Lopinavir
General Information about Lopinavir
Lopinavir, also known by its model name Kaletra, is a medicine that has been extensively used within the remedy of HIV/AIDS. It is a mixture of two medicine, Ritonavir and Lopinavir, each of which belong to the class of anti-viral medicines. This powerful combination has been confirmed to effectively suppress the replication of HIV and improve the standard of life for those residing with the virus.
The use of Lopinavir has significantly improved the prognosis for people dwelling with HIV/AIDS. In mixture with other antiretroviral medication, it has played a critical position in decreasing the viral load in patients and increasing their CD4 cell depend, which is a measure of immune operate. This mixture remedy has also been discovered to decrease the danger of developing opportunistic infections and delay disease progression.
Like all medicines, Lopinavir can cause unwanted side effects, although not everyone experiences them. The mostly reported unwanted effects embody nausea, diarrhea, headache, and fatigue. These unwanted aspect effects are usually mild and infrequently resolve on their very own after a quantity of days. More severe side effects, similar to liver and pancreatic toxicity, have been reported in rare cases. Patients ought to monitor for any indicators of these unwanted side effects and search medical assist in the occasion that they happen.
While Lopinavir has been extensively used in the treatment of HIV, it has also shown promise in treating other viral infections. Research has advised that the medication could also be effective in opposition to SARS-CoV-2, the virus responsible for the COVID-19 pandemic. In vitro studies have shown that Lopinavir can inhibit the replication of SARS-CoV-2, and medical trials are at present underway to gauge its effectiveness in treating COVID-19.
Lopinavir works by inhibiting the protease enzyme, which is crucial for the manufacturing of new viral particles. By blocking this enzyme, the medication prevents the virus from replicating and spreading to different cells within the body. Ritonavir, then again, works by enhancing the effectiveness of Lopinavir. It does so by inhibiting the enzymes in the liver that break down Lopinavir, permitting it to remain within the physique longer and have a stronger effect.
In conclusion, Lopinavir, in combination with Ritonavir, has been a game-changer in the treatment of HIV/AIDS. Its potent antiviral properties have significantly improved the prognosis for folks residing with the virus and have also proven potential within the therapy of other viral infections like COVID-19. As with any medication, it's important to use Lopinavir as prescribed and beneath the supervision of a healthcare skilled to achieve the best outcomes and minimize the risk of side effects.
Kaletra is available in tablet kind and is usually taken twice a day with or without meals. It is important to take it at the identical time daily to make sure a constant level of the medication in the body. The dosage of Lopinavir and Ritonavir might vary depending on the individual’s weight and is usually adjusted by a healthcare professional to attain optimal outcomes. It is essential to observe the prescribed dosage and not miss any doses to avoid creating drug resistance.
Mirtazapine in progressive multifocal leukoencephalopathy associated with polycythemia vera medications ibs 250 mg lopinavir buy visa. The atypical antipsychotic agents ziprasidone [correction of zisprasidone], risperdone and olanzapine as treatment for and prophylaxis against progressive multifocal leukoencephalopathy. Chlorpromazine combined with cidofovir for treatment of a patient suffering from progressive multifocal leukoencephalopathy. Mirtazapine use in human immunodeficiency virus-infected patients with progressive multifocal leukoencephalopathy. Favourable outcome of progressive multifocal leucoencephalopathy in two patients with dermatomyositis. Mefloquine treatment in a patient suffering from progressive multifocal leukoencephalopathy after umbilical cord blood transplant. Successful management of natalizumab-associated progressive multifocal leukoencephalopathy and immune reconstitution syndrome in a patient with multiple sclerosis. Four methods of transmission are documented including direct inoculation of the conjunctiva, aerosolized droplets, fecaloral and exposure to infected tissue or blood. Asymptomatic infection, particularly of the respiratory tract, is common, but adenovirus is a common cause of febrile illnesses in young children associated with upper respiratory tract infections such as pharyngitis or coryza. Although most adenoviral illnesses are self-limiting, severe, and even fatal, infections can occur in immunocompromised hosts and occasionally in immunocompetent children and adults. In addition to