Lansoprazole
General Information about Lansoprazole
Another widespread condition that's handled with Prevacid is erosive esophagitis, a situation during which abdomen acid damages the liner of the esophagus, inflicting inflammation and discomfort. This can occur as a end result of acid reflux disorder, a condition during which abdomen acid flows again up into the esophagus, causing a burning sensation within the chest, commonly generally known as heartburn. Prevacid helps to decrease the quantity of acid within the stomach, lowering the chance of acid reflux and permitting the esophagus to heal.
In conclusion, Prevacid, or lansoprazole, is a broadly prescribed medication for the remedy of abdomen and intestinal ulcers, erosive esophagitis, and other conditions involving extreme stomach acid. By decreasing the amount of acid produced in the abdomen, it offers aid from symptoms and promotes healing. It is essential to take Prevacid as directed and to seek the guidance of a well being care provider if you experience any unwanted side effects or have any concerns.
Prevacid may interact with other drugs, particularly blood thinners and certain antibiotics and antidepressants. It is crucial to inform a healthcare professional of all current medicines earlier than starting Prevacid to keep away from any potential interactions.
Prevacid can be used to deal with a rare situation referred to as Zollinger-Ellison syndrome, in which tumors in the pancreas and small gut trigger the stomach to supply excessive amounts of acid. This can result in severe abdomen ulcers and other digestive issues. Prevacid is prescribed to reduce the quantity of acid within the stomach, offering aid from symptoms and helping to forestall complications from the condition.
Lansoprazole, generally identified by its brand name Prevacid, is a proton pump inhibitor (PPI) medication used to lower the quantity of acid produced in the abdomen. It is primarily prescribed to treat and stop stomach and intestinal ulcers, in addition to to alleviate symptoms of conditions involving excessive abdomen acid such as erosive esophagitis and Zollinger-Ellison syndrome.
Prevacid is on the market in numerous varieties, together with capsules, orally disintegrating tablets (ODT), and oral suspension. It is often taken as quickly as a day, earlier than a meal, and should be swallowed whole for capsules and ODT, or blended with applesauce for ODTs. The oral suspension may be taken alone or mixed with water before use. It is necessary to observe the dosage and instructions supplied by a healthcare skilled.
The stomach naturally produces acid to assist within the digestion of meals. However, when an excessive quantity of acid is produced, it can result in various health issues. Stomach ulcers, for instance, are sores that develop on the liner of the abdomen and may trigger burning pain and discomfort. If left untreated, they'll lead to severe problems corresponding to bleeding and perforation of the abdomen wall. Prevacid works by inhibiting the production of acid, offering relief and permitting the ulcers to heal.
As with any medication, Prevacid might trigger unwanted effects. These can include headache, nausea, diarrhea, and abdominal ache. More serious unwanted aspect effects could occur in rare circumstances, such as allergic reactions or increased threat of bone fractures. It is essential to debate any potential unwanted effects with a physician before starting Prevacid.
Although these therapeutic indications dominate the use of ureteroscopes www gastritis diet com 15 mg lansoprazole, the addition of working channels and deflection also improved their diagnostic capabilities. It is now possible to completely inspect the intrarenal collecting system, and through the working channel sample fluid for cytology and pass biopsy forceps to sample any abnormal tissue identified. The use of ureteroscopy as a diagnostic tool will grow as ureteroscopes continue to improve their imaging abilities, maneuverability, and durability. The diameter of ureteroscopes has decreased over the years of development, which greatly increases our ability to perform ureteroscopy without prior ureteral dilation, allowing clearer inspection of the untouched ureteral urothelium [3]. As the invasiveness of ureteroscopy decreases, there will be little reason to rely on radiologic studies alone when the urothelium of the upper urinary tract can be safely inspected and sampled. This chapter will discuss the diagnostic uses of ureteroscopy, the specific technical nuances of diagnostic ureteroscopy, and current results of ureteroscopy for evaluating hematuria. Indications Ureteroscopy can be used diagnostically to investigate any condition that may involve the upper urinary tract. Ureteroscopy allows urologists direct visualization, fluid sampling, and tissue sampling of the upper urinary tract. Any evaluation for conditions that might benefit from these diagnostic interventions should be considered for ureteroscopy. Common indications for diagnostic ureteroscopy include evaluating patients with unexplained recurrent or persistent