Crestor
General Information about Crestor
Crestor, also identified by its generic name rosuvastatin, is a prescription drug used to decrease levels of cholesterol in the blood. It was first permitted by the Food and Drug Administration (FDA) within the United States in 2003 and is manufactured by AstraZeneca. It is now out there in many nations and is certainly one of the most commonly prescribed statins.
High cholesterol and atherosclerosis are two of the commonest health situations that millions of individuals face worldwide. Both these circumstances are carefully related as high cholesterol levels can lead to the event and development of atherosclerosis, a condition where the build-up of fatty deposits, also referred to as plaque, happens in the partitions of the arteries. This build-up can finally result in blockages and enhance the danger of heart assault and stroke. To fight these circumstances, medical doctors typically prescribe statins, a class of medicine that help decrease levels of cholesterol. One such drug in this class is Crestor.
Crestor can also interact with certain medicines, so it is important to tell the doctor of all the medicines that are presently being taken, together with over-the-counter medicine and supplements.
However, like some other medication, Crestor also has its potential unwanted facet effects. The most typical unwanted aspect effects embrace headache, muscle ache, nausea, and weak spot. In rare cases, Crestor can cause a critical situation called rhabdomyolysis, where breakdown of muscle tissue can result in kidney failure. It is necessary to seek the guidance of a physician immediately if any signs of this situation, corresponding to muscle pain, tenderness, or weak point, are experienced whereas taking Crestor.
The recommended beginning dose of Crestor is 10-20 mg once daily, with or without food. The dosage may be elevated to a most of forty mg per day if essential. Crestor is available in pill form in numerous strengths, together with 5 mg, 10 mg, 20 mg, and 40 mg. For sufferers who've difficulty swallowing tablets, the medicine may be crushed and blended with a spoonful of applesauce or yogurt.
In conclusion, Crestor is a widely used and effective medicine for the therapy of excessive ldl cholesterol and atherosclerosis. It is important to comply with the prescribed dosage and inform the doctor of any potential side effects. Along with medicine, a healthy diet and regular train are also essential in controlling levels of cholesterol and lowering the chance of heart disease.
Crestor works by inhibiting the enzyme HMG-CoA reductase, which is responsible for the production of ldl cholesterol in the liver. By lowering the production of ldl cholesterol, this medication helps lower the total cholesterol levels within the body. It additionally will increase the degrees of high-density lipoprotein (HDL), generally known as 'good' ldl cholesterol, and decreases the degrees of low-density lipoprotein (LDL), often recognized as 'dangerous' ldl cholesterol, and triglycerides.
Crestor is proven to be efficient in reducing cholesterol levels and preventing the development of atherosclerosis. Clinical trials have shown that it may possibly decrease LDL levels of cholesterol by up to 60%, while rising HDL ldl cholesterol by 15%. It has additionally been proven to reduce back the chance of coronary heart attacks, strokes, and other cardiovascular occasions in sufferers with excessive cholesterol levels.
Loss of intercostal tone would also diminish functional residual capacity and thus worsen hypoxemia during compromised breathing cholesterol medication zocor side effects buy 10 mg crestor mastercard. Premature infants swallow more frequently during apnea than during eupneic breathing. Other evidence of the "central immaturity" of younger infants is the marked increase in periodic breathing particularly during active sleep. Thus, excessive periodic breathing, which is considered pathognomonic for "central immaturity" of respiratory control, frequently has both central and obstructive. A recent longitudinal study of 24 infants born between 27 and 36 weeks gestation showed that all but one had periodic breathing during 23 hour recordings during naps. For most infants, the periodic breathing runs were short and benign, though falls in SpO2% and cerebral tissue oxygenation index were often statistically significant. Three infants had large and sustained falls in heart rate, SpO2% (to <80%), and cerebral oxygenation index. Apneic pauses longer than 5 seconds are common on the first day of life among premature infants without