Diltiazem
General Information about Diltiazem
Diltiazem is usually used to deal with hypertension or high blood pressure. As a calcium channel blocker, it really works by stopping calcium from entering the muscle cells of the blood vessels, causing them to loosen up and allowing blood to move more easily. This reduces the drive towards the partitions of the arteries, serving to to lower blood strain. In addition, utilizing Diltiazem to treat hypertension can also cut back the risk of other complications such as heart attack and stroke.
When taken as prescribed, Diltiazem is usually well-tolerated with minimal unwanted aspect effects. However, some common unwanted aspect effects may embrace dizziness, headache, upset stomach, and flushing. In uncommon instances, extra extreme side effects similar to problem respiratory, chest pain, and swelling of the arms and feet may happen. It is essential to inform your physician when you experience any unwanted effects while taking Diltiazem.
It is also essential to notice that Diltiazem may work together with other medications, so it is essential to tell your physician about another medicines or supplements you are currently taking. This consists of over-the-counter medications, herbal cures, and nutritional vitamins. In addition, Diltiazem should be used with caution in individuals with certain pre-existing conditions such as liver or kidney illness, as properly as pregnant or breastfeeding ladies.
Apart from these main uses, Diltiazem may be prescribed for different circumstances similar to migraines and Raynaud’s Disease. Migraines are believed to be caused by the narrowing of sure blood vessels in the brain, and Diltiazem helps to widen these vessels, offering aid from migraines. Raynaud’s Disease, a uncommon condition that affects the blood vessels within the fingers and toes, can be handled with Diltiazem by enhancing blood move to those areas.
Another frequent use of Diltiazem is for treating angina, a condition where there is a reduction in blood flow to the center as a end result of narrowed arteries. This may cause chest pain or discomfort, and Diltiazem helps to alleviate these symptoms by relaxing the blood vessels and improving blood flow to the heart. By doing this, Diltiazem not solely helps to alleviate angina symptoms but additionally reduces the risk of coronary heart issues.
One of the main capabilities of Diltiazem is its ability to block the entry of calcium into the muscle cells of the center and blood vessels. This leads to the relaxation of those muscular tissues, which in turn helps to widen the blood vessels and improve blood move. By doing so, Diltiazem helps to scale back the workload on the guts and alleviates symptoms of circumstances corresponding to angina, hypertension, and arrhythmias.
In addition to those benefits, Diltiazem can additionally be used to treat sure types of arrhythmias, or irregular heartbeats. By regulating the heart’s rhythm, Diltiazem helps to enhance the heart’s efficiency and scale back the risk of serious problems such as coronary heart failure. It is also used in combination with different drugs to handle circumstances corresponding to atrial fibrillation, a standard heart rhythm disorder.
Diltiazem is a widely prescribed treatment that belongs to the class of calcium channel blockers. It works by relaxing the muscular tissues of the center and blood vessels, making it a popular selection for treating varied coronary heart and circulatory circumstances.
In conclusion, Diltiazem is a commonly prescribed medication for various heart and circulatory situations. Its capability to improve blood move and regulate the heart’s rhythm makes it an essential medicine within the administration of hypertension, angina, and arrhythmias. As with any treatment, it could be very important follow your doctor’s directions and inform them of any potential unwanted aspect effects. With the help of Diltiazem, individuals can lead a healthier and more active way of life.
