Clindamycin
General Information about Clindamycin
People with a history of gastrointestinal illness or liver disease ought to use clindamycin with warning. It can even work together with other medications, so it is essential to inform your physician of all medicines and dietary supplements you would possibly be at present taking before starting treatment with clindamycin.
One of the commonest unwanted facet effects of clindamycin is diarrhea. This occurs on account of the medication disrupting the natural steadiness of bacteria in the digestive tract. In some cases, this diarrhea may be severe and even life-threatening. It is necessary to inform a well being care provider should you expertise persistent diarrhea while taking clindamycin.
The use of clindamycin is not with out its own set of risks and precautions. It should only be used when prescribed by a doctor, and the prescribed course of medicine should be accomplished as directed. Stopping therapy prematurely can lead to recurrent infections and the development of antibiotic-resistant bacteria. It is necessary to take the medication on time and at common intervals to keep up a continuing level of the drug in the physique.
Clindamycin is on the market in numerous types including capsules, topical gels, and injections. The applicable type and dose of the treatment will depend upon the sort and severity of the infection being treated.
These infections can embody pneumonia, bronchitis, pores and skin and gentle tissue infections, and infections of the feminine reproductive organs. It can be used to treat sure forms of infections in the mouth, similar to dental abscesses. Clindamycin is a strong treatment that belongs to the class of medicine often identified as lincosamide antibiotics.
Clindamycin works by interfering with the expansion and replication of micro organism. It does this by binding to the 50S ribosomal subunit, part of the bacterial cell responsible for protein synthesis. This prevents the micro organism from producing the proteins essential for their survival, in the end resulting in their death.
Clindamycin is also known to trigger an overgrowth of a selected sort of bacteria called Clostridium difficile, which may result in a critical condition known as pseudomembranous colitis. Symptoms of this situation include extreme diarrhea, abdominal pain, and fever. It is important to seek medical attention if you experience these symptoms whereas taking clindamycin.
Clindamycin has been confirmed to be a highly efficient antibiotic in treating a extensive range of bacterial infections. However, like all antibiotics, its overuse can lead to the event of bacterial resistance. Therefore, you will need to solely use clindamycin as prescribed by a doctor and to complete the total course of treatment. Using it for non-bacterial infections or in an incorrect dosage can also contribute to the event of resistance.
In conclusion, clindamycin is a robust antibiotic that can successfully treat severe bacterial infections. However, it ought to be used with caution and beneath the direction of a physician. It is essential to listen to the potential unwanted effects and precautions associated with this treatment and to communicate any considerations with a healthcare professional. With responsible use, clindamycin can continue to be an efficient weapon in opposition to bacterial infections sooner or later.
It is not recommended to use clindamycin during being pregnant until completely essential. It can pass into breast milk and will hurt a breastfeeding child. It is essential to consult with a doctor before taking this medication in case you are pregnant or breastfeeding.
