Clarithromycin
General Information about Clarithromycin
One of the primary uses of clarithromycin is for respiratory infections, including pneumonia, bronchitis, and sinusitis. Its broad-spectrum effectiveness makes it a preferred alternative for these types of infections. It can additionally be used to treat skin and delicate tissue infections, corresponding to impetigo, cellulitis, and erysipelas. In addition, it is also prescribed for sure ear and throat infections, as properly as in the treatment of Helicobacter pylori (H. pylori) infections associated with peptic ulcers.
Like most antibiotics, there's a threat of creating antibiotic resistance when using clarithromycin. This happens when bacteria mutate and turn out to be resistant to the consequences of the antibiotic, making it tougher to treat infections in the future. To keep away from antibiotic resistance, it's essential to take clarithromycin as prescribed, with out skipping doses or stopping the therapy early.
For sufferers with liver or kidney issues, a decrease dosage may be prescribed, as these organs play a job in metabolizing the drug. It can be essential to inform the doctor of any pre-existing medical conditions and any medications currently being taken to ensure the safety and efficacy of the remedy.
Biaxin is out there in different types corresponding to tablets, extended-release tablets, and oral suspension. The dosage and period of remedy vary, relying on the sort and severity of the infection, as properly as the affected person's age and situation. In basic, the beneficial dose for adults is 250 mg twice a day, whereas for youngsters, the dosage is calculated based on their body weight. It is essential to finish the whole course of treatment, even if the signs disappear, to ensure that the infection is completely eradicated and prevent relapse.
In conclusion, clarithromycin, or Biaxin, is a extremely effective antibiotic used for the remedy of skin and respiratory infections. Its broad-spectrum exercise and minimal unwanted effects make it a popular alternative for medical doctors and patients alike. However, it is very important use this antibiotic responsibly and only under the supervision of a medical skilled to keep away from the development of antibiotic resistance and ensure successful remedy.
Clarithromycin is well-tolerated by most patients, with only a few reported circumstances of unwanted aspect effects. The most typical unwanted facet effects embrace nausea, vomiting, stomach ache, and diarrhea. These unwanted effects are normally gentle and subside on their own after the completion of the treatment. However, if the side effects persist or worsen, it's essential to consult a physician immediately.
Clarithromycin belongs to a class of antibiotics called macrolides, which additionally includes erythromycin and azithromycin. This group of antibiotics works by inhibiting the expansion of bacteria, thereby stopping the infection from spreading and allowing the immune system to fight off the infection extra successfully.
Clarithromycin, marketed beneath the brand name Biaxin, is a broadly used antibiotic within the macrolide family. It is prescribed to deal with quite so much of bacterial infections, significantly within the skin and respiratory system. With its potency and effectiveness, clarithromycin is taken into account as one of the best antibiotics available for treating bacterial infections today.
The diagnosis is usually based on a history of radiation exposure and the clinical findings of kidney injury eosinophilic gastritis elimination diet clarithromycin 500 mg mastercard. Under normal conditions, the renal medullary zone is characterized by low oxygen tension, acidic pH, and high osmolality, which can predispose to increased blood viscosity and red blood cell sickling. This increases the likelihood of local ischemia and infarction of the kidney microcirculation. In the vasa recta, vascular occlusion can interfere with the countercurrent exchange system in the inner medulla, resulting in a defect in the urine-concentrating mechanism. Patients may have nocturia or polyuria and can develop gross hematuria due to papillary necrosis resulting from medullary ischemia and infarction. The sloughed papillae can obstruct urinary tract outflow, leading to obstructive nephropathy and kidney failure. Another abnormality associated with sickle cell disease is proteinuria, a consequence of glomerular hyperfiltration that results from reduction in nephron mass. The treatment of sickle cell nephropathy focuses on primary management of the hematologic disorder. Moreover, heat exposure and consequent dehydration can enhance tubular reabsorption of toxins and potentially enhance toxin-mediated kidney injury. Furthermore, heat exposure