-assessment methods. Evolution of spontaneous atherosclerotic plaque rupture with medical therapy: long-term follow-up with intravascular ultrasound. Systematic review of dietary intervention trials to lower blood total cholesterol in free-living subjects. Efficacy and safety of plant stanols and sterols in the management of blood cholesterol levels. Quantifying effects of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. In 2003, guidance from the National Institute for Health and Clinical Excellence acknowledged that the "rising epidemic of heart failure" is partly the result of people living longer and the more effective treatments for coronary heart disease now available. It also acknowledged, however, that average life expectancy is only about three years after diagnosis, which is much worse than for many other serious illnesses such as cancer of the breast or colon. It is based on evidence from guidelines, randomised controlled trials, and population cohorts followed for many years. We also emphasise the distinction between heart failure with low ejection fraction and heart failure with preserved ejection fraction because although plenty of evidence exists on how to treat the first entity very little exists on how to treat the second. In hospital, patients with heart failure typically present with shortness of breath, exercise intolerance, and leg swelling, and they may have most of the signs in table 1. Dyspnoea, fatigue, exercise intolerance, and fluid retention are common, but some of the other features may not be present. In the community, patients often present with less acute symptoms and fewer clinical signs, and the clinical diagnosis of heart failure can be difficult. Fluid overload Fluid retention may be present in patients who have dyspnoea, an increase in weight from baseline of more than 2 kg in under three days, raised jugular venous pressure, crepitations on chest auscultation, hepatomegaly, or signs of peripheral oedema. Exercise tolerance the degree of exertion needed to elicit symptoms such as breathlessness can be used to grade the severity of symptoms into one of four New York Heart Association functional classes (table 2). Functional class does not define the cause of heart failure or the underlying cardiac abnormality that contributes to the syndrome but the categories are associated with different prognoses. Left ventricular ejection fraction Patients with heart failure may have impaired left ventricular systolic function, which is usually assessed on echocardiography by measuring the left ventricular ejection fraction. However, as many as 50% of patients with the syndrome may have preserved left ventricular ejection fraction (usually defined as >50%), and currently little evidence is available to guide management in these patients (box 1). It is important to distinguish between those with a low ejection fraction and those with a preserved ejection fraction because most of the research into treatment has been done on those with low ejection fraction. Many descriptive studies have shown that patients with diagnosed heart failure in the community are undertreated. In those who almost certainly have clinical heart failure Patients who are acutely unwell are usually admitted to hospital urgently. A bedside clinical assessment is usually sufficient to make a diagnosis without the need for further investigations. An echocardiogram will help to guide treatment for those with heart failure and low ejection fraction. Heart failure is a clinical syndrome comprising reduced cardiac output, tissue hypoperfusion, and congestion. We also reviewed guidelines from the National Institute for Health and Clinical Excellence, Scottish Intercollegiate Guidelines Network, European Society of Cardiology, and the American College of Cardiology Foundation/American Heart Association.
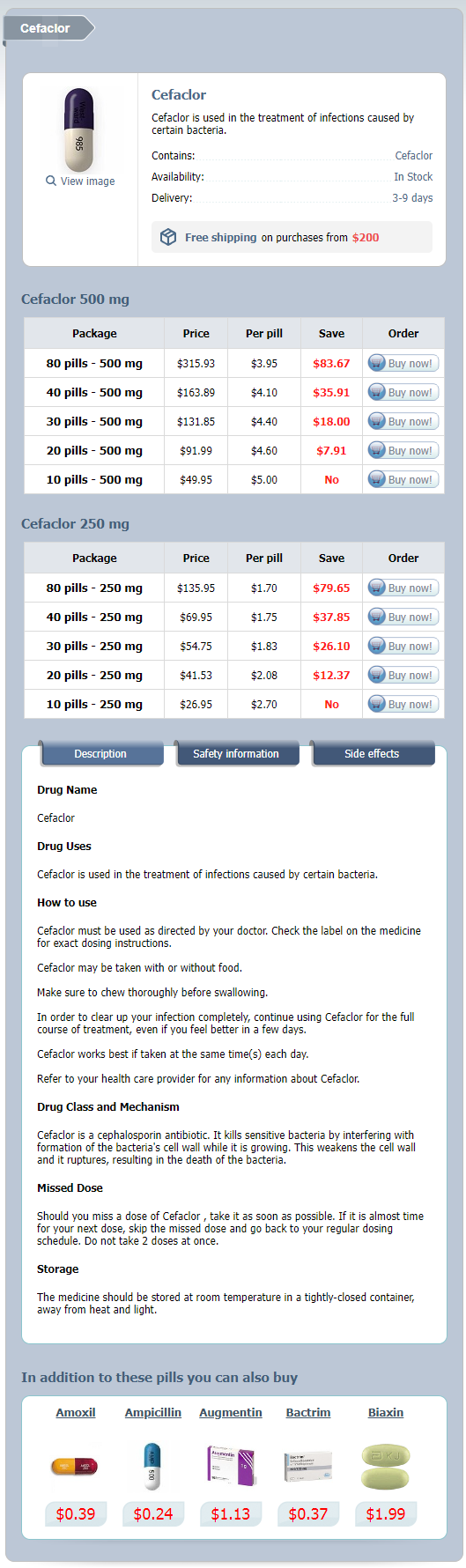
Cefaclor Dosage and Price
Cefaclor 500 mg
- 80 pills - $315.93
- 40 pills - $163.89
- 30 pills - $131.85
- 20 pills - $91.99
- 10 pills - $49.95
Cefaclor 250 mg
- 80 pills - $135.95
- 40 pills - $69.95
- 30 pills - $54.75
- 20 pills - $41.53
- 10 pills - $26.95
