Cytotec
General Information about Cytotec
It is crucial to note that Cytotec should solely be used for its accredited medical purposes. There have been stories of people utilizing it off-label for inducing labor or terminating pregnancies, which may have critical and even fatal penalties. This is why it's strictly regulated and may solely be used underneath a well being care provider's supervision.
In conclusion, Cytotec is a priceless treatment for stopping stomach ulcers in patients treated with NSAIDs or those who undergo from arthritis or continual ache. It presents a protected and efficient approach to manage the danger of ulcers and permits patients to proceed their ache management treatment without worrying about potential stomach injury. However, it's essential to use it as directed and to consult a physician if any unwanted effects happen. With responsible and informed use, Cytotec can provide much-needed reduction to patients suffering from conditions that require long-term use of pain-relieving medicine.
Apart from protecting towards NSAID-induced ulcers, Cytotec can also be used to prevent ulcers in patients who are at a high threat of creating them as a end result of situations like rheumatoid arthritis, osteoarthritis, and ankylosing spondylitis. These situations can cause persistent ache and inflammation, and patients could require long-term use of pain-relieving medication to manage their signs. However, the extended use of these drugs can lead to abdomen ulcers, and Cytotec can be prescribed as a preventative measure to reduce the risk.
Cytotec, also identified by its generic name Misoprostol, is a medicine that has been in use for almost three many years to stop the formation of stomach ulcers in patients handled by NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) or who suffer from arthritis or chronic pain. It is a synthetic prostaglandin E1 analogue that was initially permitted by the FDA (Food and Drug Administration) in 1988 to be used as an anti-ulcer medicine.
NSAIDs, which embody over-the-counter medicine like aspirin and ibuprofen, are commonly used to relieve inflammation, ache, and fever. However, they can also trigger damage to the abdomen lining, leading to the formation of ulcers. These ulcers may be painful and in extreme instances, can even cause bleeding and perforation of the abdomen, which can be life-threatening. This is the place Cytotec is out there in - by stopping the formation of stomach ulcers, it protects patients from the potential unwanted effects of NSAIDs.
Cytotec works by rising the manufacturing of mucus in the abdomen, which helps shield the abdomen lining from the irritative results of NSAIDs. It additionally reduces the production of abdomen acid, which further helps in preventing the formation of ulcers. This makes it an effective medication for patients who require long-term use of NSAIDs for their medical conditions.
Like any treatment, Cytotec additionally has its share of potential unwanted effects. The most common ones embrace diarrhea, abdomen pain, and cramps. Some patients may also experience nausea, vomiting, and bloating. These unwanted facet effects are normally mild and short-term, they usually often subside inside a number of days of beginning the medicine. However, in the event that they persist or turn out to be extreme, it is crucial to seek the assistance of a well being care provider.
Cytotec is usually taken orally, within the form of tablets, either with food or after meals. It can additionally be typically prescribed in combination with NSAIDs, as a single medication generally recognized as Arthrotec. The really helpful dosage depends on the individual's medical condition, age, and response to therapy, and it's essential to follow the doctor's directions rigorously.
In uncommon circumstances, Cytotec may trigger severe side effects, corresponding to allergic reactions, problem respiratory, and irregular heartbeat. It is important to hunt instant medical consideration if any of those symptoms occur. Cytotec can be not recommended for pregnant ladies, as it can cause uterine contractions and result in incomplete abortion or miscarriage.
