Chloroquine
General Information about Chloroquine
Chloroquine is on the market in numerous types, including tablets, injections, and syrup. The dosage and size of treatment could range depending on the condition being treated and the affected person's age and weight. It is necessary to comply with the prescribed dosage and end the complete course of remedy to make sure the an infection is totally eliminated.
In addition to its anti-malaria properties, chloroquine can be used to treat different conditions caused by parasites. For example, it's effective in treating liver diseases caused by protozoa, together with amoebic liver abscess and giardiasis. It may also be used to prevent or treat extraintestinal amebiasis, a type of amebic infection that affects the lungs, liver, and different organs.
Malaria is a life-threatening disease attributable to the Plasmodium parasite, which is transmitted through the chunk of an infected mosquito. When an individual is bitten by an contaminated mosquito, the parasite enters their bloodstream and travels to their liver, where it matures and multiplies. From there, it invades and destroys purple blood cells, leading to signs corresponding to fever, chills, and flu-like signs. Without treatment, malaria may be deadly.
Chloroquine works by killing the Plasmodium parasite, stopping it from multiplying and spreading throughout the physique. It is highly effective against the most common and dangerous types of malaria – Plasmodium falciparum and Plasmodium vivax. This medication is usually used in mixture with different antimalarial medicine to deal with more severe circumstances of malaria.
Chloroquine isn't recommended for use in pregnant ladies, as it could hurt the creating baby. It also wants to be used with caution in patients with pre-existing liver or kidney illness, in addition to those that are on different medicines, as there could additionally be interactions.
In recent times, chloroquine has gained attention for its potential use in treating COVID-19. Some research have shown promising outcomes, however extra analysis is needed to determine its security and effectiveness in treating this illness.
In summary, chloroquine is a extremely effective and versatile medication that has been instrumental in stopping and treating malaria and other parasitic infections. However, it's essential to use it responsibly to avoid the development of drug-resistant parasites. With ongoing research and proper use, chloroquine will continue to play a crucial position in enhancing health outcomes for many people around the world.
While chloroquine is mostly well-tolerated, it may possibly trigger unwanted side effects in some people. Common unwanted aspect effects include nausea, vomiting, diarrhea, and headache. These usually subside because the physique adjusts to the treatment. However, extra severe unwanted effects such as vision adjustments, muscle weak spot, and allergic reactions could occur in rare circumstances. It is essential to seek medical attention if any uncommon symptoms develop while taking this treatment.
Chloroquine is a generally used medicine that has been saving countless lives for over eighty years. It was first developed as an anti-malarial drug within the 1930s and has since been used to deal with a variety of different conditions caused by parasites.
The overuse and misuse of chloroquine have led to drug-resistant strains of malaria, making it less efficient in some components of the world. It is crucial to take this medication solely as prescribed by a doctor and to comply with proper prevention measures, similar to utilizing mosquito nets and bug repellent, to reduce back the spread of malaria.