respiratory distress syndrome and can increase to 25 per day by the third day. In the study by Eichenwald and coworkers,35 apnea was diagnosed when chest wall movement was not detected by impedance monitoring. The last events to disappear with maturation were bradycardia episodes without associated central apnea. Another study using transthoracic impedance but incorporating motionartifact resistant oximetry has led to similarly plausible speculation. The majority (75%) of preterm births in the United States each year are in this group, and over 400,000 infants are born at 3337 weeks annually. But concerns are growing about respiratory morbidity and about 80 · Sudden Infant Death Syndrome and Apparent Life-Threatening Events 1133 neurodevelopmental milestones in late preterms, particularly with regards to mathematics and reading skills. Caffeine has replaced theophylline as the methylxanthine of choice because it is as effective and less likely than theophylline to cause tachycardia or poor feeding. How caffeine given more or less prophylactically might reduce the incidence of chronic lung disease is not clear. Esophageal pressure tracing, with cardiogenic artifact, demonstrates first central apnea, then respiratory efforts. Flow and volume tracings show that the first four or five efforts after central apnea are obstructed. However, it has recently been shown that infants have more apnea when their hematocrit is lower, and apnea is less frequent for 3 days after a transfusion. Pulmonologists should be aware of the policies of local pediatric anesthesiologists with respect to perioperative monitoring, even for semielective surgery such as herniorrhaphy. The vexing problem remains whether it is possible to select candidates who will benefit most from monitoring. Monitoring for apnea in preterm infants must continue to be part of this discussion. This fundamental insight led to much research into reflexes, ventilatory control, and brainstem neurochemistry to clarify what was defined as "unexplained" by conventional histopathology. Death results from one or more failures in protective mechanisms against a life-threatening event during sleep in the vulnerable infant during a critical period. In particular, infants unaccustomed to prone sleep are at an 18-fold increased risk for sudden death when placed prone. It emphasizes the likelihood that most deaths have several partial explanations, within a causal sequence. A perspective on neuropathologic findings in victims of the sudden infant death syndrome. In a given infant or group of infants the relative importance of each influence may vary. Investigations into sleep practices over the past 20 years have increased the understanding of exogenous stressors. For example, we might consider a hypothetical infant with a sluggish arousal response to sleep environment threats while prone107,110 who comes to lie prone on bedding that covers the nose and mouth. Moreover, amelioration of one or more of the risk factors present in this example would reduce the risk for death. The success of supine sleep interventions in many countries suggests that the prone position is critical at several junctures in a hypothetical causal sequence, at least among infants sleeping alone. Deaths from accidental suffocation and strangulation in bed rose from ~0 in 1990 to ~0. It summarized the epidemiologic and physiologic research supporting an interaction between sleep position and a sleep environment containing loose blankets and soft sleep surfaces leading to rebreathing that can be lethal and to thermal stress. Three recent important papers address newer issues pertinent to the apparent but sometimes confusing decline in unexpected infant deaths in the 1990s and early in this century. Among reductions they cite are less smoking during pregnancy and fewer mothers never breastfeeding. The percent of infants being put to sleep in the back sleeping position increased from approximately 15% in 1998 to approximately 72% in 2010. However, as the authors claim, they want to quantify how frequently this occurs and recognize ". This suggests that the developmental processes leading to vulnerability occurred earlier in preterm infants. Thus, in general, when infants die suddenly and unexpectedly, perhaps 1 in 6 of the deaths will be explained by postmortem findings or tests done on autopsy specimens. Over half (58%) were explained by autopsy, primarily by congenital heart disease, acute infections, and fatty acid oxidation deficiencies. The model outlined130 may be particularly relevant to increased risk for death linked to nicotine exposure.
