Linezolid
General Information about Linezolid
Linezolid, generally recognized by its model name Zyvox, is a powerful antibiotic used to treat infections brought on by Enterococcus and Streptococcus bacteria. It belongs to a class of antibiotics called oxazolidinones, which work by inhibiting protein synthesis within the bacteria, finally leading to their dying. Linezolid has been proven to be efficient towards even probably the most drug-resistant strains of micro organism, making it a life-saving treatment for a lot of sufferers.
Linezolid works by binding to the bacterial ribosomes, that are liable for protein synthesis. By blocking this process, the bacteria are unable to grow and multiply, and eventually die off. This mechanism of motion, coupled with its broad spectrum of exercise, has made Linezolid a go-to medication for many physicians when faced with difficult-to-treat infections.
In conclusion, Linezolid, also called Zyvox, is a strong antibiotic that has revolutionized the therapy of infections attributable to Enterococcus and Streptococcus bacteria. Its broad spectrum of exercise, availability in oral and intravenous varieties, and effectiveness towards drug-resistant strains have made it an indispensable treatment in the medical area. However, it is essential to make use of this medicine responsibly to forestall the event of resistance and to report any potential side effects to a healthcare professional. As with all antibiotics, correct use and consciousness of the potential dangers are essential to keep this medication effective.
Another advantage of Linezolid is its availability in both oral and intravenous types. This makes it a versatile antibiotic, as it might be used in both hospital and outpatient settings. The oral formulation of Linezolid can be beneficial for sufferers who require long-term treatment, as it can be taken at residence somewhat than having to stay in a hospital for intravenous administration.
However, like all antibiotics, Linezolid does have its drawbacks. One major concern is the event of resistance. As with any antibiotic, the overuse or misuse of Linezolid can lead to the emergence of drug-resistant bacteria. This is why it is important to make use of this treatment solely when prescribed by a healthcare professional and to proceed the course of therapy as directed. Additionally, Linezolid can have some unwanted side effects, corresponding to nausea, diarrhea, headache, and dizziness. In rare cases, it can also cause a lower within the variety of blood cells, which can result in anemia and other blood-related complications.
Despite these potential drawbacks, Linezolid remains an important treatment within the struggle against bacterial infections. Its effectiveness in opposition to drug-resistant strains of micro organism has made it a crucial tool in the remedy of great infections. Moreover, it has been confirmed to have a low fee of resistance compared to other antibiotics, making it a extra sustainable option for long-term use.
One of the necessary thing options of Linezolid is its broad spectrum of exercise. It is effective towards gram-positive bacteria, together with strains that are immune to different antibiotics similar to methicillin-resistant Staphylococcus aureus (MRSA). This makes it a first-line remedy alternative for critical infections caused by these micro organism, such as pores and skin and soft tissue infections, pneumonia, and even sepsis.
Effects on other organs Heart After 6 months of AgalA therapy in a double-blind placebo-controlled randomized trial there was a 20% decrease of myocardial Gb3 compared to a 10% increase in the placebo group virus that causes cervical cancer 600 mg linezolid otc. Examination of the myocardial histology after 6 months of AgalB showed almost complete clearance of Gb3 deposits from all cell types except the cardiomyocytes (Thurberg et al. Overall, there was a significant improvement in left ventricular mass or a stabilization. Renal transplantation was initially thought to be a potential treatment for alleviating some of the symptoms of Fabry disease by providing a source of enzyme, However that is not the case with circulating alpha-galactosidase remaining the same after as before transplantation (van den Berg et al. The 5-year graft survival has been reported as 74% and superior to a non-Fabry group (69%) but comparable with a matched group. Patient survival at 5 years was 81%, a little less than the 90% in a matched group (Shah et al. In fact, the results are so good that renal transplantation should be considered in all Fabry patients with end-stage renal disease (Cybulla et al. Despite these good results, especially in terms of patient survival, Fabry disease confers a higher risk of death-odds ratio 2. This is better than the diabetic population but not as good as the general non-diabetic patients, and is almost certainly due to the added disease burden from the cardiac and central nervous system complications of Fabry disease (Mignani et al. Women Having recognized that many female heterozygotes can display manifestations of the disease and that some of those may have renal involvement, do female patients