Compazine
General Information about Compazine
However, like several medication, Compazine does have potential unwanted effects. These can embrace dizziness, drowsiness, dry mouth, constipation, and blurred imaginative and prescient. Some patients may also expertise more severe unwanted effects similar to muscle stiffness, tremors, and problem breathing. It is necessary for sufferers to rigorously follow their doctor's directions and report any side effects they expertise.
One of the benefits of Compazine is that it could be taken in several varieties, similar to tablets, suppositories, injections, and oral dissolvable tablets. This allows docs to choose essentially the most appropriate form for each particular person affected person, bearing in mind their situation and preferences. For example, sufferers who expertise nausea and vomiting may favor the oral dissolvable tablets as they are often simply taken with out water, whereas sufferers with severe signs may benefit from the quicker onset of reduction that comes with an injection.
In addition to treating psychotic disorders, Compazine can be generally prescribed for the administration of nausea and vertigo. The actual mechanism behind its effectiveness for these circumstances isn't totally understood, but it is believed that Compazine's capacity to dam dopamine might play a role. Nausea and vertigo may be attributable to many components, corresponding to inside ear issues, motion illness, and chemotherapy treatment. Compazine might help alleviate these signs and provide aid to those that are experiencing them.
In conclusion, Compazine is a highly effective treatment for treating psychotic issues corresponding to schizophrenia and offering relief from the symptoms of nausea and vertigo. With totally different varieties out there and the power to regulate the dosage in accordance with individual wants, it is a versatile drug that may profit a broad range of sufferers. As with any medicine, it could be very important follow your doctor's directions and report any unwanted effects. If you're experiencing symptoms of a psychotic disorder or extreme nausea or vertigo, talk to your doctor about whether Compazine could also be an appropriate therapy choice for you.
Compazine belongs to a class of medications called phenothiazines. These medicine work by blocking the action of dopamine, a neurotransmitter within the brain that is responsible for regulating temper, conduct, and notion. In individuals with psychotic disorders such as schizophrenia, there is an imbalance of dopamine ranges, which might result in signs corresponding to delusions, hallucinations, and disorganized thinking. Compazine helps to cut back these signs by blocking the extreme amount of dopamine within the brain.
Compazine, also called prochlorperazine, is a drugs that is generally used to treat psychotic problems similar to schizophrenia. However, additionally it is used in the treatment of nausea and vertigo, making it a flexible drug that can profit a variety of patients.
Compazine may work together with other medications, so it is very important inform your physician of another medicine you're taking earlier than beginning remedy. It isn't recommended to take Compazine with alcohol, as it may increase the risk of side effects.
These tumours can present with a wide variety of symptoms and can mimic many common diseases of the colon and rectum symptoms 3dpo purchase genuine compazine line, including carcinomas. They can sometimes be asymptomatic and present as an incidentally detected large abdominal mass. R0 resection is usually possible, despite these tumours being large, as they tend to displace rather than infiltrate other organs. Bowel continuity is restored in most patients, and due consideration is given to adjuvant chemotherapy with Imatinib depending on the risk stratification for recurrence and metastasis. These include radical approaches such as anterior resection and abdomino-perineal excision, as well as local approaches like transanal excisions, transvaginal excisions and transsacral excisions. It is also interesting to note that peritoneal dissemination is more common with a trans abdominal approach than with local extra peritoneal procedures and is believed to be due to tumour spill rather than haematogenous metastasis. Tumour-free margins are more common in patients with tumours larger than 5 cm 44 44. Endoscopic ultrasound helps in identifying the origin of the tumour from the muscularis propria, and also defines the layers of the bowel involved. For lesions that are unresectable or where neoadjuvant therapy is being considered, a preoperative biopsy is advisable. A multidisciplinary team consisting of surgeons, oncologists, pathologists and radiologists should make all decisions on treatment. A negative margin after resection is associated with a significant improvement in local disease-free survival but not with an improved overall survival. If there is no response to dose escalation, patients are often switched to Sunitinib, the second line chemotherapy. Neoadjuvant Therapy Neoadjuvant Imatinib is recommended in the following subgroup of patients: 1. Patients with locally advanced lesions not amenable to excision or requiring multivisceral resections 2. It has been shown to significantly improve disease-free and overall survival and reduce local recurrence rates. Therapy is usually continued until maximal response is obtained, defined by no further improvement between two successive scans. It must, however, be noted, that waiting until maximum response is not compulsory before surgical resection. If this is accompanied by a decrease in tumour enhancement, it does not signify tumour progression. Debulking procedures may prolong survival in a selected subset of patients with stable disease or limited progression. For high-risk tumours, follow-up every three to six months for the first three years during Imatinib treatment is recommended. This is followed by imaging every three months for a further two years, and every six months for another three years. The fourth patient underwent a total abdominal hysterectomy and bilateral oophorectomy with cytoreduction for a presumed ovarian malignancy. There was one documented local recurrence in the patient who had a trans anal excision. Dipti Londhe, Department of Pathology, Christian Medical College, Vellore, for providing the histopathology images. Surgical treatment of gastrointestinal stromal tumour of the rectum in the era of imatinib. The epidemiology of malignant gastrointestinal stromal tumors: An analysis of 1,458 cases from 1992 to 2000. Epidemiology of gastrointestinal stromal tumours: Singleinstitution experience and clinical presentation over three decades. Gastrointestinal stromal tumors, intramural leiomyomas, and leiomyosarcomas in the rectum and anus: A clinicopathologic, immunohistochemical, and molecular genetic study of 144 cases. Gastrointestinal stromal tumors and leiomyosarcomas in the colon: A clinicopathologic, immunohistochemical, and molecular genetic study of 44 cases. Gastrointestinal stromal tumors Definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: A meta-analysis of 1,640 patients. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: A randomised controlled trial. Clinical, pathologic, and immunohistochemical characteristics of gastrointestinal stromal tumors of the colon and rectum: Implications for surgical management and adjuvant therapies. Evaluation of prognosis for malignant rectal gastrointestinal stromal tumor by clinical parameters and immunohistochemical staining. Gainof-function mutations of plateletderived growth factor receptor alpha gene in gastrointestinal stromal tumors. Clinicopathologic, phenotypic, and genotypic characteristics of gastrointestinal mesenchymal tumors. Hohenberger P, Ronellenfitsch U, Oladeji O, Pink D, Ströbel P, Wardelmann E et al. Pattern of recurrence in patients with ruptured primary gastrointestinal stromal tumour. Molecular Insights into the Histogenesis and Pathogenesis of Gastrointestinal Stromal Tumors. Gastrointestinal stromal tumors: Review on morphology, molecular pathology, prognosis, and differential diagnosis. Prognostic analysis of rectal stromal tumors by reference of National Institutes of Health risk categories and immunohistochemical studies.
Other methods include the insertion of a papillotome or other means of electrocauthery medicine descriptions 5 mg compazine order with mastercard, but the literature is scarce on the methods or the results of this. The risk of osteomyelitis of the sacrum should always be kept in mind for which prolonged treatment with antibiotics even after symptom resolution is often recommended. The Small Pouch Some patients may have a very small pouch, which can give rise to functional problems, particularly high bowel frequency and urgency. However, pouch size alone is probably Surgical Causes of Pouch Dysfunction 1297 only an explanation for about 20% of all surgical causes of pouch dysfunction. A standard J pouch made of 2 × 15 cm of terminal ileum will achieve a matured final volume of 200 to 350 mL six months to one year post-operatively. In one study, the volume had a mean value of 221 mL at a distension pressure of 40 cm H2O and did not differ significantly from normal rectal volumes. However, the range of measured pouch volumes can be considerable, varying from 65 to 440 mL. If there is no other obvious explanation for pouch dysfunction other than the small pouch, this may be an indication to advise a redo operation, which involves augmentation of the pouch. The pouch has to be mobilised from