Traditional therapy is surgical drainage antibiotics libido discount clindamycin 150 mg buy on-line, which usually requires general anesthesia. The incision ideally is placed along Langer skin lines for a cosmetic result (Stehman, 1990). In early cases, a single incision over the most dependent portion of fluctuation is usually sufficient. Multiple abscesses, however, require several incisions and disruption of loculations. The resulting cavity is loosely packed with gauze, which should be replaced at the end of 24 hours by a smaller pack. A more recently used technique that is less invasive is sonographically guided needle aspiration using local analgesia. In a randomized trial, Naeem and colleagues (2012) compared surgical drainage and aspiration. They found aspiration resulted in quicker healing at 8 weeks, 77 versus 93 percent, respectively. Obstet Gynecol 126(3):530, 2015 Baaqeel H, Baaqeel R: Timing of administration of prophylactic antibiotics for caesarean section: a systematic review and meta-analysis. J Matern Fetal Neonatal Med 25(6):743, 2012 Bruhin A, Ferreira F, Chariker M, et al: Systematic review and evidence based recommendations for the use of negative pressure wound therapy in the open abdomen. Am J Obstet Gynecol 182:1147, 2000 Buppasiri P, Lumbiganon P, Thinkhamrop J, et al: Antibiotic prophylaxis for third- and fourth degree perineal tear during vaginal birth. Obstet Gynecol 111:533, 2008 Centers for Disease Control and Prevention: Community-associated methicillin-resistant Staphylococcus aureus infection among healthy newborns-Chicago and Los Angeles County, 2004. Obstet Gynecol 108:482, 2006 Chong E, Winikoff B, Charles D, et al: Vaginal and rectal Clostridium sordellii and Clostridium perfringens presence among women in the United States. Obstet Gynecol 127:360, 2016 Chongsomchai C, Lumbiganon P, Laopaiboon M: Prophylactic antibiotics for manual removal of retained placenta in vaginal birth. Obstet Gynecol 114(4):752, 2009 DiZerega G, Yonekura L, Roy S, et al: A comparison of clindamycin-gentamicin and penicillin gentamicin in the treatment of post-cesarean section endomyometritis. Am J Obstet Gynecol 187(2)305, 2002 Garcia J, Aboujaoude R, Apuzzio J, et al: Septic pelvic thrombophlebitis: diagnosis and management. J Reprod Med 30:549, 1985 Jacobs-Jokhan D, Hofmeyr G: Extra-abdominal versus intra-abdominal repair of the uterine incision at caesarean section. Clin Obstet Gynecol 55(4):904, 2012 Kankuri E, Kurki T, Carlson P, et al: Incidence, treatment and outcome of peripartum sepsis. Gynecologic Oncology 132(3):684, 2014 Liabsuetrakul T, Choobun T, Peeyananjarassri K, et al: Antibiotic prophylaxis for operative vaginal delivery. J Hum Lact 28(4):460, 2012 Matheson I, Aursnes I, Horgen M, et al: Bacteriological findings and clinical symptoms in relation to clinical outcome in puerperal mastitis. Int Gynaecol Obstet 124(3):226, 2014 Okumura K, Schroff R, Campbell R, et al: Group A streptococcal puerperal sepsis with retroperitoneal involvement developing in a late postpartum woman: case report. Am J Obstet Gynecol 193:1759, 2005 Rotas M, McCalla S, Liu C, et al: Methicillin-resistant Staphylococcus aureus necrotizing pneumonia arising from an infected episiotomy site. J Reprod Med 43:586, 1998 Schummer W, Schummer C: Two cases of delayed diagnosis of postpartal streptococcal toxic shock syndrome. Am J Perinatol 30(2):125, 2013 Sherman D, Lurie S, Betzer M, et al: Uterine flora at cesarean and its relationship to postpartum endometritis. J Matern Fetal Neonatal Med 27(12):1237, 2014 Sun J, Ding M, Liu J, et al: Prophylactic administration of cefazolin prior to skin incision versus antibiotics at cord clamping in preventing postcesarean infectious morbidity: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth 107(5):757, 2011 Tulandi T, Al-Jaroudi D: Nonclosure of peritoneum: a reappraisal. Obstet Gynecol 94:153, 1999 Uygur D, Yesildaglar N, Kis S, et al: Early repair of episiotomy dehiscence. New York, McGraw-Hill Education, 2017 Yildirim G, Gungorduk K, Asicioglu O, et al: Does vaginal preparation with povidone-iodine prior to cesarean delivery reduce the risk of endometritis Whitridge Williams (1903) Nearly half of all pregnancies each year in the United States are unintended (Finer, 2016). These may follow contraceptive method failure or stem from lack of contraceptive use. In 2011 to 2013, 7 percent of sexually active fertile women in the United States not pursuing pregnancy did not use any birth control method (Daniels, 2015). For those seeking contraception, effective contraceptive methods are available and variably selected (Table 38-1). With these methods, estimated failure rates of perfect and typical use during the first year differ widely. Contraceptive Failure Rates During the First Year of Method Use in Women in the United States No contraceptive method is completely without side effects, but contraception usually poses less risk than pregnancy. However, some disorders or medications can raise the risks from certain contraceptives. The World Health Organization (2015) has provided and updated evidence-based guidelines, termed Medical Eligibility Criteria, for the use of all highly effective reversible contraceptive methods by women with various health conditions. For a given health condition, each method is categorized 1 through 4 (Table 38-2). The score describes the safety profile for a typical woman with that condition: (1) no restriction of method use, (2) method advantages outweigh risks, (3) method risks outweigh advantages, and (4) method poses an unacceptably high health risk. Contraindications and Cautions with Specific Contraceptive Methods Alternatively, depending on the underlying disorder or patient desire, male or female sterilization may be a preferred or recommended permanent contraceptive method (American College of Obstetricians and Gynecologists, 2017b). These all have a T-shaped frame of polyethylene that is compounded with barium to render them radiopaque.