Electrodiagnostic studies should be performed in patients suspected of having tarsal tunnel syndrome treatment programs buy online cytotec. Periods of immobilization in a short-leg cast or walking boot may allow neuritic symptoms to subside, especially when traction causes pain. Braces and splints can provide added stability and prevent recurrent stretching injuries, especially to the superficial and deep peroneal nerves. Tarsal tunnel symptoms caused by mechanical imbalances-such as acquired pes planus secondary to posterior tendon dysfunction-may be alleviated with orthotic devices that restore foot balance. Multiple forms of pharmacologic intervention exist: Nonsteroidal anti-inflammatories Narcotics (caution must be exercised due to addiction potential, especially with chronic nerve pain) Neuromodulators can help quiet nerve response. Anticonvulsants such as pregabalin, gabapentin, or tricyclics often quiet nerve hypersensitivity. A variety of newer medications may be helpful; thus, referral to a pain management specialist often aids in complete patient care. Lidoderm patches: Applied directly over the symptomatic area, lidocaine hydrochloride is released in a time-dependent manner through the skin. Neuromodulators and local anesthetics and nonsteroidals in an absorbent gel for topical application; these creams can be found in compounding pharmacies. Steroid injection, combined with local anesthetic, may serve a dual role as both therapeutic and diagnostic agent. Risks include skin discoloration, tendon rupture, atrophy of subcutaneous fat, and collateral ligament attenuation. Ethanol injections: 4% ethanol in a Marcaine solution has been used for interdigital neuroma treatment. The benefit, besides avoiding at trip to the operating room, entails loss of nerve conduction without formation of postresection neuroma. The resection of a nerve remains essentially a "one-way street," and careful discussion helps alleviate confusing results. Issues surrounding nerve ending regrowth and possible neuroma formation are dealt with easily later if they are understood preoperatively. The motor loss of the deep peroneal nerve branches is relatively well tolerated, while the posterior tibial nerve governs much more muscle activity in the foot. The posterior tibial nerve has been resected only in salvage procedures as a precursor to possible amputation if unsuccessful. Some surgeons continue to manage these problems with implantable nerve stimulators. Under tourniquet, the vessel and the nerve can look very similar; thus, examination of the cross-section of the presumed nerve is essential at the time of surgery. Even the most experienced surgeons have been fooled by a vein impersonating the nerve: better to know at surgery than to be told by the pathologist the next day. If a patient had reflex sympathetic dystrophy or a complex regional pain syndrome involved with the leg, then consideration should be given to performing the surgery under epidural anesthesia. In theory, the diminution of painful stimulation may diminish the chance of triggering further hypersensitivity reactions. The saphenous nerve is best explored with the patient supine and the leg externally rotated. The superficial and deep peroneal nerves are best approached with the patient positioned supine. Sural nerve exposure often requires use of a rolled towel beneath the ipsilateral hip to provide better access to the nerve as it courses posteriorly. Currently, due to resection of the sural nerve very proximally in the leg, the patient is positioned in a semilateral decubitus position with the use of a beanbag. Preoperative Planning the preoperative planning includes patient education, careful patient evaluation, and decisions regarding the location of nerve burial. The final location of the proximal end of the nerve may be tender; thus, resection of the saphenous nerve just above the ankle in a patient who wears boots that may hit this level would be less desirable and a more proximal burial site would be advised. The surgeon should confirm the location of the nerve tenderness and further discuss postoperative expectations. A tourniquet should be available but is often not used in order to better visualize the vessels accompanying the nerve. Approach While each nerve dictates the appropriate surgical approach, a basic extensile exposure, following the line of the neurovascular structures, seems ideal. The incision is made with a scalpel and deeper dissection is usually performed with dissecting scissors. The variability of several nerves, especially the superficial peroneal nerve, warrants careful exposure and identification. The nerve can be fully exposed and separated from the vessels before resection and burial. If burying the nerve into bone, the surgeon should expose the area of bone to receive the nerve, incising the periosteum and drilling the appropriate hole. A tourniquet may help with exposure, but the vein and branches are better identified without. The sural nerve, perhaps the easiest to find, has anecdotally proved difficult postoperatively with nerve regrowth. The lesser saphenous vein serves as a key landmark in the posterior leg as it courses alongside the sural nerve. Begin the incision just distal to the point of maximal tenderness and carry it proximally along the posterolateral ankle and posterior leg. Tension is placed on the proximal end of the nerve while it is sharply cut in an oblique fashion and allowed to retract into the surrounding tissues. Electrocautery may also be used on the distal fragments to prevent nerve regeneration via production of neurotrophic signals.
