Divalproex
General Information about Divalproex
There are various types of epilepsy, and Depakote has shown to be effective in treating various kinds of seizures. It is commonly prescribed for generalized tonic-clonic seizures, that are characterised by loss of consciousness, stiffening of muscle tissue, and jerking actions. This type of seizure can be very intense and can lead to severe injuries. Depakote helps to reduce the frequency and intensity of those seizures, thereby enhancing the quality of life for people with epilepsy.
This medication is also used to deal with absence seizures, which involve a short lack of consciousness with minimal actions. It has been proven to be effective in up to 80% of people with absence seizures, significantly reducing the number of episodes. Depakote can be used for partial seizures, which contain one part of the brain and might trigger uncommon sensations, movements or behaviors. It can be used alone or in combination with other drugs to handle these types of seizures.
Divalproex is a drugs that falls underneath the class of anticonvulsants, also referred to as anti-epileptic medication. It is mostly recognized by its brand name Depakote, and is broadly prescribed for the treatment of varied kinds of seizure problems. Divalproex has been accredited by the United States Food and Drug Administration (FDA) since 1983, and continues for use as an efficient therapy option for people with epilepsy.
Like any medication, Depakote could cause side effects, however not everybody experiences them. Common unwanted facet effects could embrace dizziness, drowsiness, nausea, vomiting, and diarrhea. More serious unwanted aspect effects, although rare, can embrace liver issues and low platelet count, which might result in simple bruising or bleeding. It is essential to report any new or persistent side effects to the physician for proper administration.
Depakote comes in varied forms, together with tablets, delayed-release tablets, extended-release tablets, and sprinkle capsules. The dose prescribed could vary relying on the kind of epilepsy, the severity of seizures, and the individual’s age and weight. It is important to comply with the dosage recommendations offered by the physician and not to change the dose with out consulting them.
Epilepsy is a neurological disorder that impacts approximately three.4 million individuals in the United States alone. It is characterized by recurring seizures, that are sudden, uncontrolled electrical disturbances in the brain. These seizures can differ in kind and severity, from mild to severe, and may have a significant influence on a person’s day by day life. They can even have severe penalties, similar to falls, injuries, and even dying.
Depakote works by growing the degrees of a chemical called gamma-aminobutyric acid (GABA) within the brain. GABA is a neurotransmitter that helps to settle down the overexcited nerve cells within the mind, thus decreasing the probability of seizures. This treatment also works by lowering the activity of glutamate, another neurotransmitter that's answerable for stimulating nerve cells. These combined actions of Depakote assist to stabilize the electrical exercise in the brain and stop seizures.
In conclusion, Depakote (divalproex) is a broadly prescribed treatment for the treatment of epilepsy, particularly for generalized tonic-clonic, absence, and partial seizures. It has also proven to be efficient in managing bipolar disorder. However, like all medication, it should be taken as prescribed and underneath the supervision of a healthcare professional. With proper use, it could considerably enhance the quality of life for individuals residing with seizures.
Apart from treating epilepsy, Depakote can be prescribed for the treatment of bipolar disorder. Bipolar disorder is a persistent mental health condition that is characterized by excessive mood swings, starting from manic episodes of high power to depressive episodes of low mood. Depakote works by stabilizing the mood swings, making it a valuable remedy choice for this situation.