Because gold-standard isotope dilution techniques are not commonly available symptoms quit drinking generic chloroquine 250 mg buy line, the V is usually calculated using the anthropometric equation described by Watson or Hume-Weyers for adults. A 24-h urine collection to determine urine volume and renal clearance should be performed at least every 2 months. An alternative established measure is creatinine clearance, which is traditionally normalized to a standard body surface area of 1. Other less commonly applied methods of measuring dialysis dose include the solute removal index59 and the dialysis index. Peritoneal clearance is influenced by the volume and rate of dialysate exchanges, effective peritoneal membrane area, peritoneal blood flow, and transport characteristics of the peritoneal membrane. Peritoneal clearance is not constant during a dialysis exchange since the rate of diffusion peaks early during the exchange. The selection of urea as the marker for adequate dialysis dose is still a controversial issue. Small solutes such as urea and creatinine (molecular weight 60 and 113, respectively) have been favored due to their rapid accumulation in blood when renal function diminishes and simplicity of their determination. While urea and creatinine both show a fair correlation between plasma concentrations and clinical outcome, data suggest that urea might be a better surrogate marker of uremic toxicity than creatinine. It is important to keep in mind that the kinetics of urea removal are not representative of other molecules such as middle molecules or protein-bound solutes. Solute removal by dialysis therapy is very limited when compared to the natural kidneys. Achieving appropriate small solute clearances as measured by the Kt/Vurea is only one part of adequate treatment. Other important factors are ultrafiltration volume, sodium intake and removal, maintaining normal hydration status and blood pressure, preservation of residual renal function and quality of life. Apart from achieving the target clearances and the ultrafiltration necessary to maintain euvolemia, considering psycho- Principles of Peritoneal Dialysis: Management and Complications 413 social implications of the chosen modality and patient preferences are equally important factors to consider. The main determinants of dose as expressed in the Kt/V are clearance, time and urea distribution volume. While V cannot be influenced significantly, a higher volume in larger patients still implies the need for higher clearances to achieve the same Kt/V than in smaller patients. Shorter dwell times are required for high transporters and longer ones for slow transporters. Thus, the clearance can be significantly improved by increasing dialysate flow through higher exchange volumes and more frequent exchanges. However, higher glucose concentration could potentially lead to more side effects and thus should be carefuly prescribed. The clearance of large molecules is mostly determined by the membrane permeability and the time of exposure of the dialysate to the peritoneal membrane, rather than by dialysate flow. It typically has an infectious etiology, mostly due to bacteria or, in rare cases, fungus. Peritonitis is a common complication of peritoneal dialysis, with approximately 4% of episodes resulting in death of the patient. Peritonitis may be due to touch contamination during connection and disconnection (intraluminal), the consequence of exit-site infections (pericatheter or extraluminal), hematogenous, or from gynecological or intestinal sources as in the case of diverticulitis. Peritonitis often causes structural changes in the peritoneum that may be permanent and can result in membrane and technique failure. Peritonitis treatment goals include rapidly resolving inflammation by eradicating the causative organism(s) and preserving the function of the peritoneal membrane. A lower rate of peritonitis has recently been reported to have altered this trend. Comprehensive best clinical practice guidelines were established for the diagnosis and treatment of peritonitis by the International Society of Peritoneal Dialysis in 2010. If the protocol is not effective in treatment and prevention of peritonitis, it should be reassessed and changes should be implemented to achieve satisfactory results. The Gram stain should be used to define presence of yeast and permit initiation of antifungal therapy and timely removal of the catheter; however, the Gram stain has limited use for empiric therapy guidance. The differential diagnosis should include other causes aside from peritonitis, such as constipation, peptic ulcer disease, renal or biliary colic, acute intestinal perforation, and pancreatitis. Obtaining the correct microbiological culture from the peritoneal effluent is necessary to identify the responsible organism, as well as the antibiotic sensitivities. After obtaining microbiological specimens for culturing, it is important to start the patient on two antibiotics, immediately one covering Gram-positive and one Gram-negative bacteria. Gramnegative coverage may be obtained through the use of aminoglycosides or third-generation cephalosporins (Table 2). The preferred administration of antibiotics is intraperitoneal; effective intermittent and continuous dosing regimens have been defined in the literature for most antibiotics (Table 3). Subsequent to obtaining the results of the culture and sensitivities, it is recommended that the empiric antibiotic therapy be changed to a narrow-spectrum antibiotic to cover the specific organism as appropriate. Dose adjustments for drugs excreted by the kidney may be necessary in patients with considerable residual renal function. The clinical response is used to guide treatment and to determine the length of therapy. In general, clinical improvement should occur within the first 3 days after antibiotic initiation.
