Decadron
General Information about Decadron
In addition to these conditions, Decadron is used in the therapy of assorted types of cancer. It is used in combination with other chemotherapy drugs to deal with cancers of the white blood cells, such as leukemia, and lymph gland cancers like lymphoma. It can be used to stop and cut back irritation and swelling in the mind in patients with mind tumors.
One of the most typical uses of Decadron is within the treatment of arthritis, as it helps to cut back pain, inflammation, and swelling within the joints. It can be prescribed for other inflammatory circumstances corresponding to lupus, rheumatoid arthritis, and gout. The treatment is also efficient in treating blood problems similar to anemia, which is brought on by a deficiency of red blood cells, and various hormone disorders such as adrenal insufficiency and thyroid issues.
Decadron comes in different types, together with tablets, injections, and topical lotions. The dosage and length of treatment rely upon the situation being handled and the patient's response to the treatment. It is important to follow the prescribed dosage and full the full course of remedy to make sure its effectiveness.
Decadron, also called dexamethasone, is a corticosteroid medicine that is generally prescribed to treat a broad range of health conditions. It is a robust drug that's a part of a group of hormones in the physique referred to as glucocorticoids, that are liable for regulating the immune system and metabolism. Its capability to scale back irritation and suppress the immune system has made it a popular remedy choice for numerous medical circumstances.
As with any medicine, Decadron additionally has some potential side effects, including increased appetite, weight achieve, fluid retention, mood adjustments, and difficulty sleeping. Long-term use may also result in extra severe unwanted facet effects similar to osteoporosis, hypertension, and increased threat of infections. Patients should at all times consult with their physician earlier than beginning any new treatment and report any unwanted aspect effects.
Another important use of Decadron is in the therapy of respiratory problems. It is often prescribed to sufferers with bronchial asthma, chronic obstructive pulmonary disease (COPD), and other breathing problems. It helps to scale back airway irritation and improve inhaling patients with these conditions. Decadron is also used within the therapy of bowel disorders corresponding to ulcerative colitis and Crohn's disease, which are characterized by irritation of the digestive tract.
Decadron is also a vital medicine in the treatment of allergic reactions, including extreme allergic reactions such as anaphylaxis. It works by suppressing the body's natural immune response to allergens, thereby lowering symptoms similar to swelling, itching, and inflammation in the affected areas. Additionally, it is used to deal with sure skin circumstances like psoriasis and eczema, that are brought on by an overactive immune system.
In conclusion, Decadron is a versatile treatment that's widely used to treat a variety of medical situations. Its capacity to cut back irritation and suppress the immune system has made it a vital software within the therapy of various illnesses and issues. However, like all medicine, it must be used carefully and underneath the supervision of a healthcare skilled. It is essential to grasp its potential unwanted effects and search medical attention if any adverse reactions occur. If prescribed and taken as directed, Decadron can considerably improve the quality of life for sufferers with a spread of circumstances.
Even positron emission tomography/computed tomography scans will not identify all patients with extrapelvic disease acne inversa images discount decadron 1 mg without prescription. Although controversial, surgical staging has been advocated to accurately define the extent of disease and guide the subsequent radiation fields. This approach afforded the surgeon excellent exposure to both the pelvic and para-aortic nodes with the ability to debulk grossly positive nodes. A transperitoneal laparotomy approach is not recommended because it is associated with a significant increase in the rate of severe postirradiation enteric morbidity compared to extraperitoneal laparotomy, presumably secondary to adhesion formation. Both transperitoneal and extraperitoneal laparoscopic approaches have been described for surgical staging of cervical cancer. Initially, there was concern that transperitoneal laparoscopic lymph node dissection would be associated with increased adhesion formation as experienced with transperitoneal laparotomy for lymphadenectomy. However, transperitoneal laparoscopy, in general, is associated with fewer intraperitoneal adhesions when compared to laparotomy. Blinded studies in animal models reveal a similar rate and severity of adhesions between transperitoneal laparoscopic lymph node dissection and extraperitoneal laparotomy; however, transperitoneal laparoscopic lymphadenectomy is associated with significantly fewer adhesions compared to transperitoneal laparotomy. Multiple single-institutional series exist describing laparoscopy for pretreatment lymphadenectomy for advanced cervical cancer. A significant advantage for the laparoscopic approach is avoiding potential complications of a large abdominal incision and quicker postoperative recovery, allowing the patient to proceed to definitive radiation therapy more quickly. Although laparoscopic resection of nodes grossly involved with metastatic disease is technically feasible, it is definitely more difficult compared to laparotomy, especially when the nodes are fixed to vessels. Therefore some surgeons prefer extraperitoneal laparotomy in case they encounter nodes that require debulking. As in laparoscopy, the robotic approach can be used for pelvic and para-aortic lymph node dissection. In addition, the three-dimensional magnified vision, enhanced surgeon control over the operative field, and precision afforded by the wristed instruments enable the surgeon to perform the more complicated debulking surgeries if necessary. Before the availability of advanced laparoscopic procedures, vaginal hysterectomy was a less invasive option for definitive surgical therapy, especially in patients with severe comorbidities and increased risk of complications secondary to laparotomy. In fact, assuming the disease is confined to the uterus, the curative potential of the hysterectomy should be equivalent regardless of the surgical approach. The addition of laparoscopy to the vaginal hysterectomy essentially eliminates these disadvantages. The majority of patients with extrauterine disease have occult (without gross evidence) spread. Current disease assessment modalities such as preoperative imaging, intraoperative palpation, gross inspection, and frozen section of the uterus all are inaccurate when compared to comprehensive surgical staging that includes bilateral pelvic and para-aortic lymph node dissection. Comprehensive surgical staging with lymphadenectomy provides the best definition of the biologic nature of the disease and allows the oncologist to make informed postoperative treatment decisions. The overall management of patients with apparent early-stage endometrial cancer continues to evolve. Endometrial cancer remains the least uniformly managed gynecologic malignancy, even among gynecologic oncologists. It remains controversial whether all patients should have surgical lymph node assessment and, in those undergoing lymphadenectomy, the extent to which lymph node dissection should be performed. Although controversial, recent reports on surgical staging of endometrial cancer recommend that selected patients at high risk for extrauterine disease have a bilateral para-aortic dissection to the level of the renal vessels. The reported benefits of a laparoscopic approach in endometrial cancer are lower blood loss and transfusion rates, shorter hospital stay, faster postoperative recovery, and superior short-term quality of life, albeit at the expense of longer operative times. Additionally, these series vary as to whether comprehensive surgical staging was performed and, if so, as to the extent of lymph node dissection (Table 21-4). Surgeon experience and patient factors such as obesity and/or previous abdominal surgery contribute to the many disadvantages of the laparoscopic approach in endometrial cancer, especially if the goal is comprehensive surgical staging. A recent survey of members of the Society of Gynecologic Oncologists (29% responding) revealed that use of laparoscopy as a surgical treatment option for endometrial cancer is increasing; however, only 8% of all respondents use this approach in more than 50% of their cases. Therefore the majority of patients who present with endometrial cancer will undergo definitive surgical management via laparotomy rather than laparoscopy. Until recently, there was no prospective randomized trial reporting the surgical outcomes comparing laparoscopy and laparotomy in the management of endometrial cancer. All patients in this study were to undergo complete surgical staging and were randomly assigned in a 2: 1 ratio of laparoscopy to laparotomy. More than half of these conversions were a result of poor visualization (exposure), 16% were from metastasis, and 11% were from bleeding. In this landmark study, there was no significant difference in rate of node positivity between the two groups; however, significantly fewer patients in the laparoscopy arm (78. Consistent with other studies in the literature, operative time was significantly longer for the laparoscopic arm (203 minutes) versus the laparotomy arm (136 minutes). By 6 months after surgery, no significant quality of life differences were found except in that of body image. Previously reported but small single-institution studies reveal no differences in survival between laparoscopy and laparotomy for the surgical management of endometrial cancer. Laparoscopy offers selected patients with endometrial cancer the potential benefits of shorter hospital stay, less need for blood transfusion, and decreased postoperative complications with a similar risk of intraoperative complications. Although morbid obesity is the most common risk factor for developing endometrial cancer, it is also the major limitation to successful laparoscopic surgical management. The rate of conversion from laparoscopy to laparotomy ranges quite widely between singleinstitution reports.
