Glucovance
General Information about Glucovance
Glyburide, the opposite active ingredient in Glucovance, belongs to a class of medication generally known as sulfonylureas. It works by stimulating the pancreas to produce more insulin, which in turn helps to decrease blood sugar levels. It also helps by reducing the amount of glucose launched by the liver, and increasing the physique's sensitivity to insulin.
In conclusion, Glucovance is a combination of two oral medicines that work together to effectively manage kind 2 diabetes. By lowering the amount of glucose produced by the liver, rising the body's sensitivity to insulin, and stimulating the production of insulin, Glucovance helps to lower blood sugar levels and enhance the physique's response to insulin. If you might have been diagnosed with type 2 diabetes, discuss to your doctor about whether or not Glucovance could also be an acceptable treatment option for you. Remember to at all times observe your doctor's directions and keep a healthy way of life to successfully handle your situation.
Combining these two medicines creates a synergistic effect, making Glucovance a strong tool in controlling type 2 diabetes. It not only helps to lower blood sugar ranges, but in addition addresses the underlying causes of the condition. This makes it a preferred alternative among healthcare professionals for the treatment of kind 2 diabetes.
Type 2 diabetes is a continual situation that affects tens of millions of people worldwide. It is characterized by high blood sugar ranges, attributable to the body's lack of ability to properly use insulin or produce enough of it. Insulin is a hormone that helps regulate glucose levels within the blood and is important for providing energy to the physique's cells. Without proper management, high blood sugar ranges can result in critical and doubtlessly life-threatening complications similar to coronary heart disease, kidney failure, and blindness.
Glucovance is a medicine generally prescribed for the therapy of sort 2 diabetes. It is made up of two oral medicine: metformin and glyburide, each of which have a hypoglycemic effect. By combining these two medicine into one medication, Glucovance is able to effectively lower blood sugar levels and assist manage the signs of kind 2 diabetes.
In addition to taking Glucovance, it is essential to observe a wholesome way of life, which features a balanced food plan and common train, to successfully handle kind 2 diabetes. Glucovance is not a cure for diabetes, however when used in mixture with a healthy life-style, it could help to manage blood sugar levels and cut back the chance of issues.
Metformin, one of the energetic ingredients in Glucovance, works by decreasing the amount of glucose produced by the liver and rising the body's sensitivity to insulin. This helps to lower blood sugar levels and enhance the physique's overall response to insulin. It also has the added benefit of reducing the quantity of glucose absorbed by the intestines, additional aiding in the control of blood sugar levels.
Glucovance is usually taken in tablet type, both once or twice every day, depending on the person's needs and response to the medication. The dosage may also have to be adjusted primarily based on factors corresponding to food plan, train, and different medications being taken. It is important to observe your doctor's directions fastidiously and to regularly monitor your blood sugar ranges while taking Glucovance.
Like any treatment, Glucovance could trigger side effects in some people. The most typical ones embrace nausea, diarrhea, stomach upset, and low blood sugar ranges. It is necessary to discuss any concerns or unwanted aspect effects with your doctor, as some could require a change in dosage or a unique medication.