their clinical importance, adenoviruses are now frequently employed as vectors for the delivery of foreign genes for gene therapy and for immunization against other pathogens. They are classified into six subgroups or species (formerly called subgenera), AF, on the basis of their physiochemical, biological and genetic properties (Table 10. Subgroups are further classified into more than 50 distinct adenoviruses (Ad) serotypes or subspecies based upon antigenic determinants detected by viral neutralization assay [5,6]. Although typing of adenoviruses into subgroups and serotypes is not routinely performed in most clinical laboratories, specific identification can be of clinical and epidemiological importance [10]. The fiber protein is attached noncovalently to the icosahedron by a pentameric polypeptide called the penton base. The fiber protein mediates attachment to cells and is probably an important determinant of tissue tropism. This 46 kDa plasma membrane protein is highly expressed 141 142 Adenovirus Table 10. Microbiol, 31, 15621569, 1993; Center for Disease Control, Neurotropic Viral Diseases Surveillance. Group-reactive antigenic determinants are present on the hexon proteins from all human adenoviruses. Type-specific neutralizing epitopes are present on both the fiber and hexon proteins, with minor sites on the penton base. In addition, many adenoviruses hemagglutinate rat or rhesus monkey red blood cells; this property is related to the fiber proteins and is used to classify adenoviruses into four hemagglutination groups (Table 10. Adenoviruses are highly stable in adverse physical conditions of pH and temperature and resist many chemical agents, including lipid solvents [1]. These properties account for their ability to spread and survive outside host cells. Adenoviruses (usually subgroups B, C, and E) are a common cause of febrile upper and lower respiratory tract illness in infants and young children year-round. Symptoms frequently associated with adenoviral infection include conjunctivitis, tonsillitis, laryngotracheobronchitis (croup) and pneumonia. Severe pneumonia has been associated with concurrent infection with measles and B. Disseminated adenoviral disease with multiorgan involvement has been described in association with these and other adenovirus serotypes in immunocompromised patients [16]. Adenoviruses have also been implicated in outbreaks of febrile respiratory disease in summer camps and swimming pools [18]. Adenovirus serotype 4 (the only member of subgroup E) has also been associated with outbreaks of conjunctivitis [4]. Enteric adenoviruses (subgroup A or subgroup F types 40 and 41) can cause outbreaks of diarrheal illness in infants, typically in group care settings such as daycare centers. These have been described more frequently in young children and in immunocompromised hosts, often in association with multiorgan involvement, particularly pneumonia and hepatitis and during disseminated adenoviral disease. The characteristic cytopathic changes produced by this agent were also described by Hilleman and Werner in 1954 [27] when they cultured throat washings of military recruits with febrile acute respiratory illness. Adenovirus was then identified as the cause of acute respiratory disease in military recruits [28], and shortly thereafter the association between adenovirus and epidemic keratoconjunctivitis and pharyngoconjunctival fever were recognized. In fact, these epidemic syndromes caused by adenovirus had been described in Europe, Asia, and the United States since the nineteenth century and throughout the first half of the twentieth century [1,28]. Because adenovirus was an important cause of acute respiratory disease in military recruits, intensive research was carried out that resulted in the identification and classification of dozens of adenovirus types and in the development of vaccines against adenovirus types 4 and 7 to control epidemics in the military [29,30]. A suspension in the production of these vaccines in 1994 resulted in the reemergence of adenovirus epidemics in military trainees [31]. Enteric adenoviruses (types 40 and 41), first reported in 1975, were initially found by electron microscopy and subsequently shown to be a cause of diarrheal illness in children [32]. Among them, adenovirus type 7 was isolated from the brain tissue of a child who developed fatal encephalitis. Some children had concomitant or recent viral infections such as varicella [37,38]. Although isolation of adenovirus from brain tissue or spinal fluid was not always performed, adenovirus infection was documented in patients who developed neurological manifestations without other identified etiology [23,3941]. Eight cases of meningoencephalitis in children and infants were reported in association with an adenovirus type 7 epidemic in northern Finland in 1970 [42].