Several types of bone or cage constructs, including titanium and carbon fiber cages, femoral bone dowels, or impacted bone wedges, can be placed into the intervertebral space symptoms 9 dpo diltiazem 180 mg purchase fast delivery. Although the literature on this type of procedure may describe removal of only the medial facets, more surgeons find that the whole facet or most of the facet needs to be removed to provide adequate exposure and protection of the nerve root and thecal sac. Because this approach results in some posterior instability, it should be combined with some form of posterior instrumentation such as pedicle screws. Prevention of nerve root sleeve and dural tears requires adequate removal of the posterior elements. Because of the nature of the implants and the difficulty in obtaining postoperative imaging. Another problem with use of nonbiodegradable spacer devices is the fact that the body forms a "protective" capsule around all foreign bodies that gets larger over time, thereby resulting in further impingement on the diameter of the fusion mass traveling vertically in the spacer, which reduces the strength of the fusion mass. This may explain why many studies have shown better outcomes earlier in the series and a decrease in successful outcomes more than 2 years after surgery. The use of various technologic advances, such as stereotactic navigation and neurophysiologic monitoring, can help improve accuracy. A thorough understanding of the types of problems encountered with a given procedure or approach makes the surgeon more wary and probably reduces the incidence of such complications. Newer techniques are being developed to improve exposure with lower morbidity, and over time it is likely that many of the procedures now commonly performed will be replaced by less invasive and more effective ones as our understanding of the underlying processes progresses. The value of somatosensory and motorevoked potentials in predicting and monitoring the effect of therapy in spondylotic cervical myelopathy: prospective randomized study. Unilateral blindness due to patient positioning during cervical syringomyelia surgery: unilateral blindness after prone position. How accurately do novice surgeons place thoracic pedicle screws with the free hand technique Prophylaxis for deep venous thrombosis in neurosurgery: a review of the literature. Implementation of evidence-based practices for surgical site infection prophylaxis: results of a pre- and postintervention study. Anterior tibial compartment syndrome as a positioning complication of the prone-sitting position for lumbar surgery. Motor-evoked potential monitoring for intramedullary spinal cord tumor surgery: correlation of clinical and neurophysiological data in a series of 100 consecutive procedures. Preoperative laryngeal nerve screening for revision anterior cervical spine procedures. Visual loss in a prone-positioned spine surgery patient with the head on a foam headrest and goggles covering the eyes: an old complication with a new mechanism. Anti-epileptic drugs for preventing seizures following acute traumatic brain injury. Prevention of positional brachial plexopathy during surgical correction of scoliosis. Femoral artery ischemia during spinal scoliosis surgery detected by posterior tibial nerve somatosensory-evoked potential monitoring. Pedicle Screw Fixation the use of pedicle screw fixation has significantly increased fusion rates over those with noninstrumented fusions. The major risks are related to misplacement of the screws, fracture of the neural elements being stabilized, injury to neural and vascular structures, and infection or poor wound healing. Understanding the biomechanical parameters and indications can reduce the risk for surgical misadventure. Pedicle screws can be placed by relying only on anatomic parameters to determine the entry point and angulation, but for surgeons who wish to have confirmatory assistance, several imaging and image-guided techniques are available, as discussed previously. The practice at our institution is to not place them at L5-S1 because of stress concentration or when significant spondylolisthesis is present. During the first half of the 20th century, several investigators had measured ventricular fluid pressure in a small number of patients. Most practitioners use anatomic landmarks (freehand technique) to insert the ventricular drain into the lateral ventricle with the tip in the foramen of Monro. In a recent survey of practicing neurosurgeons and residents, the success rate of cannulation of the ventricle was just 82%, even in the hands of practicing neurosurgeons. Hemorrhage rates ranging from 0% to 15% have been reported in the literature, with an average rate of 1. However, most studies are retrospective in nature and often do not have enough statistical power to detect small absolute differences in the incidence of infection. Sandalcioglu and Stolke reported that there was a significant difference in infection rate (83% versus 17%) for catheters that were tunneled less than 5 cm subcutaneously versus catheters that were tunneled more than 5 cm, respectively. Prophylactic antibiotics can be given periprocedurally only or administered during the entire duration that the catheter is in place. In a large retrospective study, Alleyne and colleagues did not find any significant difference in infection rates between the two groups. This was especially the case during the early study period because health care personnel were not familiar with the device and proper precaution in handling and securing the device was not taken. The fiberoptic cables are delicate and can be broken easily during transport or with patient movement. As many as 10% to 23% of the fiberoptic devices had a mechanical malfunction because of breakage of cable, dislocation of the probe, or other unknown factors. The subdurally placed monitor is marketed as a postcraniotomy monitor, though there are no large-scale clinical studies to evaluate its accuracy. In addition, the Camino fiberoptic device can also be inserted with a temperature probe or brain tissue oxygen probe. The most commonly used technique involves insertion of the monitor into the right frontal region, although it is possible to insert the probe into a region with pathology as well.