Stent placement has been tried in carefully selected patients cholesterol yellow eyes order crestor uk, with biodegradable stents offering a new alternative. Infants with bronchiolitis who develop lobar atelectasis are more likely to have severe disease and require admission to the intensive care unit,17 while exhaustion and sudden severe deterioration may indicate the development of massive atelectasis affecting a whole lung. Preterm infants with bronchiolitis are at higher risk of developing atelectasis,17 and younger children in general are more at risk of developing atelectasis than older children and adults owing to less well developed collateral ventilation effected by the pores of Kohn and the canals of Lambert. Atelectasis may not cause detectable abnormalities on clinical examination; thus the diagnosis must be made radiologically. There may be impaired oxygen saturation, decreased expansion of the chest on the affected side, dullness to percussion, and diminished or absent breath sounds. If the atelectasis is partial or airway obstruction is not complete, crackles may be heard during inspiration and expiration. In some cases of significant or even whole-lung atelectasis, oxygen saturation may be normal, since alveolar hypoxia can induce reflex vasoconstriction and thus minimize ventilation/ perfusion mismatch. Paradoxically, intubation and mechanical ventilation of such patients with supplemental oxygen may cause a temporary deterioration in oxygen saturation due the abolition of the protective vasoconstrictive reflex, thus inducing intrapulmonary shunting and the perfusion of unventilated, atelectatic lung tissue that does not take part in gas exchange. Bronchiectasis, usually caused by recurrent or long-standing airway inflammation, is often complicated by atelectasis. Rounded atelectasis, seen more often in adults than children, is mostly asymptomatic and associated with chronic pleural disease, lung fibrosis, or pleural effusions. Diagnosis the prompt diagnosis of atelectasis in children is important, since early detection and subsequent treatment may lead to an improved outcome. For example, postoperative atelectasis is not uncommon, particularly in children undergoing cardiac surgery. Flexible bronchoscopy has a role in the diagnosis of atelectasis when there is suspected airway obstruction due to , for example, foreign-body inhalation, mucous plugging, endobronchial tuberculosis, airway malacia, external compression from a vascular ring, enlarged lymph nodes, or an enlarged heart. The most frequently used modality for the diagnosis of atelectasis is chest radiography. Frontal projection is always included, but sometimes lateral views are better suited, as in atelectasis of the right middle lobe and the lower lobes. Sometimes fluoroscopy is also used to delineate difficult locations of increased opacification. Fluoroscopy may also be used to diagnose air trapping and mediastinal shift when a foreign body is suspected. In older children, however, an x-ray at end-inspiration followed by another at end-expiration will suffice. Shift of the mediastinum and tracheal contours toward the affected side is quite common, but these general signs may be absent if emphysema develops in the ipsilateral lung or if the atelectasis occurs together with ipsilateral pleural effusion. A summary of major findings on chest radiography related to extent and location of the atelectasis is presented in Table 70. The use of a controlled ventilation protocol reduces the frequency of atelectasis in these children. Chest radiograph shows atelectasis of the right upper lobe and elevation of the interlobar fissure. Computed tomography after sedation shows extensive dependent atelectases in both lungs (Video 70. Bronchiectasis is most pronounced in the atelectatic left-sided middle lobe (Video 70. Ultrasound shows atelectasis of the left lung (a), which is clearly seen next to pleural effusion (p) (Video 70. Bronchography is rarely used but may be combined with diagnostic and therapeutic bronchoscopy in selected cases to show short segments of localized stenosis or bronchomalacia. Treatment and Management the cause of the atelectasis and the presence of any preexisting condition will determine the type of treatment and the need for future prophylactic measures. Chest physiotherapy is often used as a first-line approach, but proof of its efficacy is not firmly established. In a prospective controlled study of 46 mechanically ventilated preschool children with atelectasis, children who were randomized to intrapulmonary percussive ventilation comprising ventilation at 180220 cycles per minute at pressures of 1530 cm H2O for 1015 minutes 4 times daily following instillation of 0. Children who were using controller medications at the time of admission had a higher rate of resolution of atelectasis at 14 days,6 suggesting a therapeutic advantage of antiinflammatory treatment with inhaled or oral steroids. Magnetic resonance imaging shows extensive atelectasis of both lower lobes (Video 70. When the atelectasis is located near the thoracic cage, and especially when it is combined with pleural effusion (as is often the case after cardiac surgery or pleural empyema), ultrasonography is a quick and reliable bedside method. Repeated episodes of atelectasis of the left lung occurred after corrective surgery. Administration of dornase alfa (Pulmozyme), either via nebulizer or direct instillation in intubated patients, may lead to a rapid improvement in atelectasis in children severely ill with respiratory syncytial virus bronchiolitis25 and after cardiac surgery. In children with atelectasis due to suspected inhalation of a foreign body, flexible bronchoscopy to confirm the diagnosis is performed urgently in the case of severe respiratory compromise or electively within the next 24 hours in the majority of cases. The absence of an air bronchogram on chest x-ray in lobar atelectasis is suggestive of proximal airway occlusion and, in this case, bronchoalveolar saline lavage or the direct instillation of dornase alfa may be useful. Diaphragmatic eventration and paralysis can cause lobar collapse that responds to plication of the diaphragm. In children with tracheobronchial obstruction secondary to adjacent vascular structures or an enlarged heart, tumor, lymphadenopathy or severe airway malacia, silicone or wire mesh stents have been used to relieve airway obstruction.