urinary tract infections, persistent positive cytologies, upper urinary tract filling defects, and hematuria [4, 5]. Upper urinary tract filling defects Excretory urography is the most common imaging modality for evaluating patients with hematuria. Despite improvements in upper urinary tract imaging for patients with hematuria, the evaluation of the upper urinary tract filling defects identified on imaging studies remains one of the most common indications for diagnostic ureteroscopy. Direct ureteroscopic inspection alone often provides the diagnosis when evaluating upper urinary tract filling defects [4]. Upper urinary tract calculi are easily distinguishable from soft tissue lesions, and treatment can be rendered using a holmium laser in the same setting. Extrinsic filling defects can often be determined visually with the appearance of compression of the ureter in the absence of any intrinsic mass in the ureteral lumen. When the ureter is extrinsically compressed by a venous structure, the ureteral lumen is distensible during ureteroscopic inspection, whereas extrinsic compression from an artery often results in visible pulsations. In this setting, most filling defects will be soft tissue in nature and should be considered cancer until proven otherwise. When evaluating any soft tissue lesion with concern for possible urothelial cancer, the diagnosis should be based on visual appearance, cytologic evaluation, and biopsy [6]. The most critical factors in deciding the course of treatment are the stage and grade of the tumor. If an obvious source of the hematuria cannot be determined through conventional studies, the condition is referred to as benign essential hematuria [5, 8]. Patients with benign essential hematuria can have frequent bouts of gross hematuria with clots and renal colic; otherwise, their long-term course is generally benign. Additional radiologic studies are frequently done to evaluate patients with benign essential hematuria. These additional imaging studies are usually of low yield because the most common vascular lesions causing benign essential hematuria are small venous abnormalities and hemangiomas [9]. These are seen better on endoscopic inspection of the upper urinary tract and will usually be missed on vascular imaging studies. Other causes of chronic hematuria, including loin pain hematuria syndrome and the Nutcracker syndrome, should be considered [1012]. Loin pain hematuria syndrome patients have intermittent pain and microscopic or gross hematuria. Although this diagnostic entity somewhat overlaps benign essential hematuria, loin pain hematuria syndrome has no specific anatomic findings and a significant psychiatric component, specifically associated with somatoform disorder. It is caused by venous hypertension of the left kidney due to compression of the left renal vein, between the aorta and the superior mesenteric artery [13]. Diagnosis is generally made by demonstrating venous hypertension during venography studies with a pressure drop beyond the point of compression of the left renal vein. Treatment is surgical, with repositioning of the left renal vein or renal autotransplantation. In the past, some patients with benign essential hematuria required treatment with partial or total nephrectomy. With the advent of current flexible ureteroscopic instruments and techniques, most of these patients can be evaluated and successfully treated ureteroscopically. The two most common ureteroscopic findings are renal hemangioma and venous abnormalities of the calyces ("minute venous ruptures"). Fortunately, stage and grade correlate closely, and accurate grading of the tumor is heavily relied upon to guide treatment options [7]. Cytology and biopsy are complementary tools in diagnosing and grading these tumors. While cytology is specific, it is less sensitive because most low-grade lesions will be missed. Thus, fluid aspirations for cytology and biopsies should be obtained from any suspicious lesion during ureteroscopy. A more extensive description of tissue sampling techniques is given in Chapter 41. Benign essential hematuria Evaluating patients with hematuria is one of the most common consultations for urologists.
There are gastritis symptoms after eating purchase lansoprazole canada, however, some characteristic symptoms that should be screened for in all patients in whom the diagnosis is suspected. Flashing lights in the vision, epigastric pain and restlessness are all symptoms that warrant prompt investigation. Senior obstetric, anaesthetic and midwifery personnel should be requested to attend urgently. Haematology input should be requested, but it is rare that they will need to attend labour ward, and will be more effective co-ordinating the blood bank response. Ultrasound scan of the uterus may be useful in identifying problems such as retained products of conception, but will not form part of the initial management. The abdomen should be tilted (for example with a Cardiff wedge) to relieve caval compression and increase venous return. The weight of the mammary glands increases in late gestation and may alter the