Despite the ambiguities in the law acne before and after 4 mg decadron order overnight delivery, incidents of health care discrimination are very few. There is currently proposed legislation that would broaden protection of individuals with increased genetic risk. Many argue against the legislation as unnecessary because there are currently no data to suggest that any discrimination exists. Again, the actual impact of these laws need to be tested in court and it is therefore difficult to predict exactly what effect these laws will ultimately have on genetic discrimination. Several important points should be considered here: (1) the actual incidence of genetic discrimination is exceedingly small, with few cases nationwide that address this issue, and (2) national sympathy clearly sides with those with the possibility of genetic disease. Nonetheless, part of counseling should include the possibility of discrimination with information gained from the test. It is the duty and obligation of the physician to inform the patient of the risks of a positive genetic test. However, there is also a duty of the physician to inform other family members who are at risk for the disease. However, there is a case litigated in 1996, Safer v Estate of Pack, in which an individual with familial adenomatous polyposis died from colon cancer. Genetic tests are unique in that they affect not only the individual, but may also affect the offspring and other relatives. This further confuses the issue of patient confidentiality and is an issue that will continue to be sorted out as time progresses and other genetic issues are defined by scientific discovery. This is an important part of the counseling process and is one of the reasons most centers recommend counseling before testing. This is defined as what is reasonable or what a reasonable physician should do for his or her patient. Genetic testing and counseling is quite new, and therefore clear standards have not been established. However, it is clear that it is important to take a family history and inform patients of diseases for which they may be at risk and offer testing for these diseases when available. Although there are no universally established standards, most specialties, such as the American Society of Clinical Oncology and the American Medical Association, have their own guidelines. Updates of the family history should be asked about at annual examinations because additions and new diagnoses may alter the initial recommendation regarding genetic testing. Indicators of a possible hereditary cancer syndrome include early age at diagnosis, multiple primary cancers (such as breast and ovarian cancer, or colon and endometrial cancer, or bilateral breast cancer), cancer in two or more close relatives on the same side of the family, and/or rare cancers such as male breast cancer or ureteral cancer. The counselor may expand upon the pedigree and request confirmatory documents such as pathology reports, operative reports, and/or death certificates. It usually takes 2 to 4 weeks for these results to return; the findings are then presented to the patient and the clinical recommendations are discussed. The American Society of Clinical Oncology offers guidelines for cancer predisposition testing that are followed by most cancer geneticists. Genetic testing is recommended when the individual has a personal history or family history suggestive of a cancer susceptibility syndrome, when the test can be adequately interpreted, and when the test result will influence medical management. The benefits of genetic testing include a more precise estimation of cancer risks for the individual and her family and the identification of those individuals who should participate in risk-reducing interventions. Families should be reminded, however, that the finding of a genetic mutation only predicts an elevated risk of cancer developing. A negative genetic test result does not guarantee that the individual will not get cancer, but rather that the person shares the general population risk rather than an elevated risk because of a hereditary predisposition. Most health insurance companies cover the costs of genetic testing when these guidelines are followed. Once a genetic abnormality is identified, the patient can be counseled regarding optimal future prevention, surveillance, and prophylactic surgery. When it is amplified, the gene is of prognostic significance in breast and ovarian neoplasms. Chromosome translocation Exchange of genes or a portion of genes between different. Codon A group of three nucleotides forming a basecoding message in the gene sequence. In ras genes, for example, the 12th, 13th, or 61st codon is often mutated, leading to oncogene activation. Cytoplasmic signal transduction molecules Proteins within the cytoplasm of cells responsible for transmitting signals from one event to the next event. Gene amplification the presence of multiple copies of a gene within a cell that is normally present in only two copies per somatic cell. An increased number of copies of an individual gene, usually a protooncogene, per cell. Gene rearrangement the process by which part or all of a gene is moved from its normal location in the genome to another site within the genome. Genomic imprinting An epigenetic modification of a parental allele of a gene that leads to differential expression of that allele. Growth factor receptors Proteins that interact with growth factors and transmit the growth signal to the cell. These are called polymorphisms and are often responsible for the heterozygous state. Informative A term used to describe the situation in which two homologous chromosomes from an individual can be distinguished from one another at a given locus; heterozygous is an alternative term. Myc protooncogenes the protooncogene family that includes c-myc, N-myc, L-myc, and R-myc.