Proximal small intestine is mostly responsible for absorption of proteins medications you cant crush purchase chloroquine 250 mg with mastercard, carbohydrates, and fats. The ileocecal valve serves as a barrier to colonic bacteria and delays small bowel transit which improves nutrient absorption. Loss of the ileocecal valve is associated with rapid intestinal transit and bacterial translocation in the small bowel with subsequent bacterial overgrowth. The ileum is associated with vitamin B12 and bile acid absorption, and resection can lead to vitamin B12 and bile acid malabsorption. Bile acid malabsorption, consequently, can cause fat soluble vitamin deficiency and cholerheic enteropathy. Intestinal adaptation involves lengthening of intestinal villi rather than upregulation of specific transporters. Small bowel dilation and lengthening of intestinal villi increases the absorptive surface area. Enteral feeds facilitate intestinal adaptation by stimulating both biliary and pancreatic secretions as well as enterocyte-derived mediators such a glucagon-like peptide. Intestinal adaptation is less likely if <15 cm small bowel is remaining, the ileocecal valve is removed, or the colon is removed and primary anastomosis cannot be performed. Indirect assessment of intestinal adaptation may be obtained by measuring citrulline, an enterocyte-produced amino acid. These procedures include placement of a gastrostomy tube or gastroduodenal/gastrojejunal tube in patients with motility disorders involving the stomach or duodenum. Continuity of bowel ensures maximal contact and absorption of nutrients, fluid, and electrolytes. Intestinal lengthening procedures have been used to lengthen the dilated small bowel to increase the length of intestine and the absorptive surface. The Bianchi procedure involves longitudinal intestinal lengthening where the lumen is recreated by formation of two narrow channels which are approximated in series to potentially double the length of intestine. There are three different kinds of intestinal transplantation: intestine alone, liver plus intestine, and multivisceral that contains stomach, duodenum, pancreas, intestine, and liver. Transplantation still carries significant morbidity and mortality, including the need for life-long immune suppression and associated complications due to infection and rejection. This modality has been increasingly explored as it would potentially prevent the complications associated with transplant as well as the need for immune suppression. Over the last decade, significant advances have been made to mitigate adverse host reactions. These include a quest for identifying autologous cell sources such as embryonic and adult stem cells, bone marrow-derived cells, neural crest-derived cells, and muscle derived-stem cells. A serial transverse enteroplasty was then performed in an attempt to lengthen the remaining intestine. Children with intestinal lymphangiectasia typically have diarrhea; other symptoms include fatigue, fever, weight loss, and abdominal pain. In general, manifestations are variable and depend on the underlying disease processes (malabsorption, inflammation, infection, or malignancy). Lymphopenia may appear years after the onset of protein loss and in variable ways. Asymmetric peripheral Intestinal lymphangiectasia, an uncommon condition, is characterized by diffuse or localized ectasia of the enteric lymphatics (23. Protein-Losing Enteropathy 201 lymphatic abnormalities elsewhere that may present at any age. Secondary lymphangiectasia Lymphatic obstruction occurs in a wide range of disorders. In children, certain syn dromes are associated with intestinal lymphangiectasia, most notably Turner, Noonan, and KlippelTrénaunayWeber syndromes. Lymphatic obstruction can be seen in patients with infiltrative processes (such as lymphoma, tuberculosis, and sarcoidosis). Elevated lymph pressure can occur from mechanical obstruction (as in malrotation) or can have more remote origins (due to structural heart defects, constrictive pericarditis, cardiomyopathy, following cardiac surgery, or transplant). Severe malnutrition, systemic vasculitidies (including HenochSchönlein purpura), congenital disorders of glycosylation, and Primary lymphangiectasia is characterized by ectatic lymphatics located in the mucosa, submucosa, or subserosa. Lymphatic occlusion or agenesis results in an increase in pressure and rupture, with loss of proteinaceous lymph from the lacteals in mucosal microvilli. In patients with lymphatic disorders, mucosal pathologic changes include alteration in the enterocyte basal membrane glycosaminoglycans. Primary mucosal disorders involve the release of proinflammatory cytokines, resulting in disruption of mucosal cells and in increased intestinal permeability to proteins. Matrix metalloproteinases degrade components of the extracellular matrix in ulcer formation. The degradation of epithelial proteoglycans may be implicated in protein leakage, epithelial permeability, hyperemia, and disruption of the mucosal integrity. It has a molecular weight similar to albumin and is not secreted, absorbed, or present in the diet. Intravenous administration of radiolabeled (chromium 51) Protein-Losing Enteropathy 203 albumin followed by a timed stool analysis is a standard method to assess enteric protein loss. Endoscopy or enteroscopy with biopsy will reveal hypertrophic gastric folds of Ménétrier disease, inflammation, erosion, enteropathy, and certain infections. Diuretics and supportive care (with stockings, limb elevation, and protection of the skin) may help avoid complications from peripheral edema.