Instill a 50:50 mixture of 10 mL of 2% lignocaine hydrochloride (Antigen Pharmaceuticals) and 10 mL of 0 medications kidney infection generic 200 mcg cytotec. The patient is placed prone, and a pillow is placed beneath the anterior aspect of the ankles to allow the feet to hang free. Angle the operating table down about 20 degrees cranially to reduce venous pooling in the feet and ankles. The first is directly over the palpable defect and measures about 2 cm in a transverse direction. The other incisions are about 4 cm proximal and 4 cm distal to the first incision and are vertical 1-cm stab incisions on the medial and lateral aspect of the Achilles tendon. We advocate blunt dissection with a small hemostat directly onto the Achilles tendon. This avoids damaging the sural nerve, which crosses the lateral border of the Achilles tendon about 10 cm proximal to its insertion into the calcaneus. Reintroduce the needle into the medial proximal stab incision through a different entry point in the tendon and pass it longitudinally and distally through the tendon to lock into the tendon. Rethread the suture that is still protruding from the lateral proximal stab incision onto the needle and reintroduce it via the lateral proximal stab incision into the tendon substance. Also pass it longitudinally and distally through the tendon to exit from the middle incision. We sometimes use an eight-stranded method by doubling the sutures used for the Kessler-type technique we are describing. Close the skin wounds with undyed subcuticular 3-0 Vicryl (Ethicon) suture and apply nonadherent dressings. A hemostat is used to free the Achilles from any subcutaneous and peritendinous adhesions. The needle is introduced into the lateral proximal stab incision through the substance of the tendon. The needle is reintroduced into the medial proximal stab incision through a different entry point in the tendon and passed longitudinally and proximally through the tendon, directed toward the middle incision and out through the ruptured tendon end. The same is done with the suture protruding from the lateral proximal stab incision once it is rethreaded onto a needle. Traction is applied to the suture to ensure a satisfactory grip within the tendon. A full plaster-of-Paris cast is applied in the operating room with the ankle in physiologic equinus. After assessment by a physiotherapist, making sure that the patient is safe and comfortable in the cast, the patient can be discharged. The full cast is retained for 2 weeks, and patients are allowed to bear weight as comfort allows. During the period in the cast, patients are advised to perform gentle isometric contractions of the gastrocsoleus complex. At 2 weeks, patients are reviewed as outpatients, the cast is split, and the wounds are inspected. Patients are advised to mobilize with partial weight bearing initially, increasing to weight bearing as able by 4 weeks. The splint is then removed, and physiotherapy follow-up for gentle mobilization is arranged. Light weight-bearing exercise can be started 2 weeks after cast removal, and the patient should be fully weight bearing by 10 weeks. We reviewed 31 patients who underwent percutaneous repair in our tertiary referral center between 2001 and 2003. Surgical shortening of the Achilles tendon for correction of elongation following healed conservatively treated Achilles tendon rupture. Chronic rupture is usually defined as a rupture not appropriately treated within 8 weeks of injury. Chronic or neglected ruptures result in retraction of the proximal myotendinous portion and diastasis between the ruptured tendon ends. This chapter presents a combined reconstruction and augmentation technique for repairing chronic or neglected Achilles tendon ruptures. Without treatment patients develop gait dysfunction, particularly walking up stairs, inclines, or ladders, as well as balance difficulties, with a tendency to fall forward. Silent or spontaneous ruptures may occur in the presence of systemic inflammatory diseases, steroid use, or chronic underlying Achilles tendinosis. Patients are usually able to walk on the limb and plantarflex the ankle without significant pain despite the chronic rupture. Primary complaints are: Weakness of plantarflexion (walking up inclines, stairs, ladders) Gait and balance difficulties Clinical examination Inability to walk on tiptoes Inability to perform a single-leg toe raise (difficulty with double-leg raise) Direct evaluation should be performed with the patient lying prone with both knees flexed to 90 degrees (both sides are examined and compared): Decreased resting tension of the Achilles tendon (normal resting tension of the unaffected side holds the ankle at 20 to 30 degrees of plantarflexion, while the ruptured side will usually be neutral [zero degrees plantarflexion]). Careful palpation can usually detect the proximal end, and the gap can be estimated, although it is difficult to measure clinically. The Thompson test (squeezing the calf) will not result in symmetrical ankle plantarflexion (compared to the unaffected side), although some degree of plantarflexion is usually present in chronic rupture cases. The tendon is loosely surrounded by a paratenon, which allows the tendon to slide about 1. The blood supply to the tendon emanates from the muscle proximally and the calcaneal insertion distally, leaving a watershed area of relatively avascular tendon 4 to 5 cm from the calcaneal insertion. Ruptures occur most commonly in the 30- to 40-year age group, with a male predominance. Eighty percent of Achilles tendon ruptures occur in the watershed area 2 to 6 cm above the insertion. Mechanism of injury resulting in rupture can be forceful plantarflexion or hyperdorsiflexion of the ankle.