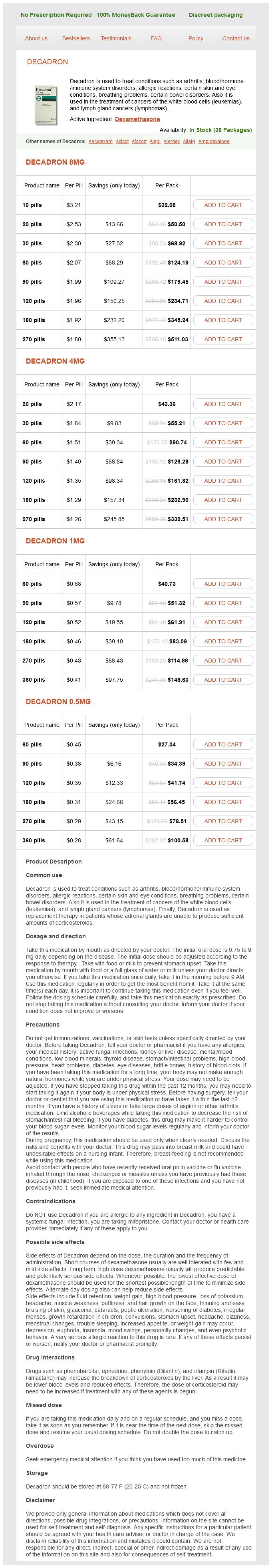
Decadron Dosage and Price
Decadron 8mg
- 10 pills - $32.08
- 20 pills - $50.50
- 30 pills - $68.92
- 60 pills - $124.19
- 90 pills - $179.45
- 120 pills - $234.71
- 180 pills - $345.24
- 270 pills - $511.03
Decadron 4mg
- 20 pills - $43.36
- 30 pills - $55.21
- 60 pills - $90.74
- 90 pills - $126.28
- 120 pills - $161.82
- 180 pills - $232.90
- 270 pills - $339.51
Decadron 1mg
- 60 pills - $40.73
- 90 pills - $51.32
- 120 pills - $61.91
- 180 pills - $83.09
- 270 pills - $114.86
- 360 pills - $146.63
Decadron 0.5mg
- 60 pills - $27.04
- 90 pills - $34.39
- 120 pills - $41.74
- 180 pills - $56.45
- 270 pills - $78.51
- 360 pills - $100.58
With one exception acne zinc buy decadron online from canada, the patients in the study by Young and colleagues were initially treated by conservative surgical procedures. Two of them received chemotherapy and two received radiation therapy postoperatively. Hysterectomies and salpingo-oophorectomies were performed as second operations in 8 cases; no residual tumor was found in any of these specimens. Adjuvant therapy has not been demonstrated to improve the outcome in this group of patients and is not recommended during pregnancy. Chemotherapy for Nonepithelial Ovarian Cancer During Pregnancy A recent literature review by Azim and colleagues identified 18 cases of nonepithelial ovarian malignancies treated with systemic chemotherapy during pregnancy. Other histologies reported included 3 cases of dysgerminoma, 3 cases of immature teratoma, 1 mixed germ cell tumor, and 1 SertoliLeydig tumor. Postnatal chemotherapyinduced adverse events were restricted to one baby who developed minor anemia and transient respiratory distress at delivery at the 35th week of gestation. This baby had been exposed to three cycles of carboplatin plus paclitaxel for a maternal dysgerminoma and the condition resolved quickly and the authors reported normal development at 20 months of follow-up. Epithelial Ovarian Cancer in Pregnancy Very few series of malignant ovarian carcinomas in pregnancy have been published. Reported in 2002, the most recent series contains nine ovarian cancers concurrent with pregnancy from Libya and Saudi Arabia. Among these cases were included seven epithelial cancers (four serous, two mucinous, one undifferentiated), one dysgerminoma, and one granulosa cell tumor. As expected, the latter two lesions occurred in younger women, aged 18 and 21 years, respectively. All seven women with epithelial cancers were multiparous (range 3-10), which is of some interest given the epidemiologic data suggesting increasing parity to be inversely related to the risk of developing ovarian carcinoma. None of the patients with more advanced disease who went on to receive chemotherapy did so during pregnancy. Thus fully six of seven women with epithelial ovarian cancers were diagnosed with early or locally advanced disease only, which does not reflect what is typically observed in the general population. It is quite certain that antenatal care including serial physical examinations and ultrasonography contributed to these early pick-ups. In those patients who present with metastatic disease manifest as malignant ascites and carcinomatosis, surgical exploration is warranted, 428 15. Once malignancy is confirmed and considered likely to be of ovarian origin, systemic chemotherapy during the second and third trimesters in a "neoadjuvant" fashion can be considered, with plans for interval cytoreductive surgery following delivery. The standard regimen for metastatic epithelial ovarian cancer in nonpregnant patients includes platinum-based chemotherapy. Regimens containing cisplatin alone and cisplatin plus paclitaxel, and even administration