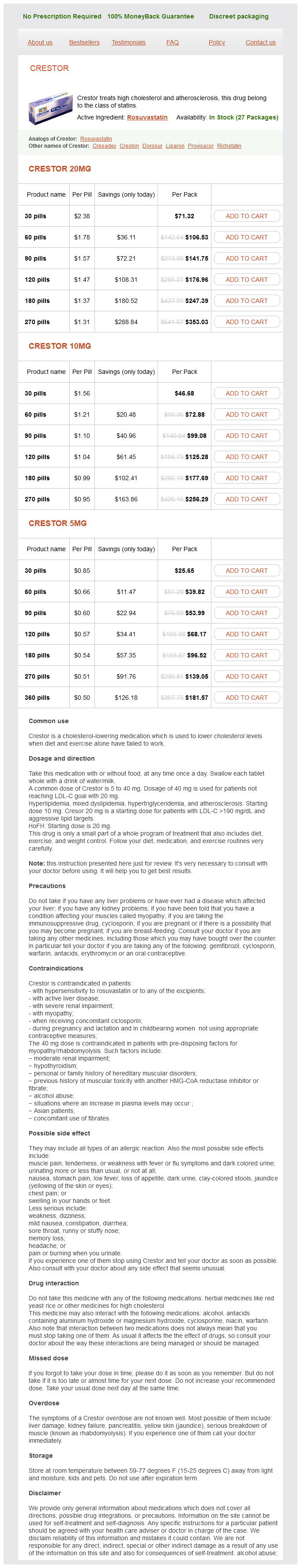
Crestor Dosage and Price
Crestor 20mg
- 30 pills - $71.32
- 60 pills - $106.53
- 90 pills - $141.75
- 120 pills - $176.96
- 180 pills - $247.39
- 270 pills - $353.03
Crestor 10mg
- 30 pills - $46.68
- 60 pills - $72.88
- 90 pills - $99.08
- 120 pills - $125.28
- 180 pills - $177.69
- 270 pills - $256.29
Crestor 5mg
- 30 pills - $25.65
- 60 pills - $39.82
- 90 pills - $53.99
- 120 pills - $68.17
- 180 pills - $96.52
- 270 pills - $139.05
- 360 pills - $181.57
The bronchial microvasculature cholesterol definition english buy crestor 20 mg amex, much like visceral capillaries, is discontinuous, with intercellular fenestrations or gaps. Whether these gaps account for the greater fluid movement across the bronchial capillaries, but not the pulmonary capillaries, remains to be determined. The role of bronchial circulation in the genesis of pulmonary edema may have been underestimated, but it is certain that 580 36 · Pulmonary Edema 580. This, coupled with an improved understanding of the pathogenesis of pulmonary edema, has enhanced our ability to treat various illnesses in which pulmonary edema develops. The interstitial spaces of the alveolar capillary septae and peribronchovascular compartment can only accommodate small amounts of fluid. This anatomic difference, in part, explains why interstitial edema may resolve quickly, whereas alveolar edema takes significantly longer periods of time. They induce an increase in respiratory rate and their continued activation is responsible, in large part, for the continued tachypnea seen in pulmonary edema even when hypoxemia has been corrected through the use of supplemental oxygen and positive airway pressure. Factors Responsible for Fluid Movement the factors responsible for fluid accumulation include intravascular and interstitial hydrostatic and colloid osmotic pressures, permeability characteristics of the fluid-exchanging membrane, and lymphatic drainage. The equilibrium of fluid across fluid-exchanging membranes is generally expressed as the Starling equation: Qf = K f [(Pmv - Ppmv) - (mv - pmv)] wherein, Qf = the net transvascular flow; Kf = the hydraulic conductivity and filtration surface area of the fluid-exchanging vessels; Pmv = microvascular hydrostatic pressure; Ppmv = perimicrovascular (interstitial fluid) hydrostatic pressure; mv = colloid osmotic pressure in the microvasculature; pmv = colloid osmotic pressure in the perimicrovasculature, the interstitial fluid colloid osmotic pressure; and = the reflection coefficient, which is a measure of the resistance of the membrane to the movement of protein. If the endothelium were completely impermeable to protein (protein = 1), then the 5 g/dL of plasma would yield approximately 28 mm Hg osmotic pressure (each 1 mOsm/L of solute yields 19 mm Hg pressure). The osmotic pressure resulting from proteins is also termed the "oncotic pressure. However, it should be emphasized that in the normal lung, Qf is positive and there is a continuous movement of fluid from the vascular to the interstitial spaces of the lung. Experimentally derived values are approximately: Pmv = 20 cm H2O, Ppmv = -2 cm H2O, mv = -33 cm H2O, pmv = 20 cm H2O, and 0. The areas where the basement membranes are fused remain thin; only the areas with a connective tissue interstitial space widen. Extraalveolar vessels lie in the larger interstitial spaces and behave as if their outer walls were exposed to a pressure that is as negative as or more negative than pleural pressure and that tends to vary with pleural pressure. In addition, there are vessels lying in the intersections of alveolar septal walls (corner vessels) that are exposed to more negative pressures than the alveolar vessels. Unfortunately, there is no clear-cut correlation between the functional and the anatomic classifications. In the following discussion, each of the above factors and the pathophysiologic influences on them are described in detail. The pulmonary artery wedge pressure (Pw), also known as the pulmonary artery occlusion pressure, reflects the pressure in the first pulmonary veins where there is flow from nonobstructed vascular routes. The relative amounts of arterial and venular resistance within the pulmonary vasculature is altered during hypoxia, the infusion of vasoactive agents. The plasma colloid osmotic pressure may be markedly reduced in clinical conditions in which the plasma proteins are low. Although only 510 cm H2O may be applied, if the pressure does not distend some areas of the lung as quickly as others, the pressure surrounding lagging units may be considerably greater because of amplification. Surfactant alters the liquid pressure within the airspace and, by extrapolation, the alveolar interstitial pressure. However, when the experimental protocol ensures that there is full recruitment of the pulmonary vascular surface area, there is remarkable consistency of the normalized baseline Kf values between species with widely varying body weights from mice to sheep. Experiments have shown that the walls of the pulmonary circulation are not a perfect semipermeable membrane and that the normal pulmonary vasculature has 0 < < 1. The larger the protein relative to the size of the pore, the less protein will be dragged. When the protein is the same size as or larger than the pore, the reflection coefficient is 1. The pressure surrounding the corner and extraalveolar vessels is less than pleural pressure5 and becomes considerably more negative at high lung volumes. In disease, these negative pressures may be amplified many fold because of "mechanical interdependence" of lung units. Amplification of transpulmonary (distending) pressures by mechanical interdependence is seen in conditions characterized by increased respiratory resistance, decreased lung compliance, and expansion of the lung from the airless state. Mechanical interdependence can act on diseased areas of the lung to produce distending pressures that are exceedingly high. When transmitted to the interstitial space around blood vessels, these pressures can enhance edema formation and can cause the rupture of vessels. Early in the onset of interstitial edema, lymphatic drainage of fluid is an important protective mechanism to prevent alveolar flooding. Although early work had indicated that increased motion or ventilation of the lung increased the lymphatic fluid drainage, suggesting a passive milking action, it is now known that there are active contractions of the lymphatic smooth muscle that can be further augmented by vasoactive agents. Indeed, rhythmic inflation and deflation is not required for normal lymphatic function in lungs that have normal or increased vascular permeability. Because the lymphatics ultimately drain into the great veins, elevation of systemic venous pressure might be expected to increase fluid accumulation, not only by raising pressure in the fluid-exchanging vessels, but also by opposing lymphatic drainage. This surface tension at the alveolar air-liquid interface would be expected to expand the perivascular space and to lower perimicrovascular pressure. As pulmonary edema fluid enters the airspace, it first collects in the corners, but as fluid continues to accumulate, the filling of an alveolus with fluid is self-accelerating once there is a critical amount of fluid present. In each case, there would be an increase in the amount of water and solute leaving the microvasculature and entering the interstitium. Large pleural effusions may develop in diseases such as the nephrotic syndrome, but there is no evidence of lung edema as assessed by gas exchange and chest radiography. However, in patients where vascular pressure or alveolar capillary membrane permeability increases, pulmonary edema is more likely to develop and be more severe when the plasma protein concentration is low. This is seen in various conditions including severe malnutrition, massive burns, protein-losing enteropathies, and nephrosis.