Congenital Chagas disease in Córdoba medications and mothers milk 2014 buy discount divalproex on line, Argentina: epidemiological, clinical, diagnostic and therapeutic aspects. In vivo selection of a population of Trypanosoma cruzi and clones resistant to benznidazole. Molecular characterization of cytosolic and mitochondrial tryparedoxin peroxidase in Trypanosoma cruzi populations susceptible and resistant to benznidazole. Urban outbreak of acute Chagas disease in Amazon Region of Brazil: four-year follow-up after treatment with benznidazole. Experimental chemotherapy against Trypanosoma cruzi infection: essential role of endogenous interferon-gamma in mediating parasitologic cure. Population pharmacokinetics of benznidazole in adult patients with Chagas disease. In vivo susceptibility to benznidazole of Trypanosoma cruzi from the western Brazilian Amazon. Long term outcomes of treating chronic Chagas disease with benznidazole versus no treatment. It was shown to be the most active and least toxic of this group of agents in preclinical studies, and was evaluated in clinical trials in the 1960s and subsequently marketed for use in Chagas disease in Latin America in the late 1960s and early 1970s. In addition, the drug is being evaluated as an investigational antineoplastic agent. Although the manufacture of nifurtimox was halted in 1997, production was recommenced in 2000, primarily to fulfil commitments to provide it for compassionate use and clinical trials in T. Reduction of the nitro group of nifurtimox occurs within the trypanosome and is essential for its activity (see below under 3, Mechanism of drug action). Chagas disease is endemic in many Latin American countries, and it was estimated that 5. Transmission is predominantly via the arthropod vector (triatomid bugs), which inoculate feces containing the infective metacyclic trypomastigote form of T. Infection can also occur congenitally, via blood or blood product transfusion or organ transplantation, via ingestion of food contaminated with triatomid feces, and rarely via percutaneous exposure to T. Reactivation of clinically inapparent infection can occur in immunosuppressed patients. An experimental model for the study of potential mechanisms of drug resistance in acute T. However, this test is slow and labor intensive, and is available only in specialized research laboratories. Moreover, because there is a paucity of pharmacokinetic and pharmacodynamic data on nifurtimox, clinical outcomes of drug therapy are difficult to assess. This variability occurs in isolates from sylvatic reservoirs and vectors as well as in isolates from populated regions where nifurtimox is used in the treatment of Chagas disease. Furthermore, there is evidence suggesting that rates of parasitologic clearance following nifurtimox and benznidazole therapy is higher in regions where T. However, because clinical details are scant in these reports, it is difficult to determine whether failure of nifurtimox therapy is due to antimicrobial resistance or is the result of other factors, such as suboptimal adherence to therapy or patient-to-patient variability in pharmacokinetic and pharmacodynamic parameters. Furthermore, levels of intracellular free thiols negatively correlate with susceptibility of several T. Acute (first-stage) infection involves the bloodstream and lymphatic system, and often goes unrecognized. However, some patients develop a noticeable lesion at the site of the bite (trypanosomal chancre). Second-stage infection is characterized by development of progressive neurologic dysfunction caused by central nervous system invasion by the parasite, and is uniformly fatal without treatment. In vitro synergy and antagonism Although nifurtimox is currently used in combination with other antitrypanosomal agents for treatment of T. As with other nitro-containing drugs, the metabolic reduction of the nitro group is considered to be critical for the activity of nifurtimox, as well as being responsible for many of its adverse effects. Until recently, it was believed that trypanosomes are relatively deficient in enzymes to protect themselves against "oxidative stress" generated by reactive oxygen species. This work has indicated that alkylation of cellular macromolecules by metabolites of nifurtimox and depletion of intracellular levels of thiol "scavenger molecules". Marked morphologic changes and reduced numbers of bloodstream trypomastigotes can be demonstrated shortly after the administration of nifurtimox (Haberkorn and Gömnnert, 1972). While the manufacturer recommends a three times a day dosing regimen, both twicedaily or four times a day regimes are recommended by some authorities. For adults (and children 17 years of age) the dose recommended by the manufacturer is 810 mg/kg/day in three divided doses. The manufacturer recommends that the dose be administered to breastfeeding infants and small children by pulverizing the tablets and mixing the powder with a small amount of food, which is then given before the meal (Lampit Product Information). No specific information is available on the use of nifurtimox in premature neonates. Bioavailability Pharmacokinetic studies of radiolabeled nifurtimox in rats and dogs suggest that the drug is well absorbed from the gastrointestinal tract following oral administration (Duhm et al. Although the manufacturer recommends dosing after meals, there are no published data on the effects of food on the pharmacokinetic profile of nifurtimox in humans (Lampit Product Information). Following the administration of a single 15-mg/kg oral dose of nifurtimox to healthy human volunteers, the Cmax was 0. When administered at a dose of 5 mg/kg three times daily, serum levels of nifurtimox 3 hours following ingestion of the dose were between 0. Although there is no evidence in animal models that nifurtimox is teratogenic, mutagenic and carcinogenic effects have been demonstrated, and chromosomal changes have been described in children who have received nifurtimox (see below under 6, Adverse reactions and toxicity). Nifurtimox appears in breast milk following the administration of the drug to lactating animals (Castro et al.