The hockey-stick catheter and hydrophilic guidewire are manipulated into the area where the nipple of contrast material was seen and the stricture probed with the hydrophilic guidewire until the stricture is crossed symptoms meaning 400/2.5mg glucovance order fast delivery. The hockey-stick catheter is advanced through the stricture over the hydrophilic guidewire and both are manipulated into the proximal jejunum. The percutaneous track through the liver is dilated with a 7-French dilator and a 9-French peel-away sheath placed through the percutaneous track. If the obstructing lesion is not appropriate for stenting, an internal/external biliary drainage catheter is placed to drain the biliary system. The peel-away sheath protects the liver parenchyma, prevents buckling of the guidewire and catheter in the perihepatic space, and helps direct the pushing force applied to the catheter down the bile duct. Contrast material is injected and the catheter withdrawn until contrast material is seen to opacify the biliary tree proximal to the obstruction. A left-sided biliary drainage can be technically more challenging than using the right side, depending on the size of the left lobe, the anatomic configuration of the xiphisternum and costal margins, and the relationship of the left lobe to the costal margins and xiphisternum. There is a limited window of access to the left lobe through the inverted "V" formed by the xiphisternum and medial edges of the right and left costal margins. D, After dilating the percutaneous track to 8French, an 8-French peel-away sheath was placed, and through this a 10- Ч 90-mm Wallstent was placed across the stricture in the bile duct. We use ultrasound to locate the left lobe of the liver, assess the angle of approach into the bile duct, and indeed guide the needle into a bile duct. Depending on the size of the left lobe, a segment-2 duct, which has a more horizontal course in the left lobe, can be entered if the left lobe is large enough to permit access to segment 2. The advantage of using the segment-2 duct is that there is a more gentle curve with a less acute angle for manipulating guidewires and catheters down into the common bile duct. For patients with hilar obstruction, it is important to gain access to the left lobe biliary system in as peripheral a location as the anatomy allows. The 9-French peel-away sheath is important particularly when access is gained through a segment-3 duct because it helps direct the pushing force applied to the catheter down the common bile duct and makes placement of the catheter significantly easier. Hilar Obstruction Patients with hilar obstruction form a subset of patients with biliary obstruction who are technically challenging to treat and who are usually best palliated by percutaneous methods if the obstruction is not surgically resectable. A, In patients with a large left lobe it may be possible to enter the segment-2 bile duct, which generally has a horizontal course in the left lobe and allows easy access into the common hepatic duct. B, In patients with smaller left lobes, the segment-3 duct is usually accessible, but there is a more acute angle for entry down the bile duct. A peel-away sheath is important in this situation to ensure that the pushing force applied to catheters is directed toward the common bile duct. C, In patients with very small left lobes, a left-sided biliary drainage is difficult with a very acute angle of entry into the segment-3 duct, making guidewire purchase and other manipulations difficult. Patient with hilar cholangiocarcinoma who had a left-sided biliary drainage, because of a separate occlusion of right sided ducts and the left lobe was judged to be large enough to provide palliation of jaundice. Although some operators drain one side only, we have found over the years that optimal palliation is achieved when both sides are stented. Even though our reasons for doing this are anecdotal, given the progressive nature of the disease, it seems appropriate to drain both sides. Draining both sides also means that there are no undrained segments that may become infected at a later date and require a further drainage procedure. There are a number of metal stents used in the biliary tree, with the most popular being the Wallstent (Boston Scientific, Natick, Mass. The Wallstent has a small delivery catheter (7-French), the delivery system is flexible, and the stent has a large luminal diameter (1 cm). Biliary Drainage: Key Points One-stick needle system used for access Stricture negotiated with short catheter and hydrophilic wire 9-French peel-away sheath placed 8. In this situation, it is often best to drain the left side by itself as long as the left lobe is of adequate size and there is no second-order bile duct involvement on the left side. In one approach, a single right- or left-sided biliary drainage is performed and two Wallstents are placed across the biliary hilum in a T-configuration. A guidewire is placed through the metal mesh of this initial stent, down into the duodenum, and an 8-mm balloon is used to make a hole in the mesh of this stent. The principles of effective palliation for hilar strictures are: · Peripheral purchase within the biliary tree · Overstenting Overstenting means that the proximal end of the stent is situated at least 2-3 cm above the proximal edge of the tumor. This can be done by injecting contrast material into the duodenal loop using the hockey-stick catheter when the tumor has been crossed. Obviously, if there is duodenal encasement, the stent will not provide effective palliation and the patient may need a gastro-jejunostomy or other form of surgical decompression. Approximately 3-4 cm of the stent is placed above the proximal edge of the tumor and the distal end of the stent is left in the duodenum. Again, a safety catheter is not left in place if the procedure has been uneventful, but the stent is balloon dilated if a safety catheter is not left in situ (Box 20-5). A, In patients with a horizontally orientated hilar confluence, it may be possible to perform T-stenting from a single biliary drainage. However, the vast majority of patients do not have a horizontally orientated hepatic hilum, so T-stenting is not suitable for the majority of patients. Hilar Strictures and Metal Stents Double-Y stenting best where possible 10- Ч 90-mm Wallstent used Peripheral biliary purchase necessary Proximal stent position 2-3 cm above tumor Y-stents placed simultaneously and deployed sequentially Correct catheter fixation to the skin is important for biliary drainage catheters because they are subject to the effects of liver movement during breathing, movement which can be significant. Or, a side hole may migrate outside the liver and communicate with either the pleural space or abdominal cavity, leading to a bile leak. Intravenous fluids are important to correct choleresis, which is often marked in these patients and which may precipitate hepatorenal failure. If problems are encountered with the catheter, the patient should be brought to the interventional suite for a cholangiogram and appropriate action taken. If the procedure has gone smoothly without evidence of hemobilia, and if the patient is not septic, we generally do not leave a safety catheter.
Gastrostomy: Key Points Keep stomach optimally distended by air at all times T-fastener gastropexy Angle gastrostomy track toward pylorus treatment variable order glucovance overnight delivery, if possible 14- to 16-French tube, button or percutaneous endoscopic gastrostomy placed Gastrojejunostomy performed if history of hiatus hernia, reflux, or aspiration literature indicates that routine use is probably not necessary. There are many large series in the literature that describe percutaneous gastrostomy without gastropexy without any increase in complications. The theoretical advantages of using gastropexy are that larger catheters can be placed de novo, catheters and guidewires do not buckle into the peritoneal cavity, peritoneal leakage of gastric contents is less likely, and the catheter can be replaced if it is inadvertently pulled out soon after the procedure. In four of the 42 patients (9%) from the nongastropexy group, serious technical difficulties were encountered with misplacement of the gastrostomy tube in the peritoneal cavity in two patients. This would suggest that the placement of large-bore gastrostomy tubes (greater than 14-French) may cause problems without performing gastropexy. There are some situations in which use of a gastropexy device is important, including patients with ascites in whom gastropexy combined with regular paracentesis is necessary to prevent tube dislodgment from the stomach. The needle is inserted toward the pylorus at a 45-degree angle; if conversion of the tube to a gastrojejunostomy is required at a later date, the track will be angled toward the pylorus. If nasogastric tube placement is not possible or if carbonated granules cannot be given, a 22-gauge Chiba needle is placed into the stomach and contrast injected to confirm an intraluminal position. Even though the gastrostomy track is angled toward the pylorus, the tip of the tube usually ends in the most dependent portion of the stomach - the fundus. Some authors have described the placement of a large balloon into the stomach remnant, wherein the balloon is inflated and direct puncture of the balloon is used to obtain initial percutaneous access. Sometimes the body of the stomach can be entered directly with a needle; on other occasions the efferent small bowel loop is punctured and the catheter tip ultimately positioned in the gastric remnant. In general, gastric remnants that have previously been operated on are relatively fixed in the abdomen owing to postoperative fibrosis and adhesions. Once access to the stomach is gained with a one-stick needle system, the track is dilated and a 12- to 14-French nephrostomy type catheter is placed in the gastric remnant. In one metaanalysis of the literature by Wollman and associates, the average success rate of percutaneous gastrostomy tube placement was 99. By and large, percutaneous gastrostomy has become a widely accepted technique for gastrostomy tube placement and compares favorably with the endoscopic technique. The retention device of the gastrostomy catheter had pulled out of the stomach because of the weight of the ascites pressing on the stomach wall. It is important when performing percutaneous gastrostomy in a patient with ascites to drain the ascites on a regular basis to prevent this from happening. This patient was brought to the operating theater where it was noted that the four T-tacks had pulled through the stomach wall and were lying under the anterior abdominal wall. The major complication rate included four patients with peritonitis, two with hemorrhage requiring blood transfusion, and one with external leakage of gastric contents. Prior opacification of the colon and avoiding the location of the superficial epigastric artery can help avoid colonic perforation and hemorrhage, respectively. Performing a gastropexy may help decrease the incidence of guidewire buckling and dislodgement of the gastrostomy tube into the peritoneal cavity. If the patient comes to the interventional suite soon after catheter dislodgment, it is usually possible to regain access to the stomach using a combination of a Kumpe catheter and hydrophilic wire. The referring clinician should be advised to replace the tube if it does fall out at night or over a weekend so that the percutaneous track is kept open until a new tube can be