Vestibular neuritis is primarily treated with rest medicine 2015 lyrics 250 mg lopinavir order with amex, vestibular suppressant medications, and vestibular rehabilitation. Patients may initially be admitted if symptoms, such as nausea and vomiting, are severe or if stroke is suspected. Treatment with antihistamines (dimenhydrinate [Dramamine]1 50 mg every 6 hours), antiemetics (promethazine [Phenergan]1 25 mg every 6 hours), or benzodiazepines (lorazepam [Ativan]1 1 to 2 mg every 4 hours) may be used to treat severe symptoms. However, these should not be continued for more than 2 to 3 days because they inhibit central compensation. Using vestibular suppressants blocks central compensation and lengthens the course of the disease. Although studies show that vestibular-function testing improves more quickly in patients treated with corticosteroids, there is conflicting evidence that corticosteroids hasten the recovery of clinical signs and symptoms of vestibular neuritis. A 2011 Cochrane review concluded that there is insufficient evidence to recommend corticosteroids for the treatment of vestibular neuritis. Finally, antiviral medications have not been proven effective for vestibular neuritis. For patients with vestibular neuritis, vestibular rehabilitation should be started as soon as symptoms improve and a patient can tolerate the exercises. Exercises include balance and gait training as well as coordination of head and eye movements. Vestibular rehabilitation hastens recovery and improves balance, gait, and vision by increasing central compensation for vestibular dysfunction. Exercises may be home-based for compliant patients with mild symptoms, whereas formal referral may be more beneficial for patients with severe symptoms, or for the elderly. Failure to improve warrants further evaluation for other etiologies, including central causes. Similarly, patients with vestibular neuritis should slowly improve over several weeks, and failure to do so suggests alternative diagnoses. Patients should be warned that nausea or vomiting may occur during the procedure, and may be pretreated with an antiemetic medication. The procedure can be repeated immediately if unsuccessful, and the majority of patients will respond after three attempts. Observation is an option if symptoms are mild or if a patient will not tolerate the canalith repositioning procedure or vestibular rehabilitation. Counseling patients about recurrence can lead to earlier recognition, earlier treatment, and avoidance of falls. Chan Y: Differential diagnosis of dizziness, Otolaryngol Head Neck Surg 17:200203, 2009. A mental status examination and screening for depression and anxiety should follow. The challenge with the diagnostic workup for fatigue is that most laboratory tests do not yield a significant diagnosis. Repeated studies show that only about 15% of patients in primary care settings will have an organic cause for their fatigue (Harrison, Ponka), and laboratory results affect management in as little as 5% of patients (Rosenthal). The following recommendations for the laboratory investigation of fatigue are adapted from guidelines developed by Dutch, Canadian, and Australian general practice groups (Harrison): · Consider monitoring for a month after initial presentation, while initiating conservative management. Depression, environmental factors such as lifestyle, anxiety, and anemia are among the most common causes of fatigue. Diabetes and other endocrine disorders, including thyroid disease, should be considered, as well as an undiscovered tumor. Many infections, especially those of viral origin, cause fatigue, as well as insomnia and sleep disorders such as obstructive sleep apnea. Rheumatologic disorders, such as rheumatoid arthritis, systemic lupus erythematosus, and fibromyalgia, are often accompanied by fatigue. Endocarditis, while rare, is a must-notmiss diagnosis, as are other cardiac conditions such as coronary artery disease. Finally, drugs, either prescription or of personal use or abuse, should be considered. Chronic fatigue syndrome is a specific clinical diagnosis characterized by unexplained persistent or relapsing fatigue, not relieved by rest, that substantially limits daily activity. In addition, there must be at least four of the following: memory or concentration impairment, sore throat, tender cervical or axillary lymph nodes, muscle pain, multijoint pain without swelling or tenderness, new headaches, unrefreshing sleep, or postexertional malaise lasting more than 24 hours. Epidemiology Fatigue or tiredness is a common complaint in the general population, representing the chief complaint in nearly 10% of patients presenting to a primary care physician and reported as a symptom in 21% of all patient encounters. While acute, prolonged, and chronic fatigue are relatively common, chronic fatigue syndrome is relatively rare. I 12 Risk Factors Risk factors for fatigue in adolescence include having depressive symptoms, being highly sedentary, and, conversely, being highly physically active. In adults, risk factors include age over 65 years, presence of one or more chronic medical conditions, and female gender. Precipitating factors include physical stresses such as infectious mononucleosis and psychological stresses such as jobrelated problems. Perpetuating factors include physical inactivity, emotional disorders, and disturbances of sleep. Treatment Prevention Because physical inactivity, psychological stress, and lack of sleep are predisposing and perpetuating factors for fatigue, it is helpful to advise patients about stress reduction, regular exercise, and proper sleep habits. Clinical Manifestations Fatigue is characterized by general malaise, vague physical discomfort, and an inability to perform routine activities. Acute fatigue is short-lived and generally attributable to physical exertion or an acute illness. Prolonged fatigue is defined as self-reported, persistent fatigue lasting 1 month or longer, whereas chronic fatigue is defined as similar symptoms lasting 6 months or more.
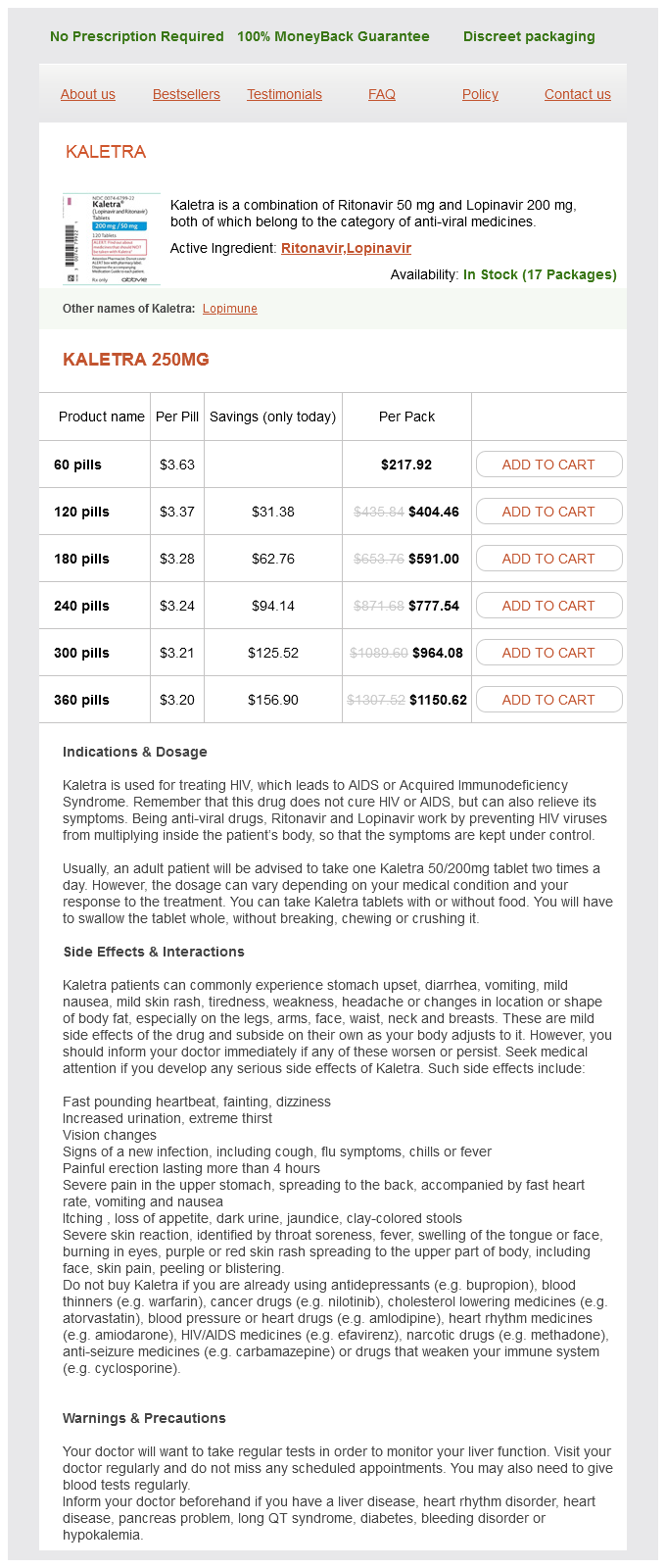
Lopinavir Dosage and Price
Kaletra 250mg
- 60 pills - $217.92
- 120 pills - $404.46
- 180 pills - $591.00
- 240 pills - $777.54
- 300 pills - $964.08
- 360 pills - $1150.62
Computed tomographic angiography is widely available treatment for gout lopinavir 250 mg buy line, requires relatively short scanning time, has low operator dependency, and provides high-resolution images that can be processed for threedimensional reconstruction. Spinal stenosis can lead to leg discomfort (pseudoclaudication) that may be confused with claudication. Pseudoclaudication is usually a paresthetic discomfort that occurs with standing and walking, usually bilateral and relieved by sitting or leaning forward. Often there is a history of chronic back pain or previous lumbosacral spinal surgery. Giant cell arteritis can involve peripheral arteries, and symptoms of peripheral artery involvement may dominate the clinical picture. Therapy is directed mainly at the underlying disease, and only after the inflammatory process is controlled should revascularization of chronically ischemic extremities be contemplated. Thromboangiitis obliterans (Buerger disease) is a segmental inflammatory disease involving the small and medium vessels of the arms and legs. The Shionoya diagnostic criteria for thromboangiitis obliterans include history of smoking, onset before age 50, infrapopliteal arterial occlusive disease, upper extremity involvement or phlebitis migrans, and absence of atherosclerotic risk factors other than heavy smoking. Angiography usually shows multiple, bilateral focal segments of stenosis or occlusion with normal proximal vessels. Treatment includes avoidance of all forms of tobacco to reduce the risk of ulcer formation and amputation. Symptoms of claudication may improve with aspirin, clopidogrel (Plavix),1 pentoxifylline (Trental),1 and cilostazol (Pletal). Repeated compression of the popliteal artery can lead to localized atherosclerosis, poststenotic dilatation, or thrombosis, resulting in ischemia in the distal leg or foot. In a large registry study, statin use was associated with an $18% lower rate of adverse limb outcomes (including worsening of symptoms, peripheral revascularization, and amputation). Treatment of diabetes does not reduce cardiovascular events but may lower risks of microvascular disease and neuropathy. Since intensive blood glucose control may increase mortality in patients with established cardiovascular disease, a target A1C should be chosen based on age, duration of diabetes, and presence of comorbid conditions. Referral for counseling and/or use of adjunctive pharmacotherapy (varenicline [Chantix], bupropion [Zyban], or nicotine replacement therapy) may increase abstinence rates. Warfarin (Coumadin)1 is not recommended, as the combination of warfarin and aspirin did not result in greater reduction in cardiovascular events than aspirin alone and was associated with more bleeding. The degree of functional limitation varies depending on the degree of arterial stenosis, collateral circulation, exercise capacity, and comorbid conditions. A program that incorporates walking at least three times per week (3060 minutes/session) for at least 12 weeks should be the first-line therapy for claudication. A home-based group-mediated cognitive-behavioral walking intervention that included goal setting, self-monitoring, managing pain during exercise, and walking at least 5 days per week improved 6-minute walking distance by 53 m compared to a control group that received health education alone. Pharmacotherapy is only modestly effective for improving symptoms of claudication. Cilostazol (Pletal), a phosphodiesterase inhibitor with antiplatelet and vasodilatory properties, improves maximal treadmill walking distance by $25%. The dose is 100 mg orally daily (50 mg orally twice daily in patients taking diltiazem [Cardizem], ketoconazole [Nizoral], or other inhibitors of cytochrome P450 3A4). Naftidrofuryl, a 5 hydroxy-tryptamine receptor blocker2 that inhibits platelet aggregation, may be more effective than cilostazol 2 and is approved in Europe for claudication. Atorvastatin (Lipitor)1 (80 mg daily for 12 months) modestly improved pain-free walking time, but not maximal walking time, compared to placebo. Revascularization is indicated when there are limiting symptoms in spite of an exercise program and medical therapy, and there is a reasonable likelihood of symptomatic improvement (including absence of other conditions that might limit functional capacity such as heart failure or lung disease), as well as limb salvage in the setting of critical limb ischemia. The revascularization strategy for each patient should be individualized based on patient preferences, anatomic factors, availability of optimal conduits, and operative risk. Aortoiliac angioplasty and stenting have high procedural success rates ($96%) and a 3-year patency rate of $82%. Stent placement is generally avoided in the common femoral artery owing to the risk of biomechanical stress-related stent fractures and the potential for interference with future arterial access. Endovascular intervention in the superficial femoral artery is associated with high rates of restenosis, and several technologies to limit restenosis including drug-eluting or covered stents, drug-coated balloons, and brachytherapy are being evaluated. Endovascular therapy of isolated infrapopliteal disease is not recommended for claudication. Patients should receive dual antiplatelet therapy for at least 30 days, and longer if a drug-eluting stent is placed. Aortofemoral bypass is a durable operation for aortoiliac disease, with patency rates up to 90% at 5 years. In patients who are poor surgical candidates, cross-clamping of 1 Not available in the United States. Anatomy Common iliac artery Internal iliac artery Common femoral artery Balloon expandable stent Endovascular Balloon angioplasty Covered Drug coated Drug coated stent balloon stent 144 Restenosis External iliac Self artery expanding stent Profunda femoris Atherectomy artery Endarterectomy Groin crease Superficial femoral artery Knee crease Tibialperoneal artery Peroneal artery Posterior tibial artery Popliteal artery Anterior tibial artery Axillofemoral; Femoralfemoral Bypass Types Aortofemoral Femoralpopliteal Femoraldistal the aorta can be avoided by an axillaryfemoral graft often combined with a femoralfemoral graft. The saphenous vein is the preferred conduit for infrainguinal bypass, but a prosthetic conduit can be used for femoralpopliteal bypass if the above-knee popliteal artery is the target vessel and good runoff is present. There is no clear guidance on antithrombotic therapy after surgical revascularization; however, in patients undergoing infrainguinal bypass surgery, venous grafts had better patency with warfarin1 than aspirin therapy, whereas prosthetic grafts had better patency on aspirin. Patients who have undergone revascularization should be monitored for stent/graft patency. The incidence of adverse limb outcomes including worsening of symptoms, peripheral revascularization, and amputation was 26% over 4 years, based on registry data.