Generally, when the shunt operations are segmented out, the wound infection rate falls into the expected range medications quiz 60 mg diltiazem purchase with amex. EvaluatingCumulativeEvidence It is a fundamental tenet of science that a fact is not a fact until it has been replicated. Single publications are rarely sufficient justification to adopt a new diagnostic or therapeutic strategy. The results of several similar investigations must frequently be combined in the form of a meta-analysis or systematic review as discussed earlier to lead to an appropriate conclusion before changing practice. In matters of determining the best evidence of prognosis, optimal diagnostic techniques, and best therapeutic interventions, the authority-driven expert opinion review is no longer the gold standard. When the formal process of systematic review and meta-analysis is applied, different reviewers should arrive at fundamentally similar conclusions. Accumulated evidence may also be summarized in a practice parameter development process. Many professional organizations have participated in the development of evidence-based practice parameters (sometimes called guidelines). When the principles of critical analysis, systematic review, and meta-analysis have been applied, true evidence-based practice parameters should result. Such practice parameters provide a tremendous time savings for the busy practitioner. Neurosurgeons who wish to provide the best care for their patients must become facile with the tools required to access the rapidly growing base of high-quality evidence regarding neurosurgical practice. Because this progress in neurosurgery is so greatly information based and the rate of information change is so high, it will not be possible to remain current with just paper technology. Centralized databases available for describing primary brain tumor incidence, survival, and treatment: Central Brain Tumor Registry of the United States; Surveillance, Epidemiology, and End Results; and National Cancer Data Base. International Study of Unruptured Intracranial Aneurysms Investigators [published erratum appears in N Engl J Med. Journal articles are increasingly out of date at the time of publication because of the circulation of results in the press and on the Internet. Evidence-based practice will be Webbased practice for the foreseeable future until supplanted by even more rapid and accessible methods of communicating large amounts of information. Individual neurosurgical practitioners should develop a collection of Web-based tools that are readily accessible wherever they practice (office, hospital, and home) and become accustomed to accessing them many times every day. Discrepancies in diagnoses of neuroepithelial neoplasms: the San Francisco Bay Area Adult Glioma Study. Surgery for primary supratentorial brain tumors in the United States, 1988 to 2000: the effect of provider caseload and centralization of care. In this chapter a clinically oriented review is presented with emphasis on mechanisms that underlie altered consciousness at the neuronal "circuit" level. A brief taxonomy of altered states of consciousness is presented, followed by a discussion of general strategies to assess patients and formulate a diagnosis and prognosis. Finally, the potential contribution of new neuroimaging modalities to the diagnostic assessment of patients with disorders of consciousness is briefly reviewed. Although many challenges currently limit the clinical application of these techniques, greater future roles may be anticipated. Altered consciousness is a most common finding in patients evaluated by a consulting neurosurgeon or neurologist. The development of a comprehensive differential diagnosis, treatment plan, and prognosis for altered consciousness is well beyond the scope of a single book chapter (instead, see Posner and colleagues1). Here, emphasis is placed on conceptualizing neurological disorders of consciousness and formulating an organized and physiologically based approach to the general set of problems. A systematic approach to evaluate patients with altered consciousness requires a foundation of the basic principles that underlie maintenance of the normal wakeful conscious state. Fragmentary elements of specific neuropsychological components are evident in these syndromes. For example, fragments of attentional function are evidently preserved in all forms of akinetic mutism, with varying levels of impairment in other components (see later). Similarly, purposeless intentional movements can occur in patients with hyperkinetic mutism or as partially integrated and organized goal-directed sensorimotor activity in those with complex partial seizures or delirium (see Schiff and Plum2 for a more extended review). Complex brain injuries typically produce a mix of the clinical features observed in these classic syndromes. Here we focus on the classification of global disorders of consciousness most frequently encountered and related to each other as recovery evolves after severe brain injury. Comatose patients remain motionless in an eyes-closed state without spontaneous periods of eye opening or change of state with vigorous stimulation. Although effortful stimulation of a comatose patient may produce a grimace in response to painful stimuli or stereotyped withdrawal movements of the limbs generated by spinal reflexes, these movements lack localization of the source of external stimulation and the organized sequence of movements associated with purposeful avoidance. Patients in deep levels of coma typically do not exhibit primitive reflex responses. By definition, the term coma implies that the state has endured for at least 1 hour and in some clinical operational definitions for at least 6 hours. Nonetheless, coma is invariably a transient condition that if uncomplicated by concurrent systemic illness, sedation, or other similar factors, typically does not persist beyond 10 to 14 days. Human conscious brain states are characterized by several neuropsychological components, including arousal, attention, intention, memory, awareness, and mood-emotion. A clinically oriented view of global disorders of consciousness suggests a roughly hierarchical organization of these components. Although this finding of extensive thalamic neuronal loss can be seen after both diffuse axonal injury from brain trauma and oxygen deprivation associated with cardiac arrest, widespread neocortical neuronal death is common only with cardiac arrest (64% versus 11%7).
