Isoptin
General Information about Isoptin
Isoptin, also known as verapamil, is a drugs used for controlling hypertension. It belongs to the class of calcium channel blockers and works by enjoyable the blood vessels, allowing for easy blood flow and reducing the pressure within the arteries.
In conclusion, Isoptin is an efficient medicine for controlling hypertension. It works by enjoyable the blood vessels, resulting in a decrease blood stress. It is important to observe the prescribed dosage and seek the advice of your doctor if you expertise any side effects. With correct use and monitoring, Isoptin may help in managing hypertension and reduce the risk of complications related to high blood pressure.
Isoptin is usually protected and well-tolerated by most people. However, as with any medication, there are some potential side effects. The most common ones embrace dizziness, headache, and constipation. More severe unwanted facet effects, though rare, might embrace low blood pressure, gradual heart fee, and heart rhythm disturbances. It is essential to tell your doctor if you expertise any of those side effects while taking Isoptin.
High blood stress, or hypertension, is a standard situation affecting tens of millions of individuals worldwide. It happens when the drive of blood towards the artery partitions is merely too excessive, placing extra pressure on the heart and blood vessels. If left uncontrolled, high blood pressure can result in serious well being issues corresponding to heart disease, stroke, and kidney failure.
In addition to controlling hypertension, Isoptin can additionally be used for treating varied heart circumstances similar to angina, arrhythmias, and coronary heart failure. It can be used to forestall or reduce recurring chest pain and improve blood move to the center.
Isoptin helps in treating high blood pressure by blocking the entry of calcium into the sleek muscles of the blood vessels, inflicting them to loosen up and dilate. This leads to a lower blood pressure and decreased workload on the heart.
The medicine is on the market in each immediate-release and extended-release formulations, and is usually taken orally a couple of times a day. It is necessary to take it exactly as prescribed by the physician for optimum effectiveness.
Certain precautions should be taken when utilizing Isoptin. It just isn't recommended for individuals with a known allergy to verapamil or those who have a history of heart failure, liver or kidney illness, or low blood strain. It should also be used with caution in pregnant or breastfeeding ladies.
Moreover, Isoptin shouldn't be taken with sure medicines corresponding to beta-blockers, amiodarone, and certain antibiotics. It is important to inform your physician about all the medicines you are taking to avoid potential drug interactions.
Splenectomy prehypertension systolic discount 40 mg isoptin free shipping, or removal of the spleen, is used as therapy for some chronic disorders or an emergency procedure for traumatic rupture of the spleen. Splenectomy in adults usually has no clinical consequence, but in children it leads to increased occurrence and severity of infections. Splenic lymphoid nodules are numerous in young people but become relatively scarce with aging. The capsule consists of collagen and elastic fibers with scattered fibroblasts and a few smooth muscle cells. The fibrous capsule is usually covered by a serous mesothelial layer of the visceral peritoneum (not seen here), which is normally simple squamous epithelium. The red pulp constitutes 75% of the volume of the spleen and contains all formed elements of circulating blood. Suspended between trabeculae is a communicating network of reticular fibers, with many attached macrophages and reticular cells. It consists of white pulp and red pulp, so named because of their color in the fresh state. As in lymph nodes, B cells may be found in primary (unstimulated) lymphoid nodules or secondary (stimulated) nodules with germinal centers. Surrounding white pulp is a shell of sparsely cellular lymphoid tissue-the marginal zone-that contains many macrophages and some B lymphocytes. This zone is not as well defined in humans as in animals, and its demonstration requires special staining methods. Red pulp makes up most of the spleen, its color being due mostly to abundant erythrocytes. Found around white pulp, it consists of many thin-walled venous sinusoids and intervening cellular, or splenic, cords (of Billroth). The term splenic cords is misleading, in that these are labyrinthine spaces between sinuses containing a scaffold of reticular fibers. Many closely packed fixed or wandering cells-reticular cells, lymphocytes, plasma cells, macrophages, and all formed elements of circulating blood-occupy these spaces. Injection of India ink into an experimental animal, followed by removal of the spleen and then its microscopic examination, allows reaction product in macrophages to be seen. This section, so prepared, shows a high concentration of macrophages in the marginal zone of white Trabecular pulp after cells ingested black carbon particles of ink. Between the endothelium and smooth muscle is a prominent layer of elastic tissue, the internal elastic lamina (arrows). The splenic artery enters at the hilum and divides into several smaller trabecular arteries, so named because they travel in trabeculae. They are known collectively as central arterioles, which is a misnomer as these vessels are usually in an eccentric position in white pulp. They also have two layers of smooth muscle cells in their walls, which is a feature of arterioles. Some branches of the central arteriole end as marginal sinuses that supply the marginal zone of the white pulp. Other arterial branches enter the red pulp as short straight penicillar arterioles. These drain into sheathed capillaries, which have an external sheath of reticular fibers and many macrophages. In red pulp, they accommodate many lymphocytes, macrophages, and other cells in splenic cords. With silver stains, reticular fibers are black fibrous strands that form an interweaving network in the organ. Macrophages closely associated with sinusoid walls often require special techniques for detection. In the closed system, about 90% of capillaries supplying red pulp drain directly into venous sinusoids, such as normally occurs elsewhere in the body. An alternative is an open system: Remaining open-ended capillaries discharge blood freely into the intersinusoidal meshwork, so blood seeps out and percolates slowly between splenic cords before regaining access to sinusoids. Both open and closed patterns likely operate at different times, according to physiologic conditions. Venous sinusoids are a tortuous network of thin-walled vessels with irregular lumina. With diameters of 30-50 µm, they have a unique structure related to high permeability. Although adjacent endothelial cells lack junctions, they are separated by slit-like spaces, 1-5 µm wide. A thin, discontinuous basal lamina forms circular bands around the endothelial cells, like hoops around staves of a leaky barrel. Formed elements of blood can thus traverse the highly porous walls of venous sinusoids by squeezing through the slits. However, worn out or fragile erythrocytes, which have lost pliability, cannot reenter the circulation and are phagocytosed by macrophages. The spleen lacks afferent lymphatics, but efferent lymphatics beginning in white pulp exit at the hilum. Just under the capsule, the internal architecture of the organ appears disorganized with irregular patches of bluish/ purple stained lymphoid tissue (*) separated by densely eosinophilic areas of dense connectivetissue fibrosis. These cells are named for American pediatric pathologist, Dorothy Reed Mendenhall, and Austrian pathologist, Carl Sternberg. Key cellular features are: large size (30-50 µm), finely granular or amphophilic cytoplasm, and two mirror-image nuclei that resemble owl eyes, each with an eosinophilic nucleolus or nucleoli. Lymphocytes, eosinophils, and cells undergoing mitoses are also in the cell infiltrate. Characterized clinically by the contiguous spread of disease from one lymph node group to another, it is the most common mediastinal malignancy.
This provides a regulatory network that modulates the host defenses of the gastrointestinal tract and the immune reactivity of gutassociated lymphoid tissue hypertension kidney failure order 40 mg isoptin free shipping. The vagus nerve and sympathetic innervation from the pelvic splanchnic nerves cannot coordinate the activity of the colon in the absence of its enteric components. Therefore, megacolon (intestinal obstruction) results from absent peristalsis and loss of smooth muscle tone of the colon. Peripheral Nervous System T7 223 Sympathetic fibers Preganglionic Postganglionic Parasympathetic fibers Preganglionic Postganglionic Afferent fibers T8 Dorsal root ganglion T9 T10 Right greater thoracic splanchnic nerve Posterior vagal trunk Right phrenic nerve Left greater thoracic splanchnic nerve Anterior vagal trunk Common areas of referred pain in biliary diseases Diaphragm Phrenic ganglion Anterior vagal trunk Celiac ganglia Hepatic triad Portal vein branch Bile duct Hepatic artery branch Anterior hepatic plexus Posterior hepatic plexus Splenic artery Aorta Common hepatic artery Gastroduodenal artery and plexus Sphincter ampullae 9. Postganglionic noradrenergic sympathetic nerve fibers end directly adjacent to hepatocytes; norepinephrine released from these nerve fibers initiates glycogenolysis and hyperglycemia for fight-orflight responses and induces gluconeogenesis. Autonomic innervation helps to regulate vascular, secretory, and phagocytic processes in the liver. The gallbladder, especially the sphincter ampullae and the sphincter of the choledochal duct, is also supplied by autonomic nerve fibers. The sympathetic nerve fibers cause contraction of the sphincters and dilation of the gallbladder; the parasympathetic nerve fibers cause opening of the sphincters and contraction of the gallbladder. Autonomic neuropathy to the gallbladder can result in atonic smooth muscle responses, with the development of gallstones (especially in individuals with hypercholesterolemia) and diarrhea. Pancreatic exocrine glands and endocrine cells (islets of Langerhans) are innervated by parasympathetic subdiaphragmatic vagal nerve fibers via intramural ganglia and by sympathetic nerve fibers derived from T5T9 intermediolateral spinal cord gray via the celiac ganglion. Cholecystokinin is secreted by I cells in response to fats in the duodenum and upper jejunum and acts on acinar cells to stimulate the secretion of enzymes. Peripheral Nervous System 225 Intermediolateral cell column (lateral horn of gray matter) T10 Abdominopelvic splanchnic nerves (presynaptic fibers) Celiac, aorticorenal and renal ganglia T12 Postganglionic fibers supply blood vessels Medulla Cortex T11 L1 Spinal cord Sympathetic trunk Preganglionic cholinergic nerve fibers ramify around cells of the medulla Norepinephrine (20%) and epinephrine (80%) secreted into the general circulation Suprarenal gland (adrenal gland) 9. These chromaffin cells are of neural crest origin and function as sympathetic ganglion cells. An adrenal portal system conveys blood directly from the adrenal cortex to the adrenal medulla. Cortisol, derived from action of the hypothalamopituitary-adrenal axis, bathes the chromaffin cells in very high concentrations, inducing the enzyme phenylethanolamine-Nmethyl-transferase, which is responsible for the synthesis of epinephrine. Approximately 70% to 80% of the adrenal medullary output of catecholamines is epinephrine; the remaining output is norepinephrine. Both epinephrine and norepinephrine can be taken up into sympathetic postganglionic noradrenergic nerve terminals at any site throughout the body by the high-affinity uptake carrier and can be subsequently released. A sympathetic arousal response that generates the secretion of epinephrine from the adrenal medulla will therefore provide altered catecholamine content (higher epinephrine) because of high-affinity uptake in nerve terminals throughout the body; subsequent release of this epinephrine modifies the usual sympathetic balance of alpha versus beta receptor stimulation on target organs for a brief period. Peripheral Nervous System 2nd lumbar sympathetic trunk ganglion Intermesenteric (abdominal aortic) plexus Gray and white rami communicans L2 Inferior mesenteric ganglion Lumbar splanchnic nerves Right sympathetic trunk and its 3rd lumbar ganglion L3 Gray rami communicans Superior hypogastric plexus (presacral nerve) L4 Right and left hypogastric nerves Superior rectal artery and plexus Inferior mesenteric artery and plexus 227 1st sacral sympathetic trunk ganglion Nerves from inferior hypogastric plexuses to sigmoid and descending colon Gray rami communicans L5 Right ureter and ureteral plexus Seminal vesicle Sacral part of sympathetic trunk S1 Ductus deferens Sacral plexus S2 S3 S4 S5 Pelvic splanchnic nerves (sacral parasympathetic outflow) Pudendal nerve Vesical plexus Inferior rectal plexus Prostatic plexus Cavernous plexus Right inferior hypogastric (pelvic) plexus Dorsal nerve of penis 9. These fibers travel along visceral and vascular nerves to the colon, ureters, and great vessels, such as the inferior mesenteric and common iliac vessels. Parasympathetic nerve fibers arise from the S2S4 intermediate gray of the spinal cord and travel via the pelvic splanchnic nerves to distribute with the branches of the inferior hypogastric plexus. The parasympathetic ganglia are intramural, in or adjacent to the wall of the organ innervated. The sympathetic trunk ganglia and superior hypogastric plexus distribute sympathetic nerve fibers to pelvic viscera, and S2S4 intermediate gray neurons send pelvic splanchnic nerves via the inferior hypogastric plexuses to end in intramural ganglia that supply the pelvic viscera. Of particular functional importance is the autonomic distribution to the bladder and reproductive organs. Lesions in these pelvic autonomic nerves can occur with diabetes, demyelinating diseases, and mass lesions. Damage to pelvic parasympathetic nerves can produce a flaccid bladder with overflow incontinence and can cause erectile impotence in males. It should be noted that both parasympathetic and sympathetic autonomic nerves play roles in sexual function. Parasympathetic nerves are essential for proper erectile function, and sympathetic nerves play a role in ejaculation and may also contribute to erectile function; beta-adrenergic blockers sometimes have the side effect of erectile dysfunction. Peripheral Nervous System 229 Sympathetic fibers Preganglionic Postganglionic Parasympathetic fibers Preganglionic Postganglionic Afferent fibers Solitary tract nucleus Dorsal vagal nucleus Medulla oblongata Vagus (X) nerve Spinal ganglion Gray ramus communicans Descending fibers Ascending fibers White ramus communicans Ventral ramus of T11 (intercostal nerve) T10 Spinal cord (T10 to L1) T11 T12 Sympathetic trunk ganglia L1 Lesser thoracic splanchnic nerve Lowest thoracic splanchnic nerve 1st lumbar splanchnic nerve Celiac plexus Aorticorenal ganglion Renal ganglion Renal artery and plexus Intermesenteric plexus Superior hypogastric plexus (presacral nerve) Hypogastric nerve Sacral plexus Pelvic splanchnic nerves S4 S2 S3 Inferior hypogastric (pelvic) plexus 9. Noradrenergic postganglionic fibers travel in fascicles that accompany the upper ureteric, renal, pelvic, calyceal, and segmental branches of the renal vessels. Parasympathetic nerve fibers are distributed to renal ganglia by the vagus nerve and pelvic splanchnic nerves via a longer course through other plexuses. The sympathetic nerve fibers stimulate renin secretion (and the reninangiotensin-aldosterone system); decrease the glomerular filtration rate; stimulate proximal tubule and collecting duct sodium chloride reabsorption (further elevating blood pressure); and stimulate contraction of the ureters. Parasympathetic nerve fibers cause relaxation of smooth muscle in the pelvis, the calyces, and the upper ureter and, when accompanied by decreased sympathetic activation, may lead to a decrease in blood pressure. Parasympathetic innervation derives from the S2S4 intermediate gray of the spinal cord and distributes to intramural ganglia in the wall of the bladder via pelvic splanchnic nerves. Sympathetic nerve fibers relax the detrusor muscle and contract the trigone and the internal sphincter. Parasympathetic nerve fibers contract the detrusor muscle and relax the trigone and the internal sphincter, thus stimulating emptying of the bladder. Sensory nerves also are present in the bladder; when the bladder is stretched because it is full, these nerves can initiate the sensation of the need to empty the bladder. Later in the course of parasympathetic damage, a flaccid bladder with incomplete emptying and incontinence can occur. Sensory neuropathy also can result in an enlarged bladder caused by incomplete emptying because of the inability of the patient to sense fullness and by the decreased sense of urgency for urination. Peripheral Nervous System Sympathetic trunk and ganglia Greater splanchnic nerve (T59) T10 Gray ramus communicans T11 White ramus communicans T12 Lesser splanchnic nerve Least splanchnic nerve L1 Upper lumbar splanchnic nerves L2 L3 Gray ramus communicans L4 Testicular artery and plexus Superior hypogastric plexus Hypogastric nerves Intermesenteric (aortic) plexus Inferior mesenteric ganglion Celiac ganglia 231 Superior mesenteric ganglion Left aorticorenal ganglion Renal ganglion Testicular artery and plexus Ductus deferens and plexus Inferior extent of peritoneum Pelvic splanchnic nerves S1 S2 S1 Ductus deferens and plexus Pelvic splanchnic nerves Sacral plexus S2 S3 S4 S5 Sacral plexus S3 S4 S5 Pudendal nerve Inferior hypogastric (pelvic) plexus Vesical plexus Prostatic plexus (Greater and lesser) cavernous nerves of penis Pudendal nerve Posterior nerves Sympathetic Presynaptic of penis fibers Postsynaptic Epididymis Parasympathetic Presynaptic fibers Postsynaptic Testis Afferent fibers 9. Parasympathetic innervation derives from the S2S4 intermediate gray of the spinal cord and travels to the inferior hypogastric plexus via pelvic splanchnic nerves.
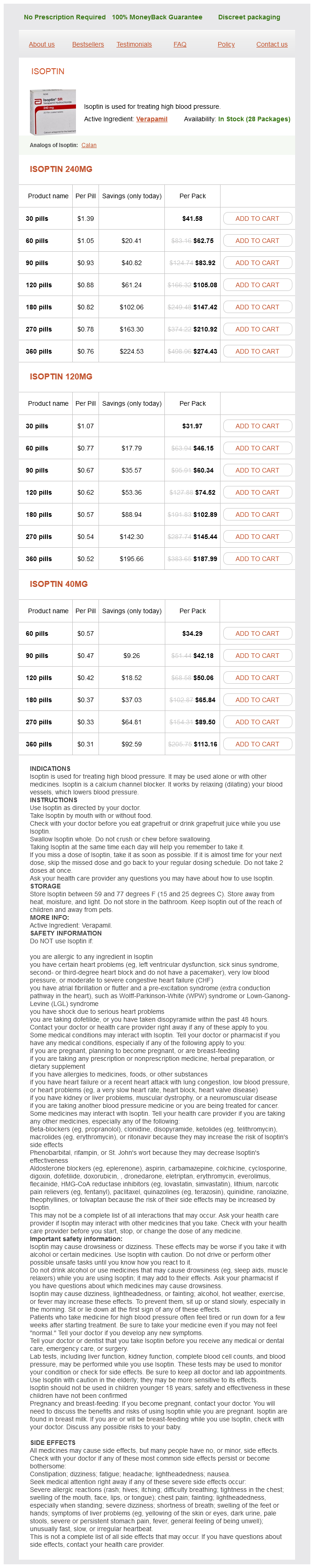
Isoptin Dosage and Price
Isoptin 240mg
- 30 pills - $41.58
- 60 pills - $62.75
- 90 pills - $83.92
- 120 pills - $105.08
- 180 pills - $147.42
- 270 pills - $210.92
- 360 pills - $274.43
Isoptin 120mg
- 30 pills - $31.97
- 60 pills - $46.15
- 90 pills - $60.34
- 120 pills - $74.52
- 180 pills - $102.89
- 270 pills - $145.44
- 360 pills - $187.99
Isoptin 40mg
- 60 pills - $34.29
- 90 pills - $42.18
- 120 pills - $50.06
- 180 pills - $65.84
- 270 pills - $89.50
- 360 pills - $113.16
Anteroposterior pulse pressure heart failure isoptin 40 mg order otc, lateral, and spot films of L5S1 area may be of use in selected patients. Special Tests: Computed tomography, magnetic resonance imaging, or myelography only for specific cause. Diagnostic Procedures: History and physical examination (with special attention to the back and hips). Prevention/Avoidance: Muscle-strengthening exercises, care in lifting, maintenance of reasonable weight. Possible Complications: Chronic low back pain, pain medication dependence, and dependency state resulting from secondary gain. Expected Outcome: Gradual improvement with analgesics, muscle relaxants, massage, and exercise (16 weeks). Surgery versus nonsurgical treatment of lumbar spinal stenosis: a randomized trial. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: a randomized clinical trial. A randomized, placebocontrolled trial of bupropion sustained release in chronic low back pain. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Treating acute low back pain with continuous low-level heat wrap therapy and/or exercise: a randomized controlled trial. Some relief is gained when the fetus descends into the pelvis in the last days of the gestation, but the sudden return to upright and the constant bending to care for a newborn make this improvement short lived. Valdecoxib is as efficacious as diclofenac in the treatment of acute low back pain. Spinal muscle evaluation in healthy individuals and low-back-pain patients: a literature review. Association of early imaging for back pain with clinical outcomes in older adults. Cost-utility analysis of physiotherapy treatment compared with physiotherapy advice in low back pain. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Prevention/Avoidance: Avoidance of excessive sun exposure, especially blistering sunburn. Possible Complications: Disease progression or spread, cosmetic damage by excision. Expected Outcome: Prognosis is based on staging-5-year survival if no local or distant spread (70%); less than 0. Although any malignant metastasis to the fetus is rare, melanomas represent up to one-third of all malignancies found. Melanoma is one of the few malignancies that spreads to the placenta, and metastatic melanoma is a threat to both the fetus and mother. If a woman has had melanoma, it is recommended that she wait for 2 or more years before planning a pregnancy. Primary malignant melanoma of the vagina: a case report and review of the current treatment options. Cutaneous melanoma: interferon alpha adjuvant therapy for patients at high risk for recurrent disease. Palpation of the anterior abdominal wall may demonstrate thickening or tenderness that is suggestive of the diagnosis. Description: Myofascial syndrome is characterized by muscular and fascial pain and is associated with localized tenderness and pain referred to sites that are often remote. Myofascial pain syndromes and fibromyalgia frequently demonstrate trigger-point involvement. These syndromes may present as chronic lower abdominal or pelvic pain that is easily confused with gynecologic causes. Several studies indicate that women who have a family member with fibromyalgia are more likely to have fibromyalgia themselves. Pathologic Findings A trigger point is often felt as an extremely taut band of muscle (normal muscle should not be tender to firm compression and does not contain taut bands). Compression of this site elicits local tenderness and often reproduces the referred pain. Most trigger points are located at or near areas of moving or sliding muscle surfaces, although they are not limited to these locations. Genetics and physical and emotional stressors are possible contributory factors to the development of the illness. A 22-gauge needle is selected for trigger-point injections because of the amount of movement within the tissue that is often required to probe for and block the taut muscle bundle. The length of the needle should be sufficient to allow the entire trigger point to be reached without indenting the skin or having the hub at the skin surface. Superficial trigger points may also be treated with a "spray-and-stretch" technique (the area overlying the trigger point is sprayed with a coolant or freezing spray [eg, ethyl chloride] for several seconds, and the muscle is forcibly stretched by passive extension). Directed pelvic floor physical therapy has shown good effect and for many represents first-line therapy. Trigger points may be found throughout the body but are most common in the abdominal wall, back, and pelvic floor when pelvic pain is the symptom.