Antibiotic prophylaxis to reduce the risk of joint implant contamination during dental surgery seems unnecessary symptoms magnesium deficiency cefaclor 250mg generic. Antibiotics for prevention of periprosthetic joint infection following dentistry: time to focus on data. Both procedures are equally successful regarding alleviation of pain, implant function, and device survival. The comparison of these figures shows a significant increase on both sides of the Atlantic. Prosthetic joints are highly susceptible to infection, due to an impaired host defense around the implant (see Chapter 8) [6Â8]. Most studies revealed patient characteristics, intervention-related factors, and remote infection/bacteremia as risk factors. Previous joint surgery, prolonged operative time, and multiple simultaneous joint implantations are intervention-related risk factors. The risk is very high (> 30%) during documented Staphylococcus aureus bacteremia [15Â17], but relatively low (< 2%) during exposure to a remote infection. Data from five studies with a nonselected population, reporting only cases from a defined joint, and giving the type of microorganisms in sufficient detail, are summarized [24Â28]. Total hip arthroplasty Microorganism Staphylococcus aureus Coagulase-negative staphylococci Streptococcus spp. Gram-negative bacilli Miscellaneous Polymicrobial No growth a Total knee arthroplasty n = 500b 152/500 = 30. The most frequent sources are skin and soft tissue as well as respiratory tract infections. Systemic signs of infection (sepsis syndrome) are frequent, whereas local inflammation is lacking in the early stage. Key symptoms are pain caused by local inflammation, chronic joint effusion, or implant loosening. If the diagnosis is missed for a long time, a sinus tract with spontaneous drainage of pus can be observed [24]. Unfortunately, its specificity for detecting infection is limited, and various cutoffs have been proposed for different types of infections. There are two main indications for testing parameters of inflammation in patients after arthroplasty. Similarly, a neutrophil fraction greater than 80% had a sensitivity of 84% and a specificity of 82% [25]. It allows detecting radiolucency, osteolysis, and migration, which, however, are signs of not only infection, but also aseptic loosening [37]. Ultrasonography can be used for guidance for joint aspiration, which is mainly useful in the hip. With radionuclide imaging, signs of infection are visible before anatomical changes. Bone remodeling, and hence marker uptake, is increased for at least 1 year after implantation [42]. The first question is whether a curative or only a palliative management is planned (see Chapter 8). Cure means complete eradication of infection and restoring a reasonable joint function. In contrast, the aim of palliative treatment is suppression of symptoms either by lifelong oral antibiotic therapy or by surgical removal of the infectious focus without considering function (removal without replacement or amputation). This guarantees the highest tissue levels possible and overcomes possible perioperative disturbance of enteral resorption. The correct duration of treatment has never been tested in a randomized controlled trial. Long-term treatment is based on the concept that remaining bacteria cannot be killed by host defense, if the microorganisms persist as biofilm. Therefore, we suggest a 3-month course in case of debridement with implant retention, one-stage exchange, or two-stage exchange with a short interval (2Â3 weeks) [30, 47, 48]. Since this was not a comparative study, the length of therapy remains a matter of debate. In case of twostage exchange with a long interval (8 weeks), a 6-week course is long enough, because the site of the device is supposed to be sterile at the time of implantation. Antimicrobial dosage recommendations are based on normal renal and hepatic function. Antimicrobials should be chosen based on in vitro susceptibility as well as patient drug allergies, intolerances, and potential drug interactions or contraindications to a specific antimicrobial. In patients with immediate hypersensitivity, penicillin should be replaced by vancomycin. When using combination therapy, monitor signs of ototoxicity and nephrotoxicity of aminoglycosides; the latter is potentiated with other nephrotoxic agents. Use of two active drugs could be considered based on clinical circumstance of the patient. The decision should be based on clinical and laboratory signs of inflammation, formation of hematoma, wound healing, and wound secretion [46]. The role of rifampin for treatment of pathogens other than staphylococci has been reviewed recently. There are not enough data to suggest rifampin combination therapy in streptococcal, enterococcal, P. An additional problem is the rapid emergence of resistance, if rifampin is inappropriately used [53].