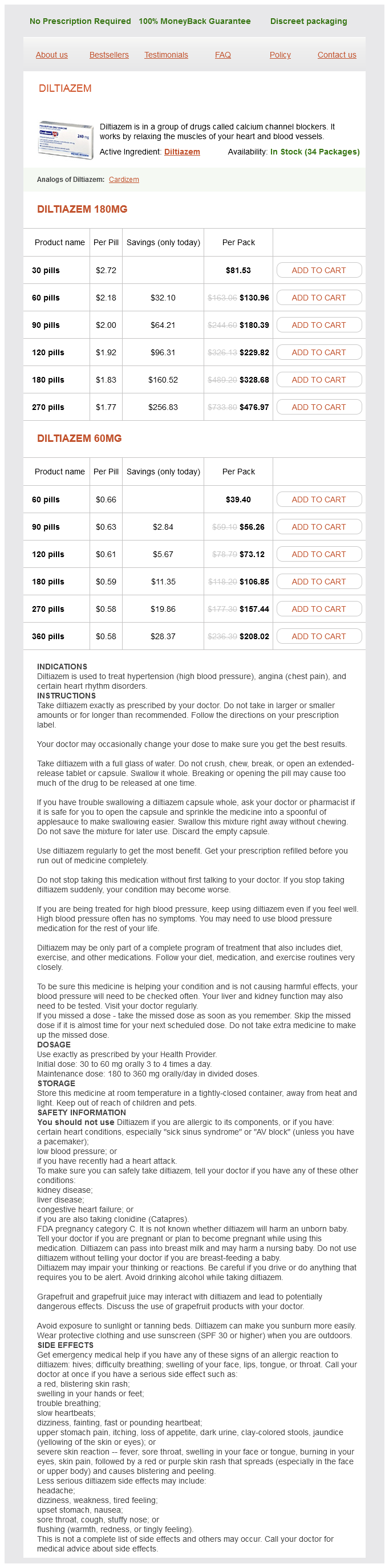
Diltiazem Dosage and Price
Diltiazem 180mg
- 30 pills - $81.53
- 60 pills - $130.96
- 90 pills - $180.39
- 120 pills - $229.82
- 180 pills - $328.68
- 270 pills - $476.97
Diltiazem 60mg
- 60 pills - $39.40
- 90 pills - $56.26
- 120 pills - $73.12
- 180 pills - $106.85
- 270 pills - $157.44
- 360 pills - $208.02
Complex partial seizures are characterized by alteration of awareness and amnesia for at least a portion of the seizure treatment deep vein thrombosis 180 mg diltiazem with mastercard. Partial seizures may include signs or symptoms correlating with activation of any brain region-specifically, motor, autonomic, somatosensory, special sensory, or psychic, as elegantly demonstrated by Drs. Penfield and Jasper in their intraoperative stimulation studies of persons with epilepsy. Generalized seizures are "those in which the first clinical changes indicate initial involvement of both hemispheres. The generalized epilepsies, as opposed to generalized seizures, are often divided into primary (idiopathic) and secondary (symptomatic). Cerebrovascular disease is the most frequently identified cause of epilepsy, followed by developmental disorders, head trauma, brain tumor, infection, and degenerative disorders. Similar to seizure classifications, the epilepsies are divided into two main categories: localization related and generalized. Hence, factors that influence the risk for seizure recurrence will be discussed as they relate to the diagnosis and especially to the decision for treatment to prevent subsequent seizures. In this situation, the physician must use diagnostic tests judiciously to make a definitive diagnosis and exclude progressive or potentially life-threatening disorders expeditiously. If a cardiac cause is suspected, appropriate testing or referral should be requested. ApproachtotheFirstSeizure Acute Evaluation A seizure after which mental status and the results of neurological examination quickly return to normal is not typically an emergency; this clinical situation is discussed in the next section. If mental status and the neurological examination have not normalized within minutes after the event appears to end, however, two questions must be answered as rapidly as possible. First, is there an underlying medical or neurological condition that requires immediate treatment These two questions must be addressed whether the patient is in an emergency room, intensive care unit, or ambulatory setting. The urgent evaluation should include serum glucose, sodium, urea nitrogen, creatinine, and calcium and hepatic enzyme concentrations. A toxicology screen is necessary if no other cause is readily identified, especially for ethyl alcohol, cocaine, amphetamines, benzodiazepines, opioids, phencyclidine, tricyclic antidepressants, and antipsychotic drugs. If the patient has a possible history of seizures, anticonvulsant medications should be identified and serum concentrations determined. Decreased responsiveness or unusual behavior may be the only indication of a persistent seizure. A thorough history of potential clues to seizure occurrences, supplemented by reports from family, friends, and coworkers, is required to optimize care. Another approach to defining the spectrum of the phenomenology of seizures is to emphasize that any experience that the brain can generate could be a