More recent rat studies have shown that even at the highest tolerated dose of suramin medicine interaction checker buy 250 mg divalproex with mastercard, trypanosomal growth continues exponentially in the bloodstream for at least 6 hours (Fairlamb and Bowman, 1980). Suramin inhibits the activity of many enzymes that probably have no relation to its antiparasitic effect, including hyaluronidase, urease, hexokinase, fumarase, and trypsin (Pepin and Milord, 1994). However, uptake by cells exceeds the rate that would be expected by this alone (Fairlamb and Bowman, 1980; de Koning, 2001). In a recent study investigating suramin targets, it was found these were restricted to proteins from the surface proteome and endosomal system (Zoltner et al. Adults Suramin is prepared as a powder in 1 g vials and reconstituted with sterile water for intravenous administration to a concentration of 10%. It should not be administered intramuscularly or subcutaneously, as it causes severe inflammation and necrosis (Pepin and Milord, 1994). The duration of administrations should not exceed 30 minutes, as the drug degrades rapidly (Pepin and Milord, 1994). Patients should be under medical supervision and the drug should be administered in hospital, with full supportive care available, including adrenaline (epinephrine), parenteral 3. The mechanism of action responsible for its trypanocidal action is not well understood. The drug has complex cellular pharmacology, possibly explaining the diverse range of 4. Mode of drug administration and dosage 3229 antihistamines, and corticosteroids. Because of the risk of a rare but severe idiosyncratic reaction, it is recommended that a test dose of 100200 mg suramin be administered in 2 ml of sterile water for injection before administering the full treatment dose. A recommended method of administration is to inject a few microliters of the test dose, then wait at least 1 minute; then inject the next 0. An alternate protocol included giving 1 g as a weekly dose up to a total of 4 g (Voogd et al. Suramin is no longer recommended for onchocerciasis because of the high incidence of severe reactions, especially in patients with ocular disease, owing to the risk of serious ocular complications such as optic atrophy (Voogd et al. Newborn infants and children There are no studies of the use of suramin in children or infants (Edwards and Breckenridge, 1988). As no adequate pharmacologic studies have been conducted in this patient group, it is essential to observe carefully for any signs of drug toxicity, including regular clinical and biochemical monitoring. This protocol involves giving 5 mg/kg on day 1, 10 mg/kg on day 3, followed by 20 mg/kg on days 5, 11, 17, 23, and 30. Suramin is sometimes used as a lead-in therapy prior to melarsoprol for second-stage disease caused by T. This regimen is used in an attempt to reduce the risk of reaction to melarsoprol, perhaps by reducing or eliminating circulating trypanosomes from the blood. Another theory proposed to explain the putative protective effect of suramin is that it inhibits activity of the P-glycoprotein transporter of the bloodbrain barrier, thus preventing removal of the second-stage drug from the brain (Enanga et al. There is a paucity of evidence to support this strategy, and this regimen is not universally recommended (Burri and Brun, 2009; Krishna and Stich, 2016). The regimen for suramin administration before melarsoprol treatment for second-stage disease is shown in Table 194. Pregnant and lactating mothers Suramin has not been studied in pregnant women, but animal studies have shown that suramin may cause birth defects or death of the fetus. For a potentially fatal infection such as trypanosomiasis, it has been recommended that suramin be used during pregnancy only when there is no suitable alternative available. This has been demonstrated in rats with histopathologic changes seen in the cortex and medulla after prolonged administration (Soldani et Table 194. A report of 15 patients who received suramin as part of a phase I study for prostate cancer demonstrated mild hypophosphatemia in all 15 patients by day 42, and prolonged phosphatemia in two patients who developed a full Fanconi syndrome (Rago et al. In patients with pre-existing renal impairment, there are no data to guide treatment decisions. Suramin is likely to worsen pre-existing impairment, but given the lack of suitable alternatives, this consideration should be weighed against the overall condition of the patient. Bioavailability Suramin is not absorbed when given orally, partly because it forms stable complexes with protein (Voogd et al. It causes intense irritation and necrosis when given intramuscularly, so it must be given intravenously (Edwards and Breckenridge, 1988; Voogd et al. No patient had a peak plasma concentration greater than 300 mg/ml, the level above which serious hematologic and neurologic toxicity is reported to be more likely (Stein et al. After the last dose, the plasma half-life was 4454 days-among the longest of half-lives to be recorded for a drug in humans. In a study of six patients from Ghana with onchocerciasis who were administered radiolabeled suramin, the mean volume of distribution was 98. Early reports on the pharmacokinetic properties of suramin indicated large inter-subject variability in pharmacokinetics (Pepin and Milord, 1994), a finding that has been confirmed in subsequent studies (Eisenberger and Reyno, 1994; Chijioke et al. However, this variability may be significant for patients experiencing toxicity; for example, when a prolonged elimination half-life in the order of 1028 days was There are no specific recommendations for the use of suramin in the presence of hepatic impairment. Suramin is known to cause liver function derangement, including elevated bilirubin and hepatic aminotransferases (Hawking, 1978; Voogd et al. At present, this presents a clinical dilemma, as there are no less toxic alternatives for hemolymphatic stage T. Adverse reactions and toxicity 3231 observed in one patient (renal function not reported) (Chijioke et al. The drug is widely distributed in tissues, with a concentration similar to plasma, with the exception of the brain. Suramin does not cross the bloodbrain barrier in sufficient quantities to reach trypanocidal levels (Hawking, 1978). This is thought to be a result of its large molecular size, its high negative charge at physiologic pH.
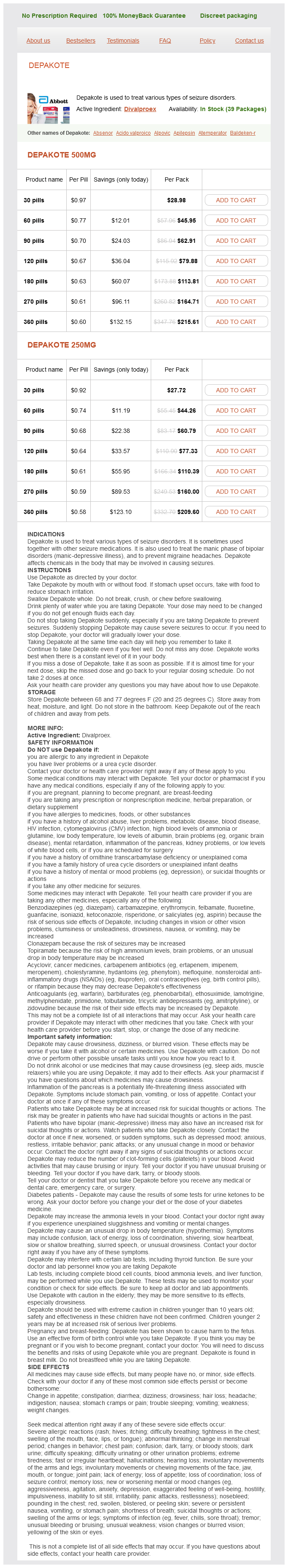
Divalproex Dosage and Price
Depakote 500mg
- 30 pills - $28.98
- 60 pills - $45.95
- 90 pills - $62.91
- 120 pills - $79.88
- 180 pills - $113.81
- 270 pills - $164.71
- 360 pills - $215.61
Depakote 250mg
- 30 pills - $27.72
- 60 pills - $44.26
- 90 pills - $60.79
- 120 pills - $77.33
- 180 pills - $110.39
- 270 pills - $160.00
- 360 pills - $209.60
Praziquantel was found to be active against a wide range of trematode and cestode helminths (Andrews et al medicine head buy divalproex pills in toronto. The drug was initially developed for veterinary use before being developed for use in humans. Praziquantel is currently the mainstay of treatment for schistosomiasis and opisthorchiasis. Praziquantel was the first drug active against Schistosoma japonicum, and additionally has become the mainstay of therapy for African schistosomiasis caused by S. Cure rates of 100% have been reported with single-dose therapy of clonorchiasis and opisthorchiasis (Horstmann et al. A detailed study has demonstrated that the adult worms of Clonorchis sinensis, Opisthorchis viverrini, S. However, all of these parasites are successfully eliminated by praziquantel in vivo (Horstmann et al. Praziquantel has recently been demonstrated to have some activity against the European liver fluke (Opisthorchis felineus) in an animal model (Pakharukova et al. Praziquantel has documented efficacy against a wide variety of taenid cestodes in both veterinary and human medicine. Single-dose therapy is reliably effective against intestinal infections caused by cestodes of the genera Taenia, Hymeno lepis, and Diphylobothrium (de Silva et al. Praziquantel has some efficacy in the treatment of viable subarachnoid and ventricular cysticercosis cysts (Garcia et al. It also has no activity against filarial parasites, such as Mansonella perstans (Bregani et al. Emerging resistance and cross-resistance Praziquantel remains the mainstay intervention for both individual therapy of schistosomiasis