can result in heat stroke or low grade rhabdomyolysis that can exacerbate kidney injury. Patients are usually young or middle-aged men, normotensive, have minimal edema, and may describe symptoms of dysuria or nocturia. Laboratory data are notable for elevated creatinine, hypokalemia, hypomagnesemia, hyperuricemia, and urinalysis is often unremarkable with no hematuria and minimal (if any) proteinuria. Histologic features show tubulointerstitial damage, glomerulosclerosis, and chronic glomerular ischemia. Treatment is supportive and further efforts should be directed to preventing disease progression. When kidney function is normal at baseline, unilateral or partial obstruction anywhere along the urinary tract may be asymptomatic, with no discernable change in kidney function or urine output. It is important to address this possibility early in the clinical course of unexplained kidney injury or uremia. Over time, nephron tubules are injured, and the resulting changes in thromboxane A2 and angiotensin levels decrease renal blood flow. If complete obstruction is not relieved, ischemia and nephron loss decrease the glomerular filtration rate. Overall, the clinical presentation depends on the cause, site, and time course of obstruction. Patients with obstructive nephropathy may present with decreased urine output associated with suprapubic pain. Pain resulting from stretching of the urinary collecting system is the most common presenting symptom. Acute ureteral obstruction usually results in severe flank pain that typically radiates to the groin and is referred to as renal colic. Patients with incomplete or intermittent bladder outlet obstruction have urinary hesitancy, dribbling, urgency, decreased urine stream, nocturia, and polyuria. Tubular injury from obstruction causes decreased urinary concentrating capability leading to polyuria. The physical examination should include palpation of the kidney and bladder, as well as a rectal, pelvic, and prostate assessment. The patient may have an enlarged and palpable bladder, enlarged prostate, costovertebral tenderness, groin pain, hypertension, or gross hematuria. The mainstays of the initial evaluation include measurement of the postvoid residual volume of the bladder (>125 mL is considered Lithium Lithium is a monovalent cation, which is freely filtered through the glomeruli. The course of kidney disease after discontinuation of lithium is highly unpredictable, with no reliable clinical clues to identify those destined for recovery or progression. Lithium also is associated with nephrogenic diabetes insipidus, which can occur in up to 40% of patients as early as 8 weeks after lithium initiation. Other tubular dysfunctions associated with lithium include water diuresis, natriuresis, and metabolic acidosis. It is primarily seen in agricultural workers (usually in sugarcane or cotton plantations) in Central America. The most significant risk factor is prolonged, strenuous physical labor in hot and humid climates. They are usually unilateral, solitary, well-defined structures, but they can be multiple and bilateral. They tend to be more common among older adults and are often benign, incidental findings on radiographic imaging. Sonography reveals a thin-walled, fluid-filled cavity with no septations or calcifications. Diagnosis: Simple cysts are usually asymptomatic but occasionally may result in a palpable abdominal mass, infection, back pain, or hematuria. Differentiation of simple cysts from cysts associated with genetic disorders is based on the cystic pattern, age at detection, and family history. If the kidney cyst becomes infected, causes pain, or leads to renin-mediated hypertension, percutaneous drainage is often the first step in further evaluation and management.
Usually there is inadequate water intake due to an alteration in the level of consciousness so that patients become unaware of thirst or cannot adequately communicate the need for water or there is restricted access to water gastritis znaki order clarithromycin 500 mg with mastercard. A reduced sensation of thirst occurs in otherwise normal individuals as a feature of increasing age. The next step is to search for the presence of accelerated water loss or increased Na+ gain, both of which will increase the likelihood of a patient developing hypernatremia. Hypovolemic hypernatremia results from fluid losses in which the Na+ concentration is less than the plasma concentration. Pure water loss, whether from mucocutaneous routes or from the kidneys, causes isovolemic hypernatremia. Because two thirds of pure water loss is sustained from within cells, patients will not become clinically volume depleted unless the water deficit becomes substantial. Insensible losses from the respiratory tract or skin result