component of a clinical seizure. The patient is often aware of the initial evolution of a seizure, which is commonly called an aura. Because an aura can define the early experience of a seizure, it may provide reliable clues to the region of onset within the brain. Auras, or simple partial seizures, are often classified by the type of symptoms experienced during the ictal event. For example, the most common symptoms in patients with temporal lobe epilepsy are categorized as visceral/abdominal, psychic, autonomic, somatosensory, special sensory, and visual. The visceral symptoms may be an ascending sense of constriction or warmth in the abdominal region, which is sometimes described in the literature as an "epigastric rising sensation. Other psychic symptoms include a sense of dissociation from the environment, depersonalization, or a sense of never being in a familiar place (jamais vu). Visual symptoms may be formed or unformed hallucinations or visual distortion such as change in size or apparent speed of Seizure Evaluation in the Ambulatory Setting A patient being evaluated in an ambulatory setting with a history of a possible seizure is a common clinical situation. An acute evaluation such as that just described may have been performed in an emergency department before referral. If metabolic assessment was not performed previously, the serum studies described in the previous section should be considered. The subsequent evaluation aims at answering four questions: (1) Was the paroxysmal change in behavior or symptom a seizure A complete history of the event from both the patient and a witness is frequently the most helpful diagnostic tool. It is important to understand that seizures arising from the region of the visual cortex my not have visual auras and that visual auras can occur with seizures beginning in areas other than the occipital lobe. An uncommon but well-described visual symptom is the sensation of watching a movie, which may localize to the mesial temporal region. Somatosensory auras are typically positive, such as a tingling or electrical sensation, and are contralateral to a parietal epileptogenic region; however, bilateral and ipsilateral somatosensory auras have been reported in patients with insular42,43 and mesial frontal seizures. For example, tuberous sclerosis complex has a prevalence of epilepsy of 78% and is characterized by facial angiofibromas, hypomelanotic macules, shagreen patches, ungual fibromas, and retinal hamartomas. ClinicalSemiology Specific behavioral changes can be used to localize brain regions involved in a seizure. Complete behavior arrest is reportedly more frequently associated with temporal lobe than with frontal lobe seizures. Imaging of neoplastic and vascular lesions is critically important for many persons with epilepsy, but specific aspects of these abnormalities are reviewed in other chapters. An interesting, but frequently overlooked clinical finding in temporal lobe epilepsy is asymmetric facial movement with spontaneous smiling. It is present on the side of the face contralateral to the epileptogenic region in more than 25% of persons with mesial temporal lobe epilepsy. The presumed mechanism of this finding is amygdala dysfunction resulting in an abnormal emotional motor response. Accurate diagnosis and treatment are therefore of the utmost importance at the initial evaluation.