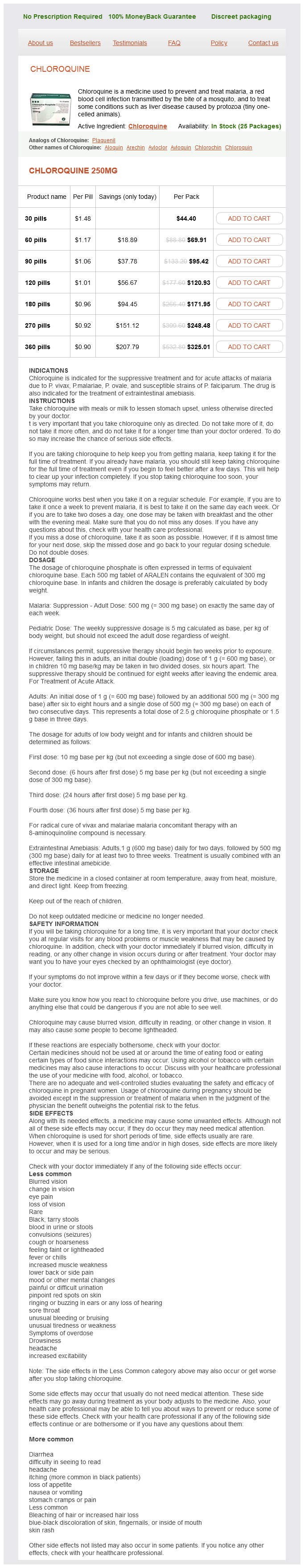
Chloroquine Dosage and Price
Chloroquine 250mg
- 30 pills - $44.40
- 60 pills - $69.91
- 90 pills - $95.42
- 120 pills - $120.93
- 180 pills - $171.95
- 270 pills - $248.48
- 360 pills - $325.01
Upbeat nystagmus may occur with lesions of the dorsal upper medulla or of the midbrain (infarction medications metabolized by cyp2d6 purchase chloroquine amex, tumour, or multiple sclerosis) and is typically transient. Cerebellar or brainstem lesions cause a dysfunction of the velocity-to-position integrator, which helps to hold gaze in eccentric positions. Gaze-evoked nystagmus should be differentiated from physiological end-point nystagmus, which arises beyond lateral gaze angles of 3040 degrees. Cerebellar infarction, for instance, causes direction-changing bidirectional gaze-evoked nystagmus with maximal intensity during gaze to the lesion side or direction-fixed unidirectional gaze-evoked nystagmus beating toward the side of the lesion (Lee et al 2006). Pendular nystagmus corresponds to back and forth eye oscillations without resetting quick phases. This rare nystagmus typically occurs with lesions in the meso-diencephalic junction, as unilateral lesions of the interstitial nucleus of Cajal. In the case of a unilateral peripheral otolithic lesion, the unopposed activity of the intact contralateral side dominates. The head tilt and skew deviation are often absent, whereas static ocular torsion may be present for a longer time, even if with declining intensity. This conjugate ocular torsion towards the affected side may be measured with indirect ophthalmoscopy or fundus photography. This simple test is very useful when the patient visits the outpatient centre after his or her most serious symptoms have abated. The most important role of the positional testing is to demonstrate if that is indeed the case. In order to test the horizontal canals, the head should be positioned sideways, into the lateral positions, preferable from the face-up supine position. The examiner should be aware that a slight peripheral horizontal-rotatory spontaneous nystagmus may be enhanced in lateral supine or in Dix-Hallpike positions and may thus be mistaken for a positional nystagmus. Canalolithiasis produces transient nystagmus after a few seconds of latency, typically lasting less than 15 to 30 seconds; cupulolithiasis causes a more persistent, less intensive nystagmus reaction. With larger masses of debris and repeated manoeuvres, the accompanying motion sickness may exhaust the patient and even elicit vomiting, especially in cases of horizontal canalolithiasis. Relatively recently, the theory of short arm canalolithiasis has been suggested (see Chapter 12), when the Dix-Hallpike and lateral provoking positions do not elicit nystagmus but there is a strong trunk sway and even retropulsion when sitting up from the Dix-Hallpike position. The examiner should note these signs too, as well as the direction, intensity, and duration of nystagmus. Cerebellar tumours and Arnold-Chiari syndrome may cause positional downbeat nystagmus; cerebellar infarction sometimes causes direction-changing laterally beating horizontal positional nystagmus, which may be seen in the lateral supine position. Tumours or haemorrhages in the dorsal vermis or in the cerebellum around the fourth ventricle may cause positional nystagmus and vertigo, which may be impossible to differentiate clinically from a peripheral positional nystagmus. Vibration applied on the mastoid may-similarly to the head-shaking nystagmus-unmask the central compensation of a past peripheral