in concentrated urine. Inappropriate water loss by the kidney, whether from central or nephrogenic diabetes insipidus, results in dilute urine. Although renal water loss can lead to hypernatremia in patients with impaired thirst or access to water, most patients with diabetes insipidus have neither of these defects and typically present with polyuria, polydipsia, and a normal serum sodium concentration. Treatment of Hypernatremia Signs and symptoms of hypernatremia include lethargy, weakness, fasciculations, seizures, and coma. If extracellular osmolality is returned rapidly to normal, the extra intracellular osmoles will pull water into the brain cells, resulting in cerebral edema. Thus, in general, hypernatremia should be corrected slowly by water administration at a rate that leads to half correction in 24 hours. The water deficit can be estimated from the following formula: Water de cit = Current body water (0. This formula also does not include the volume of isotonic saline required in those patients who may be concomitantly volume depleted. Careful monitoring of the serum Na+ is required to ensure the rate of correction is appropriate. Decreases in total body K+ are usually due to gastrointestinal or renal losses whereas hypokalemia in the setting of normal total body K+ is due to cell shift. In most cases, the cause can be determined by history, measurement of blood pressure, examination of acid-base balance, and measurement of urinary K+ levels. The kidney cannot excrete K+ rapidly enough in this setting to prevent life-threatening hyperkalemia. Thus, it is important that this excess K+ be rapidly shifted and stored in cells until the kidney has successfully excreted the K+ load. Insulin excess, whether given exogenously in a patient with diabetes mellitus or endogenous secretion as seen in a normal person given a high glucose load, will lower the serum K+. In the setting of an acute myocardial infarction, hypokalemia may result as a sequela of high circulating epinephrine levels and might predispose to arrhythmias in this clinical setting. Other clinical disorders resulting in intracellular sequestration of K+ are treatment of megaloblastic anemia with vitamin B12, hypothermia, and barium poisoning. Hypokalemic periodic paralysis is inherited in an autosomal dominant pattern and is characterized by episodic hypokalemia resulting in muscle weakness. An acquired form of the disorder is seen in thyrotoxic patients, who are often of Japanese or Mexican descent. Decreased Total Body Potassium In the absence of cell shift, low serum K+ can result from inadequate dietary intake, extrarenal losses through the gastrointestinal tract or skin, or renal losses. The urinary K+ concentration serves as a useful guide in discerning between these possibilities. A urine K+ concentration of less than 20 mEq/L is suggestive of extrarenal losses, whereas a urine concentration of greater than 40 mEq/L suggests renal K+ losses. A urine K+ concentration of 40 mEq/L may be an appropriate response in a hypokalemic patient with maximally concentrated urine due to decreased water intake. By the same token, a random urine value of less than 15 mEq/L may represent renal K+ wasting if obtained in the setting of water diuresis. While still often used, the Cellular Shift With Normal Total Body Potassium In the absence of physical and historical evidence of gastrointestinal or renal K+ losses, either a redistribution of K+ at the cellular level or laboratory error will account for a low serum K+. Spurious causes of hypokalemia can be seen in leukemia patients with leukocyte counts of 100 to 250,000 × 109/L, in which still-viable leukocytes extract K+ from the serum in the sample tube. Interestingly, some patients with acute myeloid leukemia develop kidney K+ wasting due to increased urinary excretion of lysozyme. This protein increases the luminal electronegativity in the collecting duct, providing a greater driving force for K+ secretion. The regulation of K+ distribution between the intracellular and extracellular space is referred to as internal K+ balance. Although the kidney is ultimately responsible for maintenance of total body K+, factors that modulate internal balance are important in the disposal of acute K+ loads. For this reason, a urine K+ to creatinine ratio is now the preferred way to assess renal K+ handling. Clinical situations associated with extreme K+-deficient diets include anorexia nervosa, crash diets, alcoholism, and intestinal malabsorption. Increased renal K+ excretion owing to magnesium deficiency (which is often present in these clinical situations) may contribute to the observed hypokalemia. Primary Increase in Mineralocorticoid Activity Increases in mineralocorticoid activity can be due to primary increases in renin secretion, primary increases in aldosterone secretion, or increases in a non-aldosterone mineralocorticoid or increased mineralocorticoid-like effect.
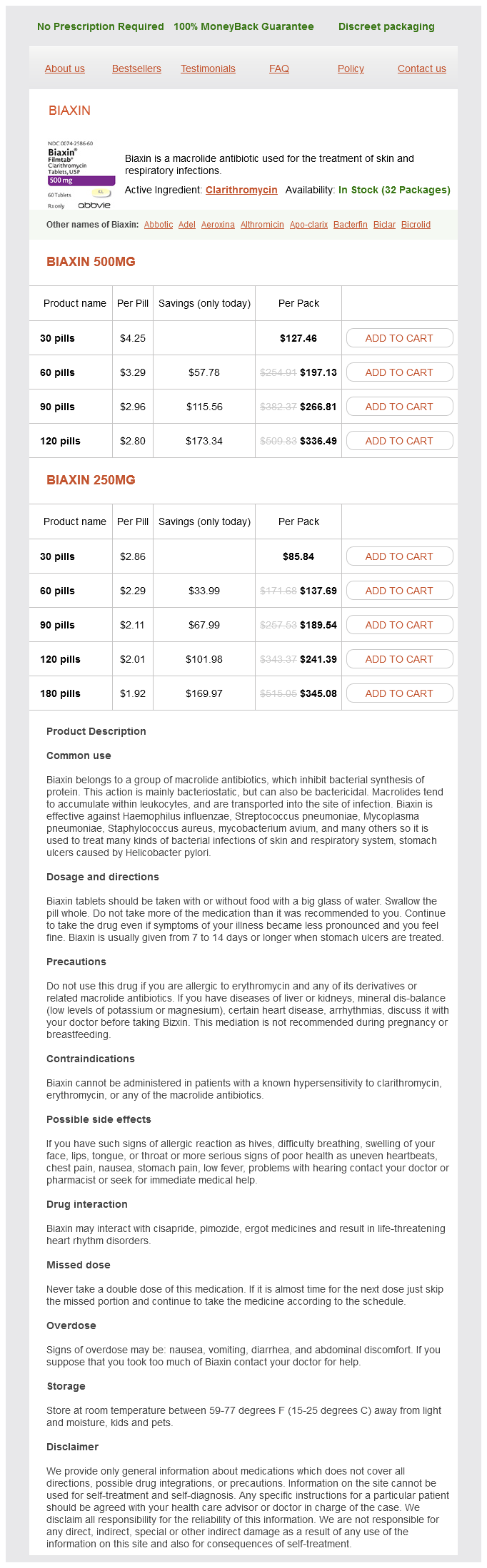
Clarithromycin Dosage and Price
Biaxin 500mg
- 30 pills - $127.46
- 60 pills - $197.13
- 90 pills - $266.81
- 120 pills - $336.49
Biaxin 250mg
- 30 pills - $85.84
- 60 pills - $137.69
- 90 pills - $189.54
- 120 pills - $241.39
- 180 pills - $345.08
Incidence gastritis b12 clarithromycin 250 mg buy, prevalence, and temporal trends of microscopic colitis: a systematic review and metaanalysis. The epidemiology of microscopic colitis in Olmsted County from 2002 to 2010: a population-based study. The epidemiology of microscopic colitis: a 10-year pathology-based nationwide Danish cohort study. The morphologic features of diversion colitis: studies of a pediatric population with no other disease of the intestinal mucosa. Short-chain fatty acids in the human colon: relation to gastrointestinal health and disease. Relationship between the severity of diversion colitis and the composition of colonic bacteria: a prospective study. Histological and histochemical changes in the colon mucosa after ureterosigmoidostomy or colonic conduit. Diversion colitis: histological features in the colon and rectum after defunctioning colostomy. Pathophysiology, clinical presentation and management of diversion colitis: a review of current literature. Effect of butyrate enemas on gene expression profiles and endoscopic/histopathological scores of diverted colorectal mucosa: a randomized trial. Treatment of diversion colitis with 5-aminosalicylic acid enemas: comparison with betamethasone enemas. Intraluminal irrigation with fibers improves mucosal inflammation and atrophy in diversion colitis. Endoscopic treatment of bleeding diversion pouchitis with high-concentration dextrose spray. A national snapshot of the surgical management of deep infiltrating endometriosis of the rectum and colon in France in 2015: a multicenter series of 1135 cases. Intestinal obstruction caused by endometriosis: endoscopic stenting and expedited laparoscopic resection avoiding stoma. Bowel preparation improves the accuracy of transvaginal ultrasound in the diagnosis of 85. Clinical features and treatment responses in pediatric lymphocytic and collagenous colitis. Incidence, clinical presentation, and associated factors of microscopic colitis in Northern France: a population-based study. The epidemiology of microscopic colitis: a population based study in Olmsted County, Minnesota. Decreased colorectal cancer and adenoma risk in patients with microscopic colitis. Lymphocytic ("microscopic") colitis: a comparative histopathologic study with particular reference to collagenous colitis. Macroscopic findings, incidence and characteristics of microscopic colitis in a large cohort of patients from the United Kingdom. The association between the intake of specific dietary components and lifestyle factors and microscopic colitis. Increased risk of microscopic colitis with use of proton pump inhibitors and non-steroidal anti-inflammatory drugs. Drug exposure and risk of microscopic colitis: a nationwide Danish case-control study with 5751 cases. Collagenous colitis and microscopic colitis: the watery diarrhea-colitis syndrome. Genome-wide association identifies multiple collagenous colitis susceptibility loci. Collagenous colitis: implications for the role of vascular endothelial growth factor in repair mechanisms. Subepithelial collagen table thickness in colon specimens from patients with microscopic colitis and collagenous colitis. An evaluation of the significance of microscopic colitis in patients with chronic diarrhea. Bile acid malabsorption in microscopic colitis and in previously unexplained functional chronic diarrhea. Collagenous colitis: a retrospective study of clinical presentation and treatment in 163 patients. Microscopic colitis and reproductive factors related to exposure to estrogens and progesterone. Early life exposure, lifestyle, and comorbidity as risk factors for microscopic colitis: a case-control study. Is there an association of microscopic colitis and irritable bowel syndromea subgroup analysis of placebo-controlled trials. Symptomatic overlap between microscopic colitis and irritable bowel syndrome: a prospective study. Systematic review with metaanalysis: diagnostic overlap of microscopic colitis and functional bowel disorders. Development and validation of a scoring system to identify patients with microscopic colitis. Optimization of a scoring system to Predict microscopic colitis in a cohort of patients with chronic diarrhea. American Gastroenterological association Institute Guideline on the medical management of microscopic colitis.