of a full six cycles of carboplatin and paclitaxel (the current standard among nonpregnant women), have been used during the second and third trimesters of pregnancy. Because there does not appear to be any significant risk to the fetus when these drugs are used in the second and third trimesters, pregnant patients diagnosed during these periods should be offered the opportunity to receive platinumbased therapy without terminating their pregnancy. Postpartum, the patient may return to the operating room to undergo definitive surgical staging or comprehensive tumor debulking. Because the prognosis for women with advanced carcinoma is poor, patients must be counseled regarding the realities of how much time they would have with their child when making decisions regarding pregnancy termination. It should be noted that there are at least two reports of an advanced-stage epithelial carcinoma of the ovary in which the uterus and pregnancy were preserved at 15 and 20 weeks of gestation. Patients were treated with six cycles of single-agent cisplatin or four courses of carboplatin plus paclitaxel followed by cesarean section and completion hysterectomy. One patient was disease free at a short follow-up of 6 months, whereas the other recurred in the pelvis at 24 months following delivery. This second patient underwent secondary cytoreduction and was re-treated with platinum-based therapy and has remained disease free at 42 months. Although some have advocated sparing the uterus if it appears to be uninvolved and the pregnancy is remote from term, this approach should be used with extreme caution when dealing with advanced-stage epithelial ovarian cancer for which the outcome remains exceedingly poor irrespective of pregnancy status. Chemotherapy for Epithelial Ovarian Cancer During Pregnancy Azim and colleagues have collected 20 patients from the literature who were treated with chemotherapy during pregnancy for epithelial ovarian cancer. The histologic subtypes included serous (n = 13), mucinous (n = 3), endometrioid (n = 2), clear cell (n = 1), and undifferentiated (n = 1). The chemotherapy regimens used included cyclophosphamide plus cisplatin (n = 5); single-agent cisplatin (n = 4); single-agent carboplatin (n = 3); paclitaxel plus carboplatin (n = 2); and cyclophosphamide, doxorubicin, and cisplatin (n = 2). There also was one case each of the use of the following regimens: cisplatin plus paclitaxel, cisplatin plus docetaxel, carboplatin plus cyclophosphamide, and single-agent paclitaxel. Seventeen of the patients received their first cycle during the second trimester and three in the third trimester. Sixteen patients delivered at week 34 or after, and 16 had experienced no pregnancy-related complications. There was 1 case each of intrauterine growth restriction, premature rupture of the membranes, and pre-eclampsia. Nineteen fetuses had a normal outcome, with 9 of these children reported to be normal at 1 year or greater follow-up. There was one neonatal death from multiorgan failure in a baby with congenital anomalies identified before starting cisplatin plus docetaxel at week 20. Although use of platinum derivatives appears to be feasible during the second and third trimesters, their administration does raise concern regarding the transplacental transfer of these drugs in late pregnancy, and the short- and long-term effects have not been wellstudied. Intraperitoneal chemotherapy in combination with intravenous chemotherapy has been associated with higher survival rates for patients with epithelial ovarian cancer. In patients opting for this type of therapy, delivery should be induced as soon as fetal pulmonary maturation can be documented before starting intraperitoneal therapy.