vestibular deficit by eliciting a vibration-induced nystagmus with the fast phase beating away from the affected side. Presumably, unilateral mastoid vibration stimulates the vestibular organs on both sides. Apparently, velocity and direction of caloric nystagmus depend not only on the absolute magnitude of vestibular activity on the stimulated side but also on asymmetry of activity (firing rate) between the left and right vestibular nuclei, most probably mediated centrally via brainstem commissural pathways (Aw et al 2000). If the slow phase velocity of the nystagmus evoked by warm and cold water or air irrigation is decreased on one side (canal paresis), this has localizing significance. If the slow phases to one side dominate on both sides during cold and warm irrigations (isolated directional preponderance), this is usually a transient, benign disorder. The authors postulated that an isolated directional preponderance reflected a gain asymmetry between neurons in the medial vestibular nucleus on either side, caused by increased sensitivity on one side or by reduced sensitivity on the other, perhaps as an adaptive change in response to abnormal input. During these tests, compensatory eye movements with short latency or small amplitude may be difficult for the examiner to assess visually; however, there are commercially available systems consisting of fast infrared video goggles and acceleration sensors, which can be used to examine and document even separate vertical canal excitability. The clinician carries out the head turns by hand; the subject is instructed to fixate a stationary target and to relax the neck muscles. The patient is instructed to fixate on a dot at a reference position straight ahead on a screen at a distance of approx. In cases with unilateral dysfunction, velocities over 100150 degrees/second are sufficient to demonstrate gain asymmetry. Overt saccades can easily be seen during bedside testing, even in spite of spontaneous nystagmus. For the analysis of covert saccades, high-speed infrared video goggles may be necessary. In case of unilateral hypofunction, the physiological disinhibition arriving from the side of the lesion is missing. Therefore, with unilateral vestibular loss, contralesional gains (during head accelerations to the healthy side) are also somewhat reduced. Especially in acute dizziness, when collaboration of the patient is limited, it is important to search for subtle central neurologic signs beyond the oculomotor examination. Results of sensory testing for slight touch, pain, temperature, position sense, and vibration (face, arms, trunk and legs) may be informative. Hearing may be tested by the whisper test (whispered voice with the other ear finger-masked). Chronic partial symmetrical hearing loss is rarely relevant to vestibular diagnosis. Coordination should be tested in the sitting position (although it is also possible in the supine position if the patient cannot be moved, An important question which has to be answered: can the patient sit or even stand unaided Is there compulsory lateropulsion out of proportion to the other complaints (central sign) Static posture may be tested by the Romberg test (ability to stand with the feet together and eyes closed). Patients with unilateral vestibular dysfunction veer (or fall) to the involved side, especially in the acute phase. Patients with bilateral vestibulopathy may perform well during this test, but usually fail on a thick foam carpet. The Unterberger (or Fukuda) stepping test and tandem walk challenge the vestibular system and cerebellar pathways.