Nasogastric decompression is necessary only with persistent vomiting or severe distention antibiotic 101 buy generic clindamycin 300 mg line. For prevention, intraoperative goals strive to minimize bowel manipulation, avoid excess intravenous fluids or profound hypovolemia, and limit surgery length (Bragg, 2015). Postoperatively, gum chewing enhances early bowel function recovery by nearly 7 hours after cesarean delivery (Zhu, 2014). Among studies, chewing was initiated immediately or up to 12 hours later, lasted 15 to 60 minutes, and was repeated in at least three sessions daily (Pereira Gomes Morais, 2016). Ambulation and Wound Care As discussed earlier, women undergoing cesarean delivery have an increased risk of venous thromboembolism compared with those delivering vaginally. Brief walks are encouraged, and ambulation can be timed so that a recently administered analgesic will minimize discomfort. Although not evidence based, we remove the surgical dressing after 24 hours and inspect the incision daily. One small randomized trial showed no wound healing differences if removed at 6 hours (Peleg, 2016). Once removed, dressing strips (Steri-Strips) can be placed as needed for 1 week to reinforce skin edge integrity. If there is concern for superficial wound separation, staples remain in place for 7 to 10 days. Hospital Discharge For uncomplicated cesarean delivery, the average hospitalization length is three to four days (Buie, 2010). Data from studies suggest that earlier discharge is feasible for properly selected women and newborns (Bayoumi, 2016; Tan, 2012). Activities during the first week should be restricted to self-care and newborn care with assistance. Driving can be resumed when pain does not limit the ability to brake quickly and when narcotic medications are not in use. In women with cesarean delivery, intercourse was resumed in 44 percent by 6 weeks postpartum, in 81 percent by 3 months, and 97 percent at 1 year (McDonald, 2013). After the puerperium, the quality of sexual functioning does not differ between those undergoing spontaneous vaginal delivery or cesarean (Chang, 2015; Fehniger, 2013; Rogers, 2014). Six weeks is commonly cited, although many women use the Family and Medical Leave Act to allow up to 12 weeks for recovery and newborn bonding. Obstet Gynecol 109(4):917, 2007 American Academy of Pediatrics, American College of Obstetricians and Gynecologists: Guidelines for Perinatal Care, 8th ed. J Matern Fetal Neonatal Med 25(8):1250, 2012 Baksu A, Kalan A, Ozkan A, et al: the effect of placental removal method and site of uterine repair on postcesarean endometritis and operative blood loss. Acta Obstet Gynecol Scand 84(3):266, 2005 Balgobin S: Urologic and gastrointestinal injuries. Am J Perinatol 28(3):207, 2011 Berhan Y, Berhan A: A meta-analysis of reverse breech extraction to deliver a deeply impacted head during cesarean delivery. Obstet Gynecol 89:16, 1997 Chaudhuri P, Mandi S, Mazumdar A: Rectally administrated misoprostol as an alternative to intravenous oxytocin infusion for preventing post-partum hemorrhage after cesarean delivery. Lancet 382(9888):234, 2013 Cromi A, Ghezzi F, Di Naro E, et al: Blunt expansion of the low transverse uterine incision at cesarean delivery: a randomized comparison of 2 techniques. Obstet Gynecol Clin North Am 26(3):469, 1999 Daykan Y, Sharon-Weiner M, Pasternak Y, et al: Skin closure at cesarean delivery, glue versus subcuticular sutures: a randomized controlled trial. Int Urogynecol J 21(5):535, 2010 Duggal N, Poddatoori V, Noroozkhani S, et al: Perioperative oxygen supplementation and surgical site infection after cesarean delivery: a randomized trial. Obstet Gynecol 122(1):79, 2013 Durnwald C, Mercer B: Uterine rupture, perioperative and perinatal morbidity after single-layer and double-layer closure at cesarean delivery. Obstet Gynecol 110(1):31, 2007 Glaze S, Ekwalanga P, Roberts G, et al: Peripartum hysterectomy: 1999 to 2006. Obstet Gynecol 111(3):732, 2008 Glazener C, Elders A, Macarthur C, et al: Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. Obstet Gynecol 115(6):1267, 2010 Güngördük K, Asiciolu O, Celikkol O, et al: Iatrogenic bladder injuries during caesarean delivery: a case control study. J Obstet Gynaecol 30(7):667, 2010 Guo J, Long S, Li H, et al: Early versus delayed oral feeding for patients after cesarean. Am J Obstet Gynecol 201(5):431, 2009 Holmgren G, Sjöholm L, Stark M: the Misgav Ladach method for cesarean section: method description. Presented at the 38th Annual Meeting of the Society for Maternal-Fetal Medicine, February 2018 Irion O, Luzuy F, Beguin F: Nonclosure of the visceral and parietal peritoneum at caesarean section: a randomised controlled trial. Br J Obstet Gynaecol 103:690, 1996 Jacob J, Phenninger J: Cesarean deliveries: When is a pediatrician necessary Br J Radiol 73(873):951, 2000 Kandadai P, Kandadai V, Saini J, et al: Acute urinary retention after cesarean delivery: a casecontrol study. J Am Coll Surg 223(5):704, 2016 Krönig B: Transperitonealer cervikaler Kaiserschnitt. N Engl J Med 334(19):1209, 1996 Larsson C, Saltvedt S, Wiklund I, et al: Planned vaginal delivery versus planned caesarean section: short-term medical outcome analyzed according to intended mode of delivery. J Hosp Infect 91(2):100, 2015 Leijonhufvud A, Lundholm C, Cnattingius S, et al: Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Int J Gynaecol Obstet 99(3):229, 2007 Linder N, Linder I, Fridman E, et al: Birth trauma-risk factors and short-term neonatal outcome. Eur J Obstet Gynecol Reprod Biol 163(1):27, 2012 MacArthur C, Glazener C, Lancashire R, et al: Exclusive caesarean section delivery and subsequent urinary and faecal incontinence: a 12-year longitudinal study. Semin Perinatol 30(5):235, 2006 Menderes G, Athar Ali N, et al: Chlorhexidine-alcohol compared with povidone-iodine for surgicalsite antisepsis in cesarean deliveries. J Perinatol 29(6):416, 2009 National Institutes of Health: State-of-the-Science Conference Statement on Cesarean Delivery on Maternal Request.
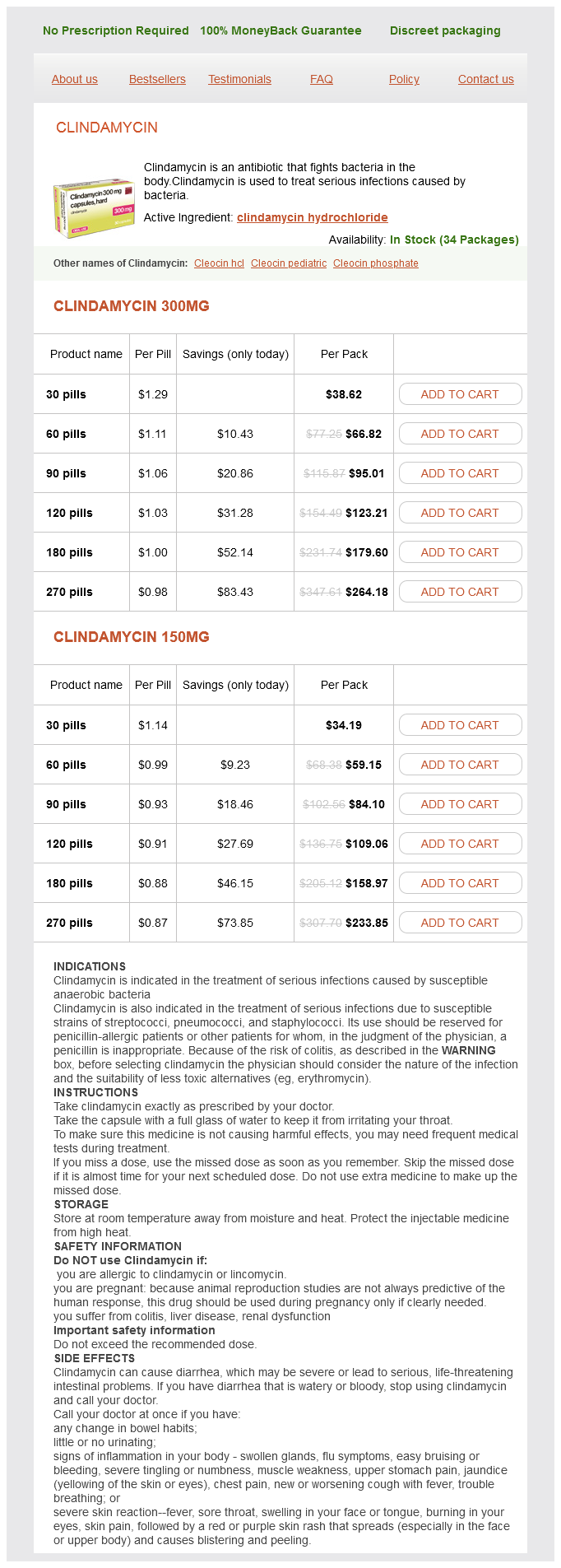
Clindamycin Dosage and Price
Clindamycin 300mg
- 30 pills - $38.62
- 60 pills - $66.82
- 90 pills - $95.01
- 120 pills - $123.21
- 180 pills - $179.60
- 270 pills - $264.18
Clindamycin 150mg
- 30 pills - $34.19
- 60 pills - $59.15
- 90 pills - $84.10
- 120 pills - $109.06
- 180 pills - $158.97
- 270 pills - $233.85
It cites a decision-analysis study that justifies elective delivery without fetal lung maturity testing after 34 completed weeks (Robinson bacteria 1000x magnification order 300 mg clindamycin visa, 2010). Two recent surveys found that most practitioners do not deliver these women until 36 weeks or later (Esakoff, 2012; Wright, 2013). At Parkland Hospital, we generally schedule these procedures after 36 completed weeks but are prepared also to manage them in nonelective situations (Rac, 2015b). Perlman and colleagues (2017) recommend individualization based on specific risk criteria. If there are inadequate resources to surgically manage the percreta, and if the woman is stable and not bleeding, then the fetus is not delivered, the abdominal incision is closed, and she is transferred to a tertiary-care facility. Preoperative Prophylactic Catheterization In cases that may involve one or both ureters, catheterization may aid in dissection or identification and repair of injury. Some, but not all, advocate preoperative ureteral catheterization (Eller, 2011; Society for Maternal-Fetal Medicine, 2010; Tam Tam, 2012). Balloon-tipped intraarterial catheters to mitigate blood loss and thereby enhance surgical visibility have also gained supporters. Catheters are advanced preoperatively into the internal iliac arteries, and then after delivery, they are inflated to occlude pelvic blood flow (Ballas, 2012; Desai, 2012). Alternatively, the catheters can be used to deliver occluding emboli to bleeding arterial sites. Others have concluded that these procedures offer borderline efficacy and have serious risks (Salim, 2015; Sentilhes, 2009). Complications have included thromboses of the common and left iliac arteries (Bishop, 2011). At this time, the American College of Obstetricians and Gynecologists (2017c) concludes that a firm recommendation cannot be made for or against intraarterial catheter use. Similarly, there are no obvious benefits to internal artery ligation (Eller, 2011; Po, 2012). Cesarean Delivery and Hysterectomy Before commencing with delivery, the risk of hysterectomy to prevent exsanguination should be estimated. Some of these abnormal placentations, especially if partial, may be amenable to placental delivery with hemostatic suture placement. Because the scope of invasion may not be apparent before delivery of the fetus, we complete many dissection steps early. This also minimizes blood loss during potentially tedious dissection after hysterotomy. Thus, we usually attempt to create a wide bladder flap before making the hysterotomy incision (Cunningham, 2017b). The round ligaments are divided, and the lateral edges of the peritoneal reflection are dissected