pressures required to achieve adequate ventilation. The functional lung capacity is reduced, however, and the diaphragm may be splinted by the gravid uterus. If initial resuscitative efforts are not successful by 4 minutes after cardiac output is lost, then a perimortem Caesarean section should be performed, primarily to increase the chances of successful maternal resuscitation. All vitamins other than vitamin K are found in breast milk; routine supplementation is therefore given to neonates at birth. Operative delivery (whether vaginal or abdominal) carries a higher risk than spontaneous delivery. If the membranes are not ruptured then there is no increased risk associated with prolonged pregnancy. Perineal pain may be due to increased spontaneous tears, haematoma formation or episiotomy repair. Obstetric palsy may be due to exaggerated lithotomy position during instrumental delivery. Puerperal infection is more common where instrumentation of the genital tract has occurred. There is a theoretical risk of teratogenicity from psychotropic medication, but this may be outweighed by the chance of relapse. Inpatient care post-natally should be facilitated in a mother and baby unit if possible. Any visible jaundice in the first 24 hours must be urgently investigated and assumed to represent haemolysis unless proven otherwise. The initial inflation breaths are given at higher pressure and for longer than subsequent maintenance breaths. Naloxone or blood transfusion may be considered by the attending paediatrician where appropriate. There is no time limit imposed on informed consent, and quick decisions may be required in difficult situations on the labour ward. Verbal consent is adequate to carry out a procedure if time pressures demand this, but written documentation of consent is preferred where possible. A symphysisfundal height measurement should be plotted at every visit after 16/40. Normal fetal development and growth 4 A woman is found to have oligohydramnios at 30/40. Antenatal care 6 A woman contacts her midwife with concerns regarding fetal well-being at 32/40 in a previously normal pregnancy. Antenatal imaging and assessment of fetal well-being 7 A thirty-seven-year-old woman attends for a routine dating scan. Which of the following features should help to reassure the doctor that this is a normal trace Single best answer questions 53 d) There are no significant accelerations of the fetal heart on the 30-minute recording. She has continued to use heroin throughout her pregnancy, but has reduced her smoking. Twins and higher multiple pregnancies 13 a) b) c) d) e) Which of the following is not an increased risk in multiple pregnancy Late miscarriage and early birth 14 a) b) c) d) e) Which statement is most accurate regarding cervical cerclage In a high-risk patient it should be performed as soon as practical after confirmation of intrauterine pregnancy. Is a suitable procedure in any woman with a history of delivery between 20 and 26 weeks. In making a plan for the management of her pregnancy, which step is least appropriate The main complications for the fetus include growth restriction and fetal bradycardia. The following are correct regarding thalassaemias except: They represent the most common genetic blood disorders. Perinatal infections 20 You are counselling a pregnant woman in the antenatal clinic who has known hepatitis with regard to fetal risk. Single best answer questions 55 21 a) b) c) d) e) Choose the best option with regard to a non-immune pregnant woman with an exposure to chickenpox: Should be given the varicella zoster vaccine as soon as possible after exposure. Should be given varicella zoster immunoglobulin as soon as possible after exposure. Labour 22 a) b) c) d) e) Choose the option that is the greatest contraindication to epidural anaesthesia: Previous treatment with anticoagulants. Operative intervention in obstetrics 23 a) b) c) d) e) Which of the following is the main advantage to performing a medio-lateral episiotomy Obstetric emergencies 25 a) b) c) d) e) Choose the option that is less common after Caesarean delivery than after vaginal delivery: Pulmonary embolism. Psychiatric disorders and the puerperium 28 a) b) c) d) e) Which statement is true regarding mental illness in pregnancy The majority of women with postpartum psychiatric disorders have pre-existing mental illness. In women with pre-existing psychiatric disorders, these usually improve during pregnancy. Neonatology 29 a) b) c) d) e) the components of the Apgar score include all except: Appearance.
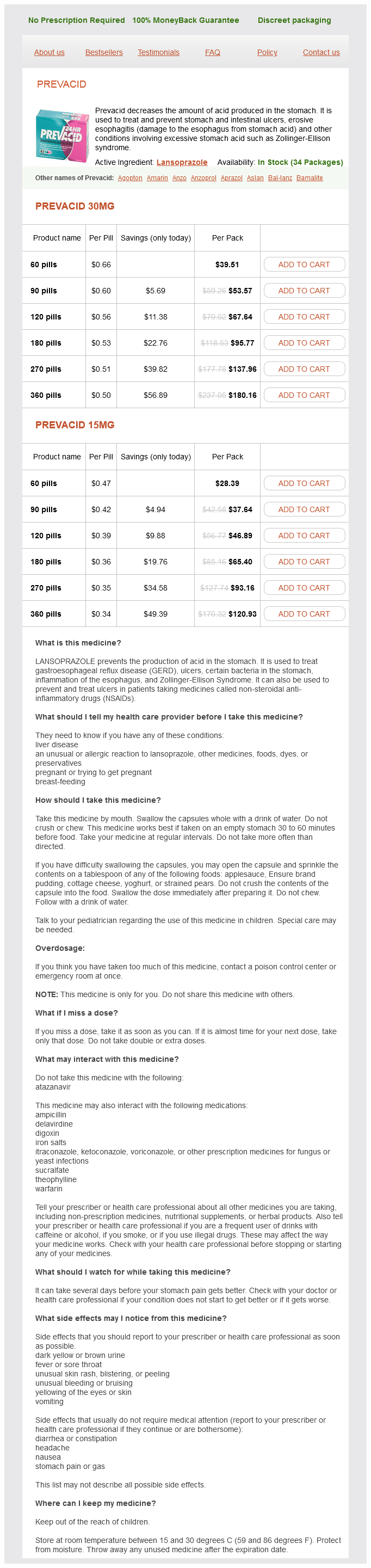
Lansoprazole Dosage and Price
Prevacid 30mg
- 60 pills - $39.51
- 90 pills - $53.57
- 120 pills - $67.64
- 180 pills - $95.77
- 270 pills - $137.96
- 360 pills - $180.16
Prevacid 15mg
- 60 pills - $28.39
- 90 pills - $37.64
- 120 pills - $46.89
- 180 pills - $65.40
- 270 pills - $93.16
- 360 pills - $120.93
Tract dilation in children can be carried out with serial dilation or balloon dilation viral gastritis diet buy lansoprazole 30 mg fast delivery. The mini-perc access system uses an 11F × 10 cm peel-away vascular access sheath with an exposed trocar length of 1 cm. The sheath is inserted in to the collecting system over an access wire and does not need sequential or balloon tract dilation. The mini-perc technique reduces the size of the percutaneous tract significantly and yet can still be effective for clearing stones [22]. It is also associated with decreased blood loss, increased maneuverability, and shorter hospital stay [23], but requires mandatory use of pediatric instruments and a greater degree of stone fragmentation prior to extraction. Impacted stone in entry calyx Renal stones tightly impacted within the intended entry calyx present a challenge for percutaneous surgery. The access can be aided by injection of contrast, relying on the generated pressure to create space around the stone [26], the use of hydrophilic wire(s) or angled-tip catheters, such as a Kumpe catheter to navigate around the stone. The main challenge in dilating the tract is to ensure the dilator can obtain enough purchase within the calyx to allow insertion of the working sheath. This maneuver will often create enough space to permit a successful reinsertion of the balloon catheter. Retroperitoneal scarring Retroperitoneal fibrosis resulting from previous surgery or retroperitoneal inflammation can present a challenge during nephrostomy tract dilation. Balloon dilators used in this situation have been associated with failure rates of 1750% [24, 25]. Balloon failure cases can be salvaged in most situations with the use of Amplatz or metal dilators. Alternatively, when dense perinephric scarring is encountered, the use of a facial incising needle can also be used to aid tract dilation. Care must be taken not to inadvertently lacerate the subcostal or intercostal neurovascular bundle on the inferior rib margin [26]. Among thin patients, care must be taken not to advance the needle too deeply, so as to avoid reaching and lacerating the renal parenchyma. A recent report has described the use of a cutting balloon for cases of heavy retroperitoneal scarring [27]. Although described as safe and successful in this case report, its safety in a wider context remains to be determined. Potential complications Hemorrhage Acute hemorrhage can originate from four sources: intercostal vessels, renal parenchymal vasculature, or branches of the renal vein or renal artery adjacent to the pelvicalyceal system. The most clinically significant bleeding related to percutaneous tract dilation is due to over-advancement of the dilating instrument, resulting in splitting of the infundibulum. This occurrence can be avoided by 238 Section 2 Percutaneous Renal Surgery: Selection of Access and Dilation Conclusions Acute dilation of the percutaneous nephrostomy tract is a safe and efficient technique that permits percutaneous renal surgery. A variety of dilating techniques and instruments can be used, each with specific advantages and risks. The dilation should always be carried out over a guidewire and under radiologic imaging. The choice of equipment will depend on patient profile, surgeon preference and expertise, local instrument availability, and costs. Study Transfusion rate (%) 2 Dilation technique Metal telescopic Metal telescopic Metal telescopic Metal telescopic Amplatz Amplatz Amplatz Amplatz Balloon Balloon Balloon Balloon Balloon Balloon Balloon Wezel et al. Influence of technique of percutaneous tract creation on incidence of renal hemorrhage. Regardless of the dilating system used, the intention should then be to place the widest part of the dilator in to the entry calyx, but not in to the infundibulum. Renal pelvis perforation the most common cause of renal pelvis perforation is the aggressive use of serial dilators. Renal pelvis perforation can also occur due to initial transgression of the puncture needle and inappropriate guidewire positioning. Acute angulation, often associated with lower renal pole entry, and guidewire kinking can also contribute to renal pelvis perforation. Initial advancement of the guidewire down the ureter and in to the bladder facilitates dilation and greatly reduces the risk of this complication. The perforation is usually recognized intraoperatively by contrast extravasation on fluoroscopy. Once recognized, it requires termination of the procedure and placement of a ureteral stent and a nephrostomy tube. Use of a modified syringe barrel to ensure control of the Apmlatz sheath during percutaneous nephrolithotomy in obese patients. Percutaneous management of renal calculi: experience with percutaneous nephrolithotomy in 60 children. Percutaneous nephrolithotomy: primary patients versus patients with history of open renal surgery. Percutaneous nephrolithotomy on patients with or without a history of open nephrolithotomy. Percutaneous nephrolithotomy in patients with previous open nephrolithotomy: One-shot versus telescopic technique for tract dilation. Does previous open nephrolithotomy affect the outcome of percutaneous nephrolithotomy Classification of percutaneous nephrolithotomy complications using the modified clavien grading system: looking for a standard.