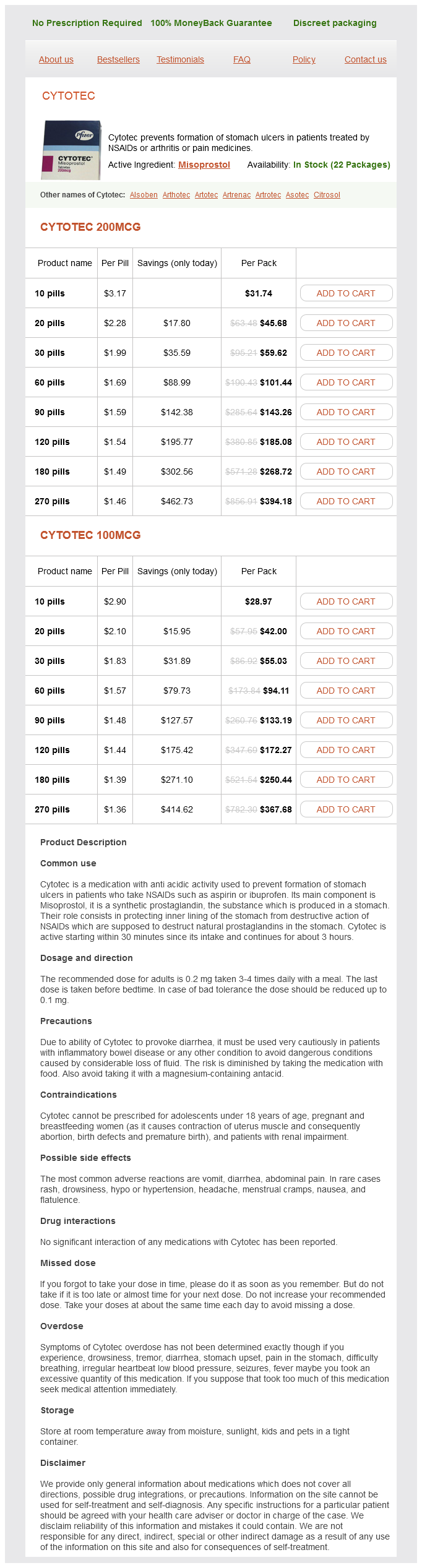
Cytotec Dosage and Price
Cytotec 200mcg
- 10 pills - $31.74
- 20 pills - $45.68
- 30 pills - $59.62
- 60 pills - $101.44
- 90 pills - $143.26
- 120 pills - $185.08
- 180 pills - $268.72
- 270 pills - $394.18
Cytotec 100mcg
- 10 pills - $28.97
- 20 pills - $42.00
- 30 pills - $55.03
- 60 pills - $94.11
- 90 pills - $133.19
- 120 pills - $172.27
- 180 pills - $250.44
- 270 pills - $367.68
Single-stage correction with external fixation of the ulcerated foot in individuals with Charcot neuroarthropathy medicine 014 100 mcg cytotec buy otc. Pattern of diabetic neuropathic arthropathy associated with the peripheral bone mineral density. Biomechanical differences among pes cavus, neutrally aligned, and pes planus feet in subjects with diabetes. The total contact cast for management of neuropathic plantar ulceration of the foot. Salvage, with arthrodesis, in intractable diabetic neuropathic arthropathy of the foot and ankle. Benchmark analysis of diabetic patients with neuropathic (Charcot) foot deformity. Treatment of Eichenholtz stage I Charcot foot arthropathy with a weight-bearing total-contact cast. Guidelines for diabetic foot care: recommendations endorsed by the Diabetes Committee of the American Orthopaedic Foot and Ankle Society. Arthrodesis as an early alternative to nonoperative management of Charcot arthropathy of the diabetic foot. Paper presented at the Annual Meeting of the American Orthopaedic Foot and Ankle Society, Seattle, July 2004. Chapter 44 Axial Screw Technique for Midfoot Arthrodesis in Charcot Foot Deformities Vincent James Sammarco and G. This chapter will demonstrate a technique used for fusion of the unstable midfoot fracture dislocation. Glycosylation and diminished blood supply to the peripheral nerves result in progressive loss of sensation, motor innervation, and autonomic function. Longer nerves are more severely affected, resulting in the typical "stocking and glove" sensory deficit. Loss of protective sensation in the lower limb predisposes patients to ulceration and may make them oblivious to fractures or dislocations. Loss of motor function leads to intrinsic imbalance of muscles in the lower extremity and commonly leads to equinus contracture of the ankle and Achilles, which significantly increases the forces through the foot during gait. Intrinsic imbalance in the foot musculature also results in clawing of the hallux and lesser digits. Autonomic sensory loss results in drying and cracking of the skin, which diminishes integumentary protection from pathogens. Autonomic dysfunction also is responsible for loss of vasomotor control, which may lead to edema and stasis. Once instability develops, bony deformity usually follows and worsens due to neurally stimulated vasomotor response, which increases blood flow to the area and leads to bony dissolution. Fracture and dissociation through the midfoot may progress to a dorsal dislocation of the metatarsals. Once bony dissociation occurs, contracture of the soft tissue envelope makes reduction of the deformity difficult or impossible without surgical resection of bone at the fracture site. Deformity at the level of the midfoot is poorly tolerated and leads to a significant increase in localized plantar pressures at the apex of the deformity. Commonly these increased soft tissue pressures, combined with the previously mentioned loss of protective sensation and loss of normal integumentary function, may lead to ulceration and potentially deep infection. In diabetics, these problems are worsened by impaired circulation and immunologic function and can lead to amputation of the limb. If osteomyelitis develops, limb salvage may still be possible but the risk of amputation is greatly increased. This technique is one of a series of evolving techniques aimed at reconstructing these significant deformities. Prognosis is significantly affected by four things for these patients: the presence of infection, the presence of adequate blood flow in the extremity to the level of the digits, the presence of chronic venous stasis with associated poor integument, and the ability for the patient to adequately control his or her medical comorbidities. Patients who are immunocompromised due to transplant or those receiving dialysis have a much worse prognosis than those with diabetes alone. The presence or absence of infection must be established at the onset of treatment. This may be difficult as many of the physical signs of stage I Charcot deformity are indistinguishable from an infection. Lack of constitutional symptoms does not preclude infection in diabetics, who may not be able to mount an adequate immune response, and patients are often started on antibiotics at presentation. At the time of consultation, the patient has often already been admitted to the hospital with the initiation of intravenous antibiotics, bed rest with elevation of the extremity, and a nonweight-bearing status, thus blurring the ability to distinguish whether the patient improved due to simple rest or medications. A history of fevers and chills, inability for diabetics to control their blood sugar levels, and a history of previous or current ulceration increase the likelihood of active infection at presentation. Any ulceration should be carefully documented, as well as its depth and Wagner grade. It is important to evaluate the contralateral foot and ankle as well as the patient may have pathology that is unrecognized. Typical radiographic changes include fracture and dislocation, bony destruction, periosteal reaction, and malalignment. These findings are difficult to distinguish from acute or chronic osteomyelitis and alone are unreliable for determining the presence or absence of infection.