respond differently than their male counter parts The answer is that the results for women are not dissimilar to males (Hughes et al. Pregnancy There is no evidence of reduced female fertility in Fabry disease although there has been a report of disorders of the menstrual cycle (Faggiano et al. Similarly, there is no evidence that Fabry disease affects pregnancy although there has been a report of an increased incidence of proteinuria in pregnant women with Fabry disease (Bouwmann et al. Antibodies to recombinant enzyme products There is little doubt that antibodies to both licensed enzyme replacement products are produced, especially in those classical patients who have little or no residual native enzyme. The antibodies cross react so that there is nothing to be gained from switching products if antibodies to one product are thought to be clinically significant. However, in another study the antibodies had a negative impact on urinary Gb3 with the implication that this would be detrimental to clinical outcome (Linthorst et al. Similar results were found when skin biopsies were examined with re-accumulation of Gb3 deposits in the presence of high antibody titres (Hollak and Linthorst, 2009). In a comparative study between agalsidase alpha and beta, beta-galactosidase A antibodies were measured as well as clinical outcome and Gb3 levels in urine and plasma in 52 patients after 12 months of treatment. Reviewing this, Warnock and colleagues are clear that treatment should be started as soon as a diagnosis is made in patients where no enzyme is detected as these are the severe classical cases. In other patients, treatment should start as soon as the first signs or symptoms appear and, from a renal perspective, this would be when proteinuria (or micro-proteinuria) is first detected (Warnock et al. It has been known for some time that typical renal lesions can be identified on histology in children (Tondeur and Resibois, 1969; Gubler et al. More recently these early changes have been correlated with small degrees of proteinuria in children, adolescents, and young adults (Tøndel et al. These studies are, however, only slightly indicative of the possibility that a dose of 1 mg of AgalB is better than 0. Despite this, more studies are needed and, in time, it may be that patients will require different doses at different periods of their management or with different degrees of organ involvement. The message should be that whatever dose of agalsidase is used there needs to be careful monitoring of progress with repeat renal biopsies if there is a poor clinical effect despite optimum adjuvant therapies. However, there is, as yet, no standardized method for measuring antibodies to these enzymes as well as the difficulty in the interpretation of results. Comparison of AgalA with AgalB There is virtually no difference between the two products when their structure and composition is considered. AgalB has slightly more sialylated oligosaccharides and a higher level of phosphorylation, but in a mouse model this did not seem to be significant (Lee et al. However, this does not take into consideration the fact that mannose 6-phosphate receptors are not the only mode of entry into the cell for enzymes and that the two products may enter different cell types in different ways and to different degrees (Prabakaren et al. However, there were many treatment failures in the relatively small number of patients studied and this was almost certainly due to the age of the patients included in the study and the severity of the disease at baseline (Vedder et al. At the end of the study there was no statistical difference between the doses but there was a trend towards the highest dose being most effective (Hughes et al. A trial has also been reported where 21 male patients were treated for 6 months with AgalB at a dose of 1 mg/kg body weight every 2 weeks and then the dose reduced to 0. The usual renal parameters and Gb3 were measured as well as examining renal and skin histology. While 100% of patients cleared deposits from interstitial capillary endothelial on the 1 mg dose, only 90% remained clear on the reduced dose and when seven other renal cell types were examined, 70% remained clear on the lower, 0. In June 2009 there was an interruption to the supply of AgalB and many patients either had their dose of enzyme reduced or were changed to AgalA in the standard dose of 0. Seven male and three female patients who had received AgalB at the standard 1 mg/kg dose for at least 48 months were changed to AgalA again at the standard dose of 0. In Australia, 40 patients who had been on AgalB for at least 2 years had their dose initially reduced by 50% and then by a further 30%. A similar study was performed in the Dutch cohort where 35 patients were receiving AgalB at the time of the shortage and either received a lower dose of AgalB or changed to the standard 0. However, this can be mitigated by the use of home therapy that is now standard practice in many countries and has been reported as safe and efficacious (Schiffmann et al. Fabry disease in children: correlation between ocular manifestations, genotype, and system clinical activity.
Timing of transfer Timing of transfer of care should take into account chronological age and maturity ear infection 1 year old linezolid 600 mg purchase visa, adolescent readiness, medical stability, psychosocial issues, and the views of the adolescent and their parents or guardians. In the United Kingdom, transfer to adult services usually occurs between 16 and 18 years of age. However, this is interpreted flexibly in some areas, although practice varies internationally and some adult units do not have trained staff to manage young adults before their 18th birthday. The American Society of Adolescent Medicine very reasonably recommends that services should be appropriate for both the chronological age of the patient and development attained. Historically, young adults were transferred to adult nephrological care at a single point in time with movement to a new healthcare setting, provider, or both, without a preceding transition process. A preparation period and education programme may help the young patient to acquire the necessary knowledge and skills to Adherence Many professionals discussing the difficulties of managing adolescents with chronic disease will highlight the importance of adherence to recommended therapy. Cumulative graft survival 20042009 20002004 19901999 19791989 Where should they attend Clinic attendance may be hampered by young adults being surrounded by much older, sicker patients, but also by being in an environment that was clearly created for young children in mind, as is often the case for paediatric facilities. Visits to and meeting staff and/or patients from the adult unit can help to allay fears during the preparation for transfer. The transition process itself depends on the modality of renal therapies and requirement for nephrological follow-up. This may be relatively simple for patients with chronic kidney disease, or more complex for adolescents with end-stage kidney disease who require in-centre haemodialysis (waiting for a slot to dialyse in an adult satellite unit), or home haemodialysis or peritoneal dialysis. There may be a tension between providing local care and attendance at a specialist clinic such as a transplant clinic, or one for a specific group of diseases, or indeed a transition or young adult clinic. Transition programmes Modern transition programmes view transfer as only one component, with transition as an anticipated, coordinated process of movement from child-centric to adult-oriented healthcare systems over a prolonged period of time. This smooth transition of care for adolescents with renal disease between paediatric and adult nephrology services should involve a preparatory phase, the transfer event itself and post-transfer phase. Parents may be reluctant to leave familiar staff and clinic surroundings and resist attempts by the adult service to enhance the self-advocacy of their child, if not adequately prepared. The development of young adult clinics in adult nephrology may help to bridge the gap between paediatric and adult services and enhance the education and preparation of young adults from a parent-focused to patient-focused service. A good transition programme should individualize care on a background model of transitioning young adults with renal disease. The framework should involve adolescent trained physicians, surgeons, nurse specialists, pharmacists, and allied health professionals, including the psychosocial team and other multidisciplinary team members, such as youth workers. Ideally both paediatric and adult professionals provide ongoing care in a joint clinic from adolescence through to adulthood, the duration of which can be individualized. Patients then benefit both from experts in paediatric diseases and the appropriate management of more pertinent adult issues, such as sexual health, fertility issues, and cardiovascular disease. During these specialist clinics, educational sessions are available for both patients and their parents, who have informal visits to the adult hospital setting and its inpatient and outpatient clinic facilities where they see adult staff previously introduced to them by the paediatric staff. This facilitates familiarity with the new adult team prior to embarking on formal outpatient clinic attendances with investigations, such as blood tests (which may be an issue for some adolescent patients). Improved patient outcomes Transition programmes are set up to improve patient-related outcome measures as well as patient experiences. However, improving patient outcomes can only be achieved by careful preparation and management. They may lack maturity, have adherence issues, and an ongoing dependence on parents or guardians. They need to work towards a good long-term outcome, which depends on the young adult managing their own care in a safe and reliable manner. Barriers There may be barriers to successful transition from the healthcare system, which may be related to personnel or time and financial constraints of services. However, unsuccessful transfers can be very expensive in hospital admissions, lost allografts, and lost lives. Paediatric medical and nursing staff may have an emotional attachment to patients and lack confidence in the potential care given by health professionals in the adult clinic due to differences in the attitudes and priorities of adult services-or simply because they do not know the staff there. They may be concerned regarding different dynamics of consultation (such as the presence of parents in consultations). They may also lack confidence in paediatric staff if aware of differences in the attitudes and priorities of paediatric services (such as feeling that the paediatrician has not managed the patient correctly or transferred either too early or too late). Many of the attitudinal barriers can be lowered by involving a limited group of staff in transfers and ensuring good communication in both directions via this team. Improving the transition between paediatric and adult healthcare: a systematic review. Growing pains, Non-adherence with the immunosuppressive regimen in adolescent transplant recipients. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. Treatment adherence in adolescents and young adults affected by chronic illness during the healthcare transition from pediatric to adult health care: a literature review. Transplant outcomes and economic costs associated with patient noncompliance to immunosuppression. Building consensus on transition of transplant patients from paediatric to adult healthcare. Conclusive evidence that contraceptive counselling improves use of, adherence to , or continuation of contraceptive practices is difficult to obtain, particularly in the context of heterogeneous randomized trial data (Lopez et al. However, consensus opinion is that contraceptive counselling improves patient choice, patient satisfaction, and more sustained use of correct contraception (Amy and Tripathi, 2009).
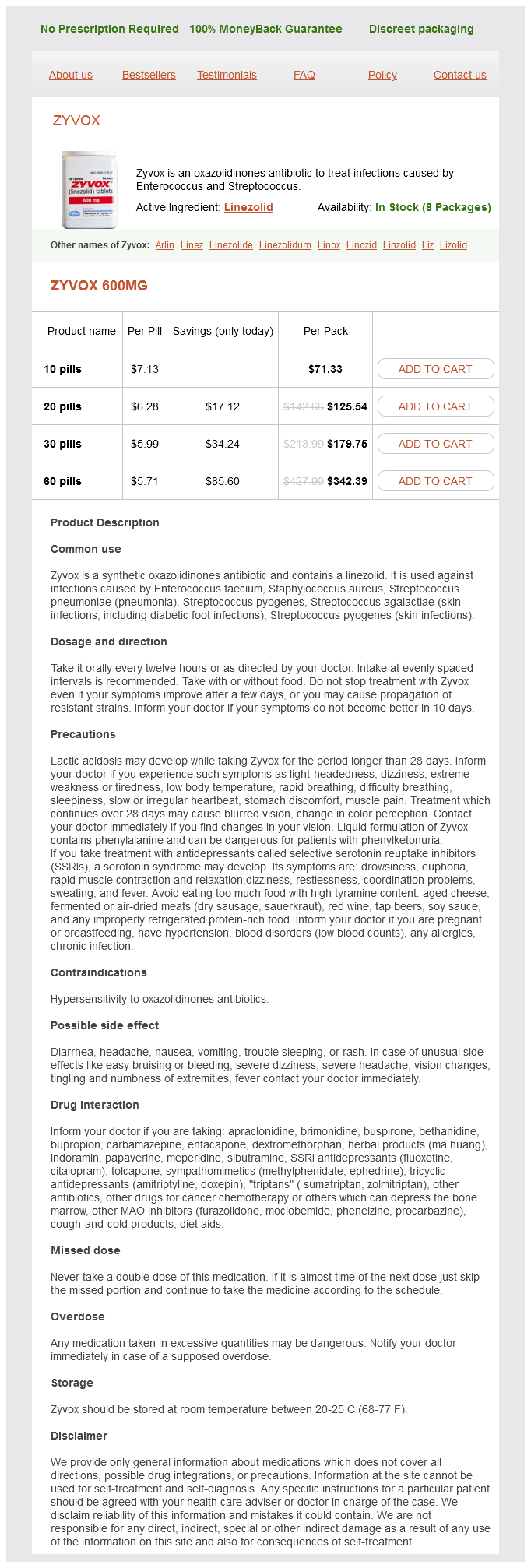
Linezolid Dosage and Price
Zyvox 600mg
- 10 pills - $71.33
- 20 pills - $125.54
- 30 pills - $179.75
- 60 pills - $342.39
Awareness of associated extrarenal manifestations is essential to facilitate appropriate investigation performed regularly infection 5 weeks after breast reduction purchase linezolid 600 mg line. Liver function tests should be performed at least annually and if there is concern of liver disease, ultrasound imaging should be requested. Several pharmaceuticals including vasopressin receptor antagonists (Gattone et al. Clinical trials are ongoing in humans with related cystic kidney diseases; however, this is currently restricted to adults or at least teenagers. Mechanism underlying early anaemia in children with familial juvenile nephronophthisis. Identification of 99 novel mutations in a worldwide cohort of 1,056 patients with a nephronophthisis-related ciliopathy. A study using electron microscopy, immunofluorescence, and a review of the morphological findings. Sayer Introduction the terminology around these diseases has shifted as underlying genetic causes have been discovered. The age of onset is between the third and fifth decades of life but may vary between families and within families. The urine sediment is usually bland; if proteinuria is present it is typically subnephrotic range. Imaging of the renal tract may identify cysts, typically cortical or corticomedullary in location, but these are not essential for the diagnosis. Renal biopsy findings reveal a focal global sclerosis of glomeruli and tubular atrophy with interstitial fibrosis (Kiser et al. This disease locus contained numerous genes, but the exact causative gene within the region defied molecular geneticists and nephrologists for > 10 years until recently, a gene that was missed by massively parallel sequencing approaches was identified. Urinalysis demonstrated minimal proteinuria, renal biopsies revealed tubulointerstitial fibrosis, and renal imaging showed cortical cysts (rather than medullary) in a few cases. A key feature, however, is the incidence of gout which occurs in around half of cases and may commence early, during the second decade of life. The gout is typically out of keeping with the degree of renal dysfunction and its presence in females provides a diagnostic clue. Renal ultrasound may reveal small kidneys and occasional medullary cysts (Dahan et al. Histologically, there is a diffuse tubulointerstitial fibrosis and tubular atrophy (Dahan et al. Umod knockout mice studies suggest a role for uromodulin in the defence against bacterial urinary tract infections (Bates et al. This phenotype was first described in 1960 in a family with early-onset gout, hyperuricaemia, and renal disease (Duncan and Dixon, 1960). The hyperuricaemia is a result of a reduced fractional excretion of uric acid, and predisposes to early gout. It is unknown whether lowering serum uric acid in this way impacts upon the progression of chronic kidney disease. Treatment is supportive care of the chronic kidney disease, management of the anaemia with erythropoietin, and control of hyperuricaemia with xanthine oxidase inhibitors and other agents. An autosomal dominant pattern of disease and the presence of gout may lead to diagnostic confusion in such cases and a molecular genetic diagnosis should be sought where there is diagnostic uncertainty (see Chapter 306). For almost all of these disorders a molecular genetic diagnosis is now possible, if not yet routinely available for all of them. This complication is secondary to a defective reninangiotensin pathway leading to a hypoproliferative anaemia with low erythropoietin levels and may occur as early as 12 months of age. The anaemia due to reduced levels of angiotensin resolves during adolescence, but may recur with the onset of chronic kidney disease. Secondary to low renin levels, the blood pressure may be low and there may be an associated hyperkalaemia. The hyperuricaemia may be explained by a hypothesis where renin deficiency leads to relative aldosterone deficiency which results in a fluid-depleted state leading to increased proximal reabsorption of uric acid and a reduced fractional excretion of urate (Zivna et al. Functional analysis of the mutation demonstrated accumulation of non-glycosylated preprorenin in the cytoplasm leading to ultrastructural damage of the kidney (Bleyer et al. Tamm-Horsfall protein knockout mice are more prone to urinary tract infection: rapid communication. Mutations in the hepatocyte nuclear factor-1beta gene are associated with familial hypoplastic glomerulocystic kidney disease. Abnormal nephron development associated with a frameshift mutation in the transcription factor hepatocyte nuclear factor-1 beta. Solitary functioning kidney and diverse genital tract malformations associated with hepatocyte nuclear factor-1beta mutations. Clinical and molecular characterization of a family with a dominant renin gene mutation and response to treatment with fludrocortisone. The rediscovery of uromodulin (Tamm-Horsfall protein): from tubulointerstitial nephropathy to chronic kidney disease. Autosomaldominant medullary cystic kidney disease type 1: clinical and molecular findings in six large Cypriot families. Characterization and separation of an inhibitor of viral hemagglutination present in urine. Medullary cystic kidney disease type 1: mutational analysis in 37 genes based on haplotype sharing.