downward. If possible, these incisions are extended to encircle the entire placental implantation site that visibly occupies the prevesical space and posterior bladder wall. Following this, a classical hysterotomy or transverse fundal incision is made to avoid the placenta (Kotsuji, 2013). After fetal delivery, the extent of placental invasion is assessed without attempts at manual placental removal. In a report from the United Kingdom, attempts for partial or total placental removal prior to hysterectomy were associated with twice as much blood loss (Fitzpatrick, 2014). Generally speaking, with obvious percreta or increta, hysterectomy is usually the best course, and the placenta is left in situ (Eller, 2011). With more extensive placental ingrowth, there may be little or no bleeding until manual placental removal is attempted. Unless there is spontaneous separation with bleeding that mandates emergency hysterectomy, the operation begins after full assessment is made. With bleeding, successful treatment depends on immediate blood replacement therapy and other measures that can include uterine or internal iliac artery ligation, balloon occlusion, or embolization. The group at Baylor College of Medicine has described a modified radical hysterectomy for surgical management of the morbidly adherent placenta (Shamshirsaz, 2015). At Parkland Hospital, we have had cases in which a traditional radical hysterectomy was necessary to excise all abnormally implanted placenta. Conservative Management Occasionally, it may be possible to trim the umbilical cord, repair the hysterotomy incision, leave the placenta in situ, and not pursue hysterectomy. This option may be used for women in whom abnormal placentation was not suspected before cesarean delivery and in whom uterine closure stops bleeding. After this, she can be transferred to a higher-level facility for definitive management. Another consideration is the woman with a strong desire for fertility and who has received extensive counseling. Conservative management was reviewed by Perez-Delboy (2014) and Fox (2015) and their colleagues. In some of these cases, the placenta spontaneously resorbed between 1 and 12 months with a mean of 6 months. Numerous complications can occur and include sepsis, disseminated intravascular coagulation, pulmonary embolism, and arteriovenous malformation (Fox, 2015; Judy, 2015; Roach, 2015). In some of these women, a subsequent hysterectomy-either planned or prompted by bleeding or infection-is performed days to weeks postpartum when blood loss might be lessened (Al-Khan, 2014; Sentilhes, 2009). In one study, only 21 percent of such women ultimately required hysterectomy (Bretelle, 2007). In other reports, however, up to 60 percent eventually required emergency hysterectomy (Clausen, 2013; Pather, 2014). At this time, we agree with the American College of Obstetricians and Gynecologists (2017c) that leaving the placenta in situ is seldom indicated. Pregnancy Outcomes In sum, these syndromes can have disastrous outcomes for both mother and fetus.