and community control programs. The potential for the development of resistance is therefore real, particularly in some regions of Africa where control programs in areas with intense transmission have resulted in heavy population exposure to the drug. Although a number of reports of praziquantel resistance have been published (Fallon and Doenhoff, 1994; Fallon et al. That is, within any infected individual, worms may range in age from new schistosomulae to worms that could have been present within the host for decades (Ross et al. As noted above, praziquantel is not active against juvenile worms aged between 3 and 26 days post-infection (Xiao and Catto, 1989). There is currently no technology available to differentiate between treatment failure due the presence of a "young" (326 days old) infection and actual drug resistance. Thus, those patients with numerous reinfections in regions of high transmission are likely to have worms of mixed ages, with a proportion of their worm burden aged 326 days at the time of treatment. This may explain why those with heavy or recent infections are less likely to be cured with single-dose therapy, as was described in northern Senegal (Fallon et al. Second, praziquantel therapy does not confer resistance to reinfection (McManus, 1999; McManus, 2005; Fenwick and Webster, 2006). Therefore a proportion of apparent treatment failures may be due to reinfection depending on the timing of the "test of cure," and also on regional intensity of transmission (Gryseels et al. Notwithstanding the above discussion, there is some laboratory evidence indicating that praziquantel-tolerant worms may have altered tegumental architecture-potentially limiting the effect of praziquantel (William et al. Praziquantel resistance can also be induced in the laboratory following exposure of miracidia within Biomphalaria sp. Some putatively-resistant laboratory-passaged strains have evolved in the absence of praziquantel-induced selective pressure (Cioli et al. Follow-up studies of subjects living in high-transmission regions in rural China who have had numerous treatment courses of praziquantel have demonstrated preserved efficacy (90% cure rates) compared with first-time treatment in new endemic regions (Yu et al. Multiple treatment courses over 10 or more years have been administered to many communities in regions of intense transmission for all three major pathogenic schistosomes in North Africa and China (Yu et al. This is an important issue, as praziquantel is the only readily deployed antischistosomal drug available. Because worm reproduction is sexual with a relatively long generation time, if resistance does develop in human populations, it is likely to take many years to become an important clinical and public health issue (King et al. Trematode Ca2+ channels appear to play a critical role in the mode of action of praziquantel (Ruenwongsa et al. Schistosomes express two Ca2+ channel beta subunit subtypes, a structurally conventional betasubunit, and a variant beta-subunit (Ca-var), with differing functional properties. Susceptibility to praziquantel appears to be conferred by drug action on the Ca-var subunit, and the effect appears to be inhibited by calcium channel blockers, such as nifedipine, in vitro (Pica-Mattoccia et al. Conversely, coexpression of Ca-var in mammalian cells with the appropriate alpha1-subunit confers praziquantel susceptibility to these otherwise resistant cells (Kohn et al. Likewise, deletion of two serine residues at positions 225 and 235 in the constitutive rat beta2a Ca-channel subunit abolishes normal interaction with the alpha1-subunit, and confers praziquantel susceptibility on the rat cells (Kohn et al. There is evidence demonstrating that Ca-var orthologus are found in other praziquantel-sensitive platyhelminths, such as the pork tapeworm Taenia solium (Jeziorski and Greenberg, 2006). These variant beta-subunits may therefore represent a platyhelminth-specific gene family. Immune-mediated worm killing may also play a significant role in the in vivo activity of praziquantel. The efficacy of the drug as determined by worm burden reduction can be reduced by up to 80% in B celldepleted mice (Brindley and Sher, 1987).