the pelvis so that another bowel segment can be incorporated by a longitudinal antimesenteric incision between the pouch and the augmented bowel. Great care is needed to ensure that there is no impairment of blood supply to the incorporated segment. Should it be necessary to take down the pouch-anal anastomosis for the reconstruction, usually this has to be hand-sewn from below. A covering loop ileostomy is regularly used after this type of redo surgery and is not reversed until at least two months after surgery and after a contrast enema has ensured that there is healing of the anastomosis. When a patient presents with abdominal or pelvic-pain associated acute emptying problems, a volvulus or a torsion of the pouch should be suspected. Reduction of the volvulus with a semi-stiff rectal catheter and leaving in for a day may solve the problem in the short term, but this condition is prone to recur. An oversized pouch results in constant retention of faecal matter with bacterial overgrowth resulting in metabolic sequelae as well as overflow incontinence. This is not always a straightforward diagnosis, and endoscopy should be complemented with contrast enemas demonstrating the pouch anatomy and an assessment of pouch emptying characteristics. Catheter emptying performed as a Pouch Torsion, Volvulus and Large Dysfunctional Pouches Torsion of the pouch anal anastomosis may explain emptying difficulties. Torsion is usually a result of not having oriented the pouch properly when firing the staple gun. Sometimes, this will become manifested by folding of the lower pouch wall that constitutes a barrier to emptying. Local endoanal procedures with an endostapler, by electocauterisation or other means of cutting through 68. Restorative proctocolectomy for ulcerative colitis: Development and validation of a new scoring system for pouch dysfunction and quality of life. The choice of procedure depends on the cause and may involve resection of a stricture alone. No more than a 1 to 2 cm of anal canal involving the anal transitional zone should remain. Cuffitis is inflammation of the mucosa of the rectal remnant, which has been left above the desired transection site usually because of technical difficulty in resecting the entire rectum in fat short males. The symptoms are variable but include urgency, incontinence, tenesmus and bleeding. Topical mesalazine has been shown to be effective for cuffitis in a small open-labeled trial. The authors suggested that in patients with refractory cuffitis, other diagnoses should be considered. Pouch Prolapse Only a few cases of prolapsing pouches have been reported in the literature. Eigthythree patients from a sample of 23,541 had either a mucosal or full-thickness prolapse. Sometimes, the patient will provide a clear history of prolapse pointing directly to the condition; others will give a more vague description of some difficulty emptying the pouch. For a complete pouch prolapse, the diagnosis is best made by asking the patient to sit on a commode and to push down as hard as they can. Of the reported cases, not all received surgical therapy, and only about half with a full-thickness wall prolapse had a transabdominal pouch pexy operation. The function outcome of a pexy procedure is variable, and some have required a complete pouch reconstruction. When the remaining segment above the dentate line is more than 2 cm, it is considered a retained rectum. In males, however, the pelvis may be very narrow and deep with subsequent difficulties in dissecting all the way down to the pelvic floor. Then there is often also difficulty in applying the cross stapler at the level of the pelvic floor due to a narrow pelvis. In males, the anal canal is longer so the distance between the dentate line to the upper surface of the pelvic floor is longer; thus, it is even more necessary to reach all the way down in men. Furthermore, the retained rectum often leads to increased frequency and incontinence due to inflammation in the retained segment, reduced reservoir function. Surgical Treatment of the Retained Rectum Emptying problems as well as an inflamed retained rectal mucosa not responding to pharmacological treatment may be an indication for a redo operation.
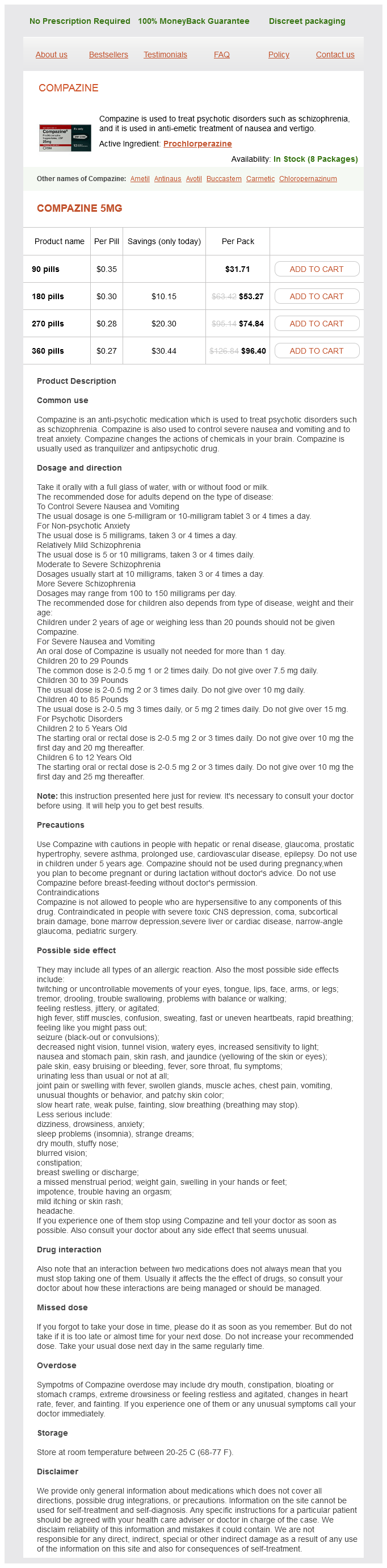
Compazine Dosage and Price
Compazine 5mg
- 90 pills - $31.71
- 180 pills - $53.27
- 270 pills - $74.84
- 360 pills - $96.40
