Ibuprofen
General Information about Ibuprofen
Moreover, people with asthma could experience opposed reactions to ibuprofen, corresponding to worsening of asthma symptoms and issue respiratory. It is beneficial to seek the guidance of a doctor earlier than using ibuprofen in case you have bronchial asthma or some other respiratory situation.
Ibuprofen works by inhibiting the manufacturing of prostaglandins, which are chemical substances liable for inducing pain, irritation, and fevers within the physique. By decreasing the manufacturing of prostaglandins, ibuprofen helps alleviate ache and irritation, making it a extremely sought-after treatment.
Another threat associated with ibuprofen is its potential interplay with sure drugs. For instance, it might scale back the effectiveness of blood strain drugs and enhance the chance of kidney damage when taken with diuretics. It is essential to inform your physician about another medicines you take to avoid such interactions.
In conclusion, ibuprofen, marketed underneath the brand name Motrin, is a extremely effective over-the-counter medication for relieving pain and irritation. It has been extensively used for decades and continues to be a go-to for individuals suffering from circumstances corresponding to arthritis and rheumatism. Its advantages embody ache aid, anti-inflammatory results, and potential protection against heart illness and cognitive decline. However, it also carries some potential risks, and it is essential to follow the beneficial dosage and precautions when using this medication. If you expertise any adverse results, it is best to consult a doctor for steering. Overall, ibuprofen stands as a valuable device in providing aid from various ailments and enhancing the quality of life for so much of individuals.
Like another medicine, ibuprofen also carries some potential risks. Long-term use or excessive doses of ibuprofen may trigger stomach irritation, leading to gastrointestinal problems such as ulcers and bleeding. It is important to stay to the recommended dosage and length of use to reduce these dangers. Individuals with a history of stomach ulcers or bleeding issues ought to seek the guidance of their doctor earlier than taking ibuprofen.
First introduced within the 1960s, ibuprofen rapidly gained recognition as a outcome of its capacity to effectively scale back ache, fever, and inflammation. Since then, it has turn into a household name and is out there over-the-counter in most international locations, making it easily accessible for anybody in need of pain reduction. Its widespread use may be attributed to its effectiveness and relatively low side effects compared to other NSAIDs.
Ibuprofen, popularly recognized by its brand name Motrin, is certainly one of the most widely used nonsteroidal anti-inflammatory drugs (NSAIDs) on the planet. It is well-known for its efficient pain-relieving and anti-inflammatory properties, and is often used to treat varied situations such as rheumatism and arthritis. In this article, we will delve deeper into the uses, benefits, and potential dangers associated with this medicine.
One of the first uses of ibuprofen is in the treatment of rheumatism and arthritis. These situations are caused by irritation in the joints, resulting in ache and stiffness. Ibuprofen is effective in lowering this inflammation, thus offering relief from related signs. It is also used to deal with different circumstances corresponding to menstrual cramps, dental pain, and headaches.
Aside from its pain-relieving properties, ibuprofen additionally has a quantity of different advantages. It has been found to decrease the risk of coronary heart disease and stroke when taken in low doses for an extended interval. This is as a result of it acts as a blood thinner, preventing blood clots from forming. Additionally, analysis has additionally suggested that ibuprofen could have a optimistic impression on age-related and cognitive decline and should help in preventing Alzheimer's illness.
Instead of inserting a biliary drainage catheter pain studies and treatment journal generic ibuprofen 400 mg amex, the stricture is predilated to 10 mm using a balloon catheter to facilitate rapid expansion of the metallic stent. After predilation, the stent on its introducer system is advanced across the lesion and is deployed so that the lower end projects through the ampulla and the upper end is well above the stricture. After stent deployment, a temporary small catheter is inserted foraccess in case of complications and is removed the next day after cholangiography. Postprocedure management instructions following biliary drainage are summarized in Table 15. Ifthecatheter permits drainage of bile into the bowel, then the drainage catheter can be capped to allow internal drainage. If the patient is able to tolerate internal drainage for 8 to 12 hours, then he/she can be discharged. If internal drainage is not possible, then external bag drainage must be maintained. With external drainage, dehydration can occur, unless adequate steps are taken to replace the lost fluids. Thishelpspreventdebrisfrom accumulating in the catheter and causing it to occlude. They should be instructed to call if they experience pain, chills, fever, or nausea or vomiting. Any malposition of the tube, bleeding within it, or leakage around the tube should also be taken seriously. A thorough cholangiogram with special attention to the ductal anatomy can sometimes identify a missing ductal segment, indicating an isolated undrained system. If the patient has a capped biliary catheter, the tube should be uncapped to allow the bile to drain externally. If externalizing the drainage catheter resolves the infection, then fluoroscopic evaluation of the catheter can be performed electively. If fever persists after externalization, however, then an emergency catheter evaluation should be performed. If catheter obstruction is not the source of sepsis, then the patient should be evaluated for undrained ductal segments. Care should be taken to avoid the pleural reflection so as not to breach the pleural space. With left-sided drains, patients have less catheter-related discomfort (the right intercostal approach being more painful) and they can more easily manage the catheter when it exits out from the midline, rather than the midaxillary line. The left-sided approach is also preferable when there is ascites because the risk of peritoneal leak is reduced. For left-sided approach, the operator needs to ensure that the catheter enters the medial, rather than the lateral, ducts. The lateral ducts are more posterior and, therefore, the catheter pathway will be directed posteriorly and then anteriorly, thus affecting the pushability, while negotiating the more distal obstruction. Hilar strictures may be treated by a single stent or by bilateral stents, depending on the pattern of biliary obstruction. If there is free communication between the left and right systems, unilateral stenting is sufficient. If only unilateral biliary drainage has been performed, but it is necessary to drain both lobes, bilateral drainage can still be accomplished if metallic stents are used. Although this T configuration achieves drainage of both liver lobes, the Y configuration is preferable because it allows easier intervention if the stents become occluded. Biliary side branches covered by the uncovered stents during placement are not associated with branch occlusion. The right hepatic duct is short, unlike the left, which is 2 to 3 cm long, until its bifurcation into the segmental ducts. Thus a catheter placed in the right system initially drains a greater part of the liver because of the size difference between the lobes. Once the tumor grows, the situation reverses because the catheter placed in the right side now drains only one segment, whereas the left-sided catheter drains the entire left lobe. Thus, for type 2 lesions either the right anterior system or the left system is chosen (left is chosen if the left lobe of the liver is of good size). It has been shown that drainage of 25% of the liver volume using a single catheter/endoprosthesis may be sufficient. Lobes and segments that are atrophic or have extensive tumor burden are not drained unless they are infected. Additionally, it is easier to cannulate them endoscopically for clearance or for additional endoprosthesis insertion. If the stent projects too far into the duodenum, it can cause erosion of the opposite wall. Plastic stents are placed by many endoscopists because of their acceptable patency rates, retrievability, low cost, and the ability of the endoscopist to insert plastic stents in a single-stage procedure. Metallic stents are more expensive than plastic endoprostheses and there has been considerable debate since metallic stents were introduced as to whether the results of metallic stents compared with plastic devices justify their additional costs. The main cause of occlusion of metallic stents is tumor ingrowth or overgrowth; bile encrustation seldom occurs. The best method of treatment of blocked biliary stents is endoscopic replacement, in the case of plastic endoprostheses, or endoscopic insertion of a plastic stent inside a metallic endoprosthesis. Percutaneous evaluation and therapy of occluded stents is usually reserved for patients in whom endoscopy has been unsuccessful or is not possible.
The Carotid Revascularization Endarterectomy versus Stenting Trial: credentialing of interventionalists and final results of lead-in phase otc pain treatment for dogs proven 600 mg ibuprofen. Characteristics of ischemic brain lesions after stenting or endarterectomy for symptomatic carotid artery stenosis: results from the international carotid stenting study-magnetic resonance imaging substudy. Less common causes include vasculitides, trauma, aortic dissections, volvulus, intussusceptions, hernias, adhesions, drugs (cocaine), cholesterol emboli, and intestinal obstruction. The classic clinical presentation of acute mesenteric ischemia is an abrupt onset of severe abdominal pain that is out of proportion to the physical examination. Diagnosis of this condition may be aided by a high index of clinical suspicion, history of cardiovascular disease, presence of hypotension requiring vasopressor support, and diagnostic imaging evaluation. In the diagnostic imaging assessment of mesenteric ischemia, catheter-based angiography remains the gold standard given its superior resolution, accuracy in detection of both large- and small-vessel disease, and ability to dynamically follow a delivered contrast bolus from arterial through venous phases. With advancements in noninvasive imaging techniques, catheterbased angiography is now generally employed in anticipation of endovascular therapy, to clarify findings of an equivocal noninvasive imaging study, or to further define vascular anatomy prior to surgery. Its sensitivity is limited for detection of very small emboli or a subtle vasculitis, however, and its use may be contraindicated in patients with severe renal insufficiency. Additionally, newer sequences can track a contrast bolus from the arterial through venous phases, allowing for the detection of both arterial lesions and mesenteric vein thrombosis. Its utility in small-vessel disease and in the assessment of bowel integrity is limited, however. Endovascular management, however, has played an increasing role with multiple case series and reports describing success with initial endovascular therapy or in combination with open surgical intervention. A frequent association with atrial fibrillation or prior myocardial infarction is seen and approximately 20% of individuals will have a concurrent peripheral arterial embolus. About 33% of individuals presenting with acute mesenteric ischemia from an embolic source will have had a history of a prior embolic event. The clinical presentation of embolic acute mesenteric ischemia typically involves an abrupt onset of severe abdominal pain, diarrhea, and/or hematochezia. Formation of thrombus directly within the mesenteric arterial vasculature occurs in about 25% of cases of acute mesenteric ischemia. It is typically seen in patients with underlying atherosclerotic lesions and is associated with previous reports of intestinal angina in up to 50% of cases. In contrast to acute embolic mesenteric ischemia, acute thrombotic mesenteric ischemia generally has a less abrupt, more insidious onset. Collateral vessels may be present, consistent with a more chronic condition in which an acute on chronic process has developed. Nonselective abdominal aortogram reveals dissection extending through the abdominal aorta. Dissection flap involves the left renal artery (arrowheads), resulting in marked reduction in flow to the left kidney. Historically, treatment of arterial occlusive acute mesenteric ischemia has involved primary surgical exploration, revascularization, and resection of infarcted bowel. Satisfactory results were observed in seven patients with two of these requiring adjunctive local thrombolysis. In this group, endovascular therapy was performed with all patients undergoing stent or stent-graft placement. Additionally, one patient received open surgical thrombectomy, one received suction thrombectomy, and one underwent local thrombolysis. Thirteen patients underwent exploratory laparotomies and eight underwent bowel resection. An in-hospital survival rate of 74% was observed with successful thrombolysis being associated with a decrease in mortality. The management of acute arterial occlusive mesenteric ischemia is evolving to include more aggressive application of endovascular therapy as an initial approach, even in the presence of bowel infarction. With imaging-verified mesenteric arterial occlusion or with a high level of clinical suspicion, the management of each patient depends heavily on the presence of bowel infarction versus bowel ischemia. If bowel infarction is present, revascularization with embolectomy/ bypass or endovascular revascularization approaches should be performed as soon as possible, followed by an exploratory laparotomy to remove infarcted bowel. The intra-arterial papaverine is administered during the surgical procedure and in the postoperative period to optimize intestinal perfusion. Occlusion was crossed with a hydrophilic guide wire and catheter, after which a sheath was placed. Persistent focal occlusion (arrow) is still seen at the proximal aspect of this vessel, likely secondary to atherosclerotic disease. However, continuous perfusion of bowel is supplied through abundant mesenteric collaterals. Lysis of an acute embolus/thrombus can be performed with the use of mechanical thrombectomy and embolic protection devices. Intra-arterial papaverine can also be added to the treatment regimen to maximize intestinal perfusion. Anticoagulation should be initiated and continued in all patients who present with an arterial embolus. In the setting of an aortic dissection causing acute mesenteric ischemia, operative repair is associated with a mortality rate that approaches 90%. Early intervention with endograft and endovascular therapy may reduce mortality rates.
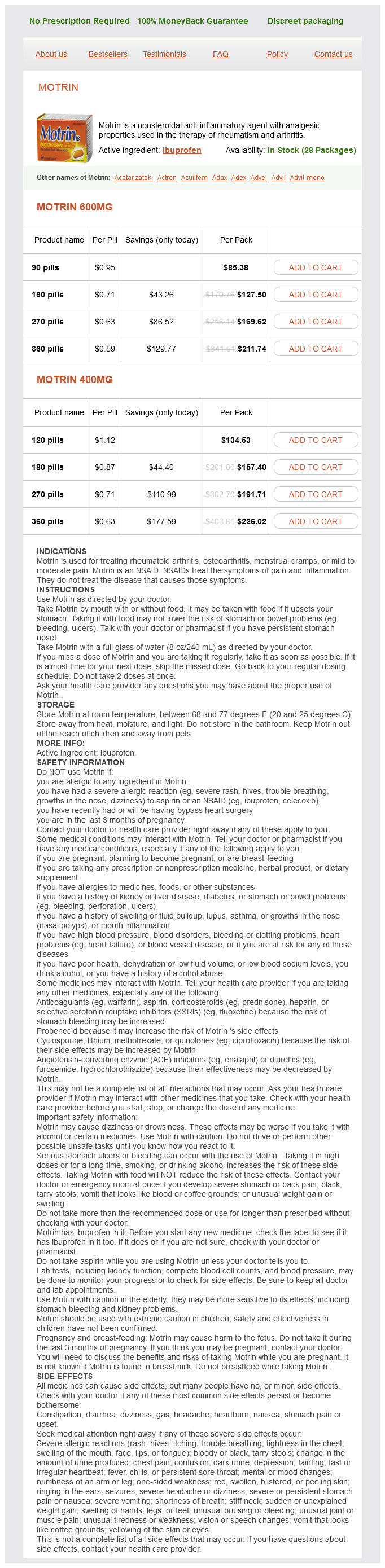
Ibuprofen Dosage and Price
Motrin 600mg
- 90 pills - $85.38
- 180 pills - $127.50
- 270 pills - $169.62
- 360 pills - $211.74
Motrin 400mg
- 120 pills - $134.53
- 180 pills - $157.40
- 270 pills - $191.71
- 360 pills - $226.02
A neurologic deficit has been found to be associated with a high percentage of vascular injuries in some studies pain treatment center american fork cheap 400 mg ibuprofen mastercard, but this finding has not been confirmed by others. The greatest controversy exists as to the need for arteriography for wounds near major neurovascular bundles. Other approaches have been reported for stable patients with suspicion of vascular injury. Duplex ultrasound has been recommended as a screening tool to identify traumatic arterial injury. The sensitivity of ultrasound for detection of arterial injury has been reported from a poor 50% to an excellent 99%. It is an operator-dependent examination that is tedious when more than a single anatomic region needs evaluation. These include the ability to generate isotropic data sets of long vascular territories with the acquisition performed in a short time. A single, plain film is obtained following contrast injection, by hand, via a small needle. Such an exam is limited to only one vascular territory, and injection timing errors could miss injuries. The mechanism of injury is also an important factor in the decision to perform arteriography. All high-velocity wounds, such as those from assault weapons and rifles, should undergo exploration or arteriography because of the greater force and possibility of remote concussive damage. High-speed missiles are preceded by a shock wave and followed by an area of decreased pressure called the temporary cavity, which can produce extensive damage. Such high-velocity wounds have the highest incidence of arterial injury, followed in decreasing order by gunshot wounds and stab wounds, which must penetrate the vessel directly. As with other forms of trauma, it remains controversial whether arteriography is indicated in all patients with knee dislocation or only in those with physical or Doppler signs of injury. Among patients with fractures requiring admission, the arterial injury rate is only 0. Complex fractures of the tibia and fibula are frequently associated with vascular injury. Identification of these injuries is important because isolated tibial arterial injuries, when associated with extensive soft-tissue damage, should be repaired to avoid limb loss, nonunion of fractures, and poor wound healing. Even small injuries were explored because of fear of subsequent thrombosis and possible distal embolization. Accordingly, doubt exists regarding the necessity to explore or treat small arterial injuries. Many of these asymptomatic injuries may not require surgical or radiologic intervention but rather can heal spontaneously. When observation is the chosen management, clinical follow-up is essential because of the unpredictability of injury healing. Areas of segmental narrowing and small intimal flaps are best suited to such follow-up. Observation needs to be maintained until the injury completely heals or until definitive therapy is provided. Therefore, improving but incompletely healed or stable injuries require serial follow-up examinations. Alternatively, some trauma specialists believe that because major vascular injuries can result in limb loss and functional disability in characteristically young victims, diagnosis and repair of all injuries is critical. The cost and legal ramifications of a missed diagnosis motivate some surgeons to request arteriography on all penetrating trauma patients. Missed injuries requiring delayed intervention may not be as difficult to repair, nor complications as frequent, as previously thought. Frontal arteriogram after through-and-through gunshot wound to the knee reveals smooth tapering of the popliteal artery initially thought to be caused by spasm. The lateral view reveals a popliteal artery pseudoaneurysm and demonstrates the importance of orthogonal views. Injury of the proximal superficial femoral artery was treated with surgical vein graft (arrowheads). A large pseudoaneurysm arising from the deep portion of the profunda femoris artery was missed (arrow). When large foreign bodies are present, fluoroscopy and test injections can allow positioning of the vessel of interest away from obscuring metallic material. Vessels proximal and distal to the potential injury site should be evaluated as well. Careful positioning of the catheter is important so that all arteries in the potential injury path are evaluated. Knowledge of both the entrance and exit wounds, if present, is therefore required. The catheter should be positioned proximal enough to the injury site to allow for common anatomic variants. Occlusions may be caused by extrinsic vessel compression or by thrombosis associated with arterial laceration or intimal flap. Luminal narrowing may be secondary to arterial spasm, intramural hematoma, extrinsic compression, or atherosclerosis. The vessel course may be altered because of hematoma or associated long bone fracture displacement. Slow flow is an important finding and may be the sole arteriographic indication of a compartment syndrome. Luminal narrowing may be a result of arterial spasm, which appears as a focal area of smooth concentric narrowing and is particularly prevalent in pediatric patients.