placed the following morning. Avoiding Complications Prior colonic opacification Regular paracentesis if ascites present Optimal gastric distention during procedure T-fastener gastropexy allows a more controlled procedure Avoid superficial epigastric artery with frequent dressing changes and wound cleansing. The combination of wound toilet, application of an antacid solution around the stoma, and upsizing the tube all help to control the skin irritation and breakdown. Occasionally, none of these procedures work and the tube may have to be removed, particularly if the skin breakdown is severe (Box 19-4). Unfortunately, existing gastrostomy catheters are derived from either "abscess drainage" catheters or "Foley"-type balloon catheters. Consequently, some authors have embarked upon the placement of the more robust endoscopic gastrostomy tubes using a percutaneous approach. If the esophagus cannot be cannulated from below, a snare can be used to pull the guidewire out of the stomach, into the esophagus, and out through the mouth. The pull type endoscopic gastrostomy catheter is then pulled from the mouth down through the esophagus and out through the anterior abdominal wall. Disadvantages include seeding of metastases from oropharyngeal or esophageal tumors, potential risk of infection, and the need for two operators to perform the procedure. A major disadvantage of the "button"-type catheter is the fact that a mature track of at least 3 months is advised before insertion of a gastrostomy button. We have not been able to place the mushroom-type button without having a mature track; we have placed the balloon retention gastrostomy button in more than 100 patients. When the stomach has been punctured and a superstiff guidewire placed, the track length can be measured by using an angioplasty balloon catheter, which is inflated within the stomach and pulled back until it abuts the anterior abdominal wall. To place a 14-French button, the track is dilated to 18 French; to place a 16-French button, the track is dilated to 20 French; to place an 18-French button, the track is dilated to 22 French. When the track is dilated, a small fascial dilator is placed through the button and loaded on the guidewire (6-French dilator for a 14-French button; 7-French dilator for a 16-French button; 8-French dilator for an 18-French button). The advantages of button catheters are many, with the most significant being the avoidance of catheter clogging due to the short tube length. Percutaneous gastrojejunostomy can be more technically challenging and tedious because the gastrostomy catheter has to be negotiated past the pylorus and duodenum into the jejunum.
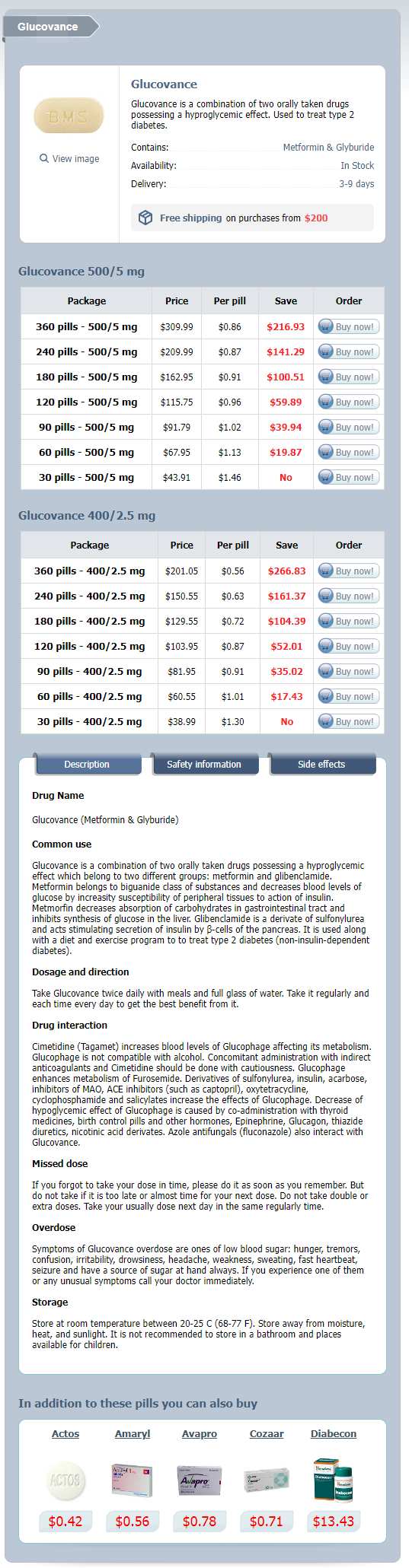
Glucovance Dosage and Price
Glucovance 500/5 mg
- 360 pills - $309.99
- 240 pills - $209.99
- 180 pills - $162.95
- 120 pills - $115.75
- 90 pills - $91.79
- 60 pills - $67.95
- 30 pills - $43.91
Glucovance 400/2.5 mg
- 360 pills - $201.05
- 240 pills - $150.55
- 180 pills - $129.55
- 120 pills - $103.95
- 90 pills - $81.95
- 60 pills - $60.55
- 30 pills - $38.99
When the ventricles relax at the beginning of diastole symptoms by dpo cheap glucovance 500/5 mg fast delivery, the ventricular pressures decrease significantly below those in the aorta and pulmonary trunk and the aortic and pulmonary valves close. Filling occurs very rapidly at first so that atrial contraction, which occurs at the very end of diastole, usually adds only a small amount of additional blood to the ventricles. The amount of blood in the ventricles just before systole is the end-diastolic volume. The volume remaining after ejection is the end-systolic volume, and the volume ejected is the stroke volume. Pressure changes in the systemic and pulmonary circulations have similar patterns, but the pulmonary pressures are much lower. List the structures through which blood passes from the systemic veins to the systemic arteries. Contrast and compare the structure of cardiac muscle with that of skeletal and smooth muscle. Describe the autonomic innervation of the heart, including the types of receptors involved. Describe the changes in membrane permeability that underlie the membrane potential changes. Explain how the electrical activity of the heart can be viewed from different angles with electrocardiography. Draw a diagram of the pressure changes in the left atrium, left ventricle, and aorta throughout the cardiac cycle. Show when the valves open and close, when the heart sounds occur, and the pattern of ventricular ejection. Contrast the pressures in the right ventricle and pulmonary trunk with those in the left ventricle and aorta. Write the formula relating cardiac output, heart rate, and stroke volume; give normal values for a resting adult. Describe the effects of sympathetic and parasympathetic neuronal stimulation on heart rate. Describe the effects of sympathetic neuron stimulation on cardiac muscle during contraction and relaxation. Draw a pair of curves relating end-diastolic volume and stroke volume, with and without sympathetic stimulation. Although the action of the muscular heart provides the overall driving force for blood movement, the vascular system plays an active role in regulating blood pressure and distributing blood flow to the various tissues. Elaborate branching and regional specializations of blood vessels enable efficient matching of blood flow to metabolic demand in individual tissues. This section will highlight repeatedly the general principle of physiology that structure is a determinant of function, as we examine the specialization of the different types of vessels that comprise the vascular system. However, the entire circulatory system, from the heart to the smallest capillary, has one structural component in common: a smooth, single-celled layer of endothelial cells (endothelium) that is in contact with the flowing blood. Capillaries consist only of endothelium and associated extracellular basement membrane, whereas all other vessels have one or more layers of connective tissue and smooth muscle. Endothelial cells have a large number of functions, which are summarized for reference in Table 12. We have previously described the pressures in the aorta and pulmonary arteries during the cardiac cycle. Text sections dealing with the individual vascular segments will describe the reasons for these changes in pressure. Although they also have smooth muscle, arteries can be viewed most conveniently as elastic tubes. The large radii of arteries suit their primary function of serving as low-resistance tubes conducting blood to the various organs. Their second major function, related to their elasticity, is to act as a "pressure reservoir" for maintaining blood flow through the tissues during diastole, as described next. Arterial Blood Pressure What are the factors determining the pressure within an elastic container, such as a balloon filled with water? The pressure inside the balloon depends on (1) the volume of water and (2) how easily the balloon can stretch. If the balloon is thin and stretchable, large quantities of water can be added with only a small increase in pressure. Conversely, the addition of even a small quantity of water causes a large pressure increase Cardiovascular Physiology 387 Large vein Few layers of smooth muscle and connective tissue Few elastic layers Large artery Many layers of smooth muscle and connective tissue Several elastic layers Artery Vein Inferior vena cava Aorta Wide lumen Endothelium Venule Endothelium Arteriole Lumen Lumen 4. Inset: Light micrograph (enlarged four times) of a medium-sized artery near a vein. The term used to denote how easily a structure stretches is compliance: Compliance = Volume/Pressure the greater the compliance of a structure, the more easily it can be stretched. If a precisely equal quantity of blood were to simultaneously drain out of the arteries into the arterioles during systole, the total volume of blood in the arteries would remain constant and arterial pressure would not change. The rest of the stroke volume remains in the arteries during systole, distending them and increasing the arterial pressure. When ventricular contraction ends, the stretched arterial walls recoil passively like a deflating balloon, and blood continues to be driven into the arterioles during diastole. The next ventricular contraction occurs while the artery walls are still stretched by the remaining blood. Arterial pressure is generally recorded as systolic/diastolic, which would be 120/80 mmHg in the example shown. Both systolic pressure and diastolic pressure average about 10 mmHg lower in females than in males.