For the desuscepted valve medicine zetia order 5 mg compazine fast delivery, an enterotomy can be made to gain access, the valve can be grasped with tissue forceps or sutures so as to desuscept it again and restaple the valve, avoiding the mesentery. For the floppy incontinent valve, the redundant antimesenteric component can be stapled against a valve catheter. In most instances, the slipped valve can be invaginated and reinforced with additional longitudinal stapler rows, followed by meticulous suturing at the outer circumference of the nipple base, and a good fixation to the anterior abdominal wall. Alternatively, when the quality or length of the slipped valve is insufficient, a new valve can be constructed using 15 cm of ileum entering the pouch. The inlet bowel is transected after division of the mesentery from the bowel attachment reaching about 7 to 10 cm towards the mesenteric root. As in primary nipple valve construction, the mesentery of the first 10 cm leading into the pouch is stripped of its peritoneum and excess fat. The pouch is then rotated 180 degrees, and the proximal bowel end is sutured to the pouch at the site of the original excised valve. In these operations, the proximal bowel used for construction of the new nipple valve is often quite wide, 69 69. The mesentery of the first 10 of 15 cm, leading into the pouch, is stripped of its peritoneum and excess fat. As a consequence, the new valve may be a bit floppy and not perfectly continent upon testing. However, this will usually have no influence on the final outcome, as the nipple valve will, with time, adapt to a normal size. This 180-degree turning with construction of a new valve is also the preferred method for dealing with nipple base fistulas. The crucial component of this is to preserve an adequate blood supply to the transposed small bowel segment. However, with this solution, there is a higher chance for complications, such as anastomotic dehiscence with abscess forming, ischaemia and long-term stenosis of the outlet. In reoperative pouch surgery, one also has to assess whether the pouch can be sited as before or if the abdominal wall opening has become too wide. In such a situation, the best option is usually to move the pouch to the other side of the abdomen. Having the pouch moved to the other side means that the patient has to adjust their emptying routine, but this is rarely a problem. A new passage through the abdominal wall is the preferred option compared to narrowing the previously used trephine by fascia or sutures. Sometimes, a new abdominal wall passage can be achieved on the original side by creating a new hole at a few centimetres away from the original stoma. Mesh reinforcement is another option, but there is a risk of chronic sepsis and fistulas from erosion. Mesh has been tried to achieve better stability of the nipple valve so as to prevent prolapse. It is not obvious that the good results reported with mesh reinforcement of the abdominal wall used in conventional stomas, such as biological meshes, can be directly applied to the continent ileostomy. Re-siting of the continent ileostomy is recommended as a preferred procedure for nipple valve prolapse. An alternative method is to staple the valve to the pouch wall, which can also be used in primary pouch construction. This technique may destabilise the valve, or result in a valve that is less secure. After reoperations for valve dysfunction, the post-operative procedures described in primary continent ileostomy construction should be followed. The studies from Gothenburg and Finland with a 30-year follow-up indicate an even higher rate of nipple valve dysfunction. It is the general experience amongst surgeons involved in continent ileostomies that most patients consider this an excellent alternative to conventional ileostomy, even if the quality of life instruments do not always show this. There are a series of patients with a continent ileostomy operated in one institute, which were compared with a similar group of patients who had undergone an ileal pouch-anal anastomosis or conventional ileostomy. Many patients have had a conventional ileostomy, which was converted to a continent ileostomy, and were, therefore, capable of making a valid comparison. In addition, about one-third of the patients reported some difficulty with intubation of the reservoir in late pregnancy, but in only a few patients did these disturbances result in a revisional operation after delivery. Pregnancy was normal in most patients, and there were only 4 premature births out of 37 pregnancies carried to term. Vaginal delivery was successful in the majority of the patients, caesarean section being chosen for obstetric reasons in nine instances. It is concluded that in the majority patients with a continent ileostomy, pregnancy and delivery is normal. In a few instances, the ileostomy function may be disturbed, necessitating later revisional operations. The Barnett continent intestinal reservoir is a side-by-side J pouch aimed at reducing nipple valve desusception. A multicentre review of 510 Barnett pouches reports that 92% are still functioning, only 6. All quality-of-life and dysfunction scores showed significant improvement over conventional ileostomy.