Macrobid
General Information about Macrobid
Macrobid, also referred to as nitrofurantoin, is an antimicrobial agent from the nitrofurans group that has been in use for over 60 years. It is specifically designed for the remedy of urinary tract infections (UTIs) and has been confirmed to be extremely effective on this regard. Moreover, it is also used for the prevention of infections after urologic surgical procedure or procedures corresponding to cystoscopy and catheterization.
In addition to treating UTIs, Macrobid is also used for the prevention of infections after urologic procedures similar to cystoscopy and catheterization. These procedures contain the insertion of medical devices into the urinary tract, which might introduce bacteria and improve the danger of an infection. By utilizing Macrobid as a safety measure, the danger of an infection could be significantly decreased.
While Macrobid is usually well-tolerated, like all medicine, it might have some unwanted effects. Commonly reported unwanted aspect effects embrace nausea, vomiting, and headache. In rare circumstances, it could cause allergic reactions or more extreme side effects such as lung or liver harm. It is important to inform a healthcare supplier of any allergy symptoms or medical situations before starting Macrobid treatment.
Macrobid is out there in both oral and intravenous varieties, with the oral form being the popular choice for treating UTIs. The really helpful dosage and length of remedy might differ relying on the severity of the infection and the affected person's medical historical past. It is important to follow the prescribed remedy plan and complete the total course of treatment as really helpful by the healthcare provider to ensure the complete eradication of the infection.
Urinary tract infections are some of the widespread bacterial infections worldwide, affecting each women and men of all ages. The main reason for UTIs is bacteria, and the commonest wrongdoer is Escherichia coli (E. coli). These infections can vary from gentle to severe, with signs like burning sensation throughout urination, frequent urination, and stomach pain. If left untreated, UTIs can result in critical issues such as kidney damage and sepsis, especially in susceptible populations like the aged and people with weakened immune systems.
In conclusion, Macrobid is a vital and highly effective antimicrobial agent in the treatment of UTIs. Its dual mechanism of action and skill to pay attention within the urinary tract make it an appropriate alternative for these affected by this common an infection. Moreover, its use in stopping infections after urologic procedures has additionally proven to be helpful. It is important to use this treatment judiciously to ensure its efficacy and forestall the event of antibiotic resistance.
One of the main advantages of Macrobid is its ability to pay attention in the urinary tract and remain energetic for an extended time frame. This makes it perfect for the remedy of UTIs, as it can effectively eliminate the micro organism causing the an infection. Furthermore, it also has a low threat of growing resistance, making it a dependable remedy possibility for recurrent UTIs.
This is the place Macrobid comes into the image as a highly effective treatment choice for UTIs. It works by disrupting the permeability of the bacterial cell membrane and inhibiting the manufacturing of proteins wanted for bacterial development and replication. This dual mechanism of action makes it highly effective in treating UTIs brought on by a variety of bacteria. In addition, Macrobid is also effective towards some strains of antibiotic-resistant bacteria, making it an important device within the battle towards antimicrobial resistance.
Brain stem auditory evoked responses can be recorded from scalp electrodes at 0 to 10 msec (early) gastritis diet oatmeal cookies buy 100 mg macrobid otc, 10 to 50 msec (middle), and 50 to 500 msec (late) following a click (a high-frequency stimulus). The early potentials reflect electrical activity at the cochlea, eighth cranial nerve, and brain stem; the later potentials reflect cortical activity. Computer averaging of the responses to 1000 to 2000 clicks separates the evoked potential from background noise. Early evoked responses may be used to estimate the magnitude of hearing loss and to differentiate among cochlea, eighth nerve, and brain stem lesions. It is typically characterized by an approximately equal loss of hearing at all frequencies and by well-preserved speech discrimination once the threshold for hearing is exceeded. Patients with conductive hearing loss can hear speech in a noisy background better than in a quiet background because they can understand loud speech as well as anyone. Sensorineural hearing loss results from lesions of the cochlea or auditory division of the eighth cranial nerve, or both. With sensorineural hearing loss, the hearing levels for different frequencies are usually unequal, typically resulting in better hearing for low- than for high-frequency tones. Patients with sensorineural hearing loss often have difficulty in hearing speech that is mixed with background noise and may be annoyed by loud speech. Three important manifestations of sensorineural lesions are diplacusis, recruitment, and tone decay. Diplacusis and recruitment are common with cochlear lesions; tone decay usually accompanies eighth nerve involvement. As a rule, patients with central lesions do not have impaired hearing for pure tones, and they can understand speech as long as it is clearly spoken in a quiet environment. The most common cause of conductive hearing loss is impacted cerumen in the external canal. This benign condition is usually first noticed after bathing or swimming when a droplet of water closes the remaining tiny passageway. Fluid accumulates in the middle ear, impairing the conduction of airborne sound to the cochlea. Because the air cavity of the middle ear is in direct connection with the mastoid air cells, infection can spread through the mastoid bone and, occasionally, into the intracranial cavity. Chronic otitis media with perforation of the tympanic membrane can result in an invasion of the middle ear and other pneumatized areas of the temporal bone by keratinizing squamous epithelium (cholesteatoma). Cholesteatomas can produce erosion of the ossicles and bony labyrinth, resulting in a mixed conductive and sensorineural hearing loss. Otosclerosis commonly produces progressive conductive hearing loss by immobilizing the stapes with new bone growth in front of and below the oval window. The hearing loss is typically conductive, although in some persons the cochlea may be invaded by foci of otosclerotic bone, producing an additional sensorineural hearing loss. Otosclerosis usually stabilizes when the hearing level reaches 50 to 60 dB and rarely progresses to deafness. Other common causes of conductive hearing loss include trauma, congenital malformations of the external and middle ear, and glomus body tumors. DifferentialDiagnosis Conductive Hearing Loss Sensorineural Hearing Loss Hereditary Deafness A quick test for hearing loss in the speech range is to observe the response to spoken commands at different intensities (whisper, conversation, shouting). In the Rinne test, nerve conduction is compared with bone conduction by holding a tuning fork (preferably 512 Hz) against the mastoid process until the sound can no longer be heard. It is then placed 1 inch from the ear and, in normal subjects, can be heard about twice as long Genetically determined deafness, usually from hair cell aplasia or deterioration, may be present at birth or may develop in adulthood. The diagnosis of hereditary deafness rests on the finding of a positive family history. Mutations in connexin 26, a key component of gap junctions in the inner ear, account for most cases of recessively inherited deafness. Intrauterine factors resulting in congenital hearing loss include infection (especially rubella); toxic, metabolic, and endocrine disorders; and anoxia associated with Rh incompatibility and difficult deliveries. Bacterial or viral infections of the labyrinth, head trauma with fracture or hemorrhage into the cochlea, or vascular occlusion of a terminal branch of the anterior inferior cerebellar artery can extensively damage the cochlea and the vestibular labyrinth. An isolated sudden unilateral sensorineural hearing loss is presumed to reflect a viral infection of the cochlea and auditory nerve terminals. Sudden unilateral hearing loss often associated with vertigo and tinnitus can result from a perilymphatic fistula. Drugs Cochlear Damage among those with exposure to loud explosive or industrial noises. The loss almost always begins at 4000 Hz and does not affect speech discrimination until late in the disease process. With only brief exposure to loud noise (hours to days), there may be only a temporary threshold shift, but with continued exposure, permanent injury begins. Salicylates, furosemide, and ethacrynic acid have the potential to produce transient deafness when they are taken in high doses. More toxic to the cochlea are aminoglycoside antibiotics (gentamicin, tobramycin, amikacin, kanamycin, streptomycin, and neomycin). These agents can destroy cochlear hair cells in direct relation to their serum concentrations. Some antineoplastic chemotherapeutic agents, particularly cisplatin, cause severe ototoxicity. Meniere Disease Progressive unilateral hearing loss, which arises insidiously, initially in the high frequencies, and worsens by almost imperceptible degrees, is characteristic of benign neoplasms of the cerebellopontine angle, most commonly acoustic neuromas. In about 10% of cases, the hearing loss can be acute, apparently due to either hemorrhage into the tumor or compression of the labyrinthine vasculature. Central Hearing Loss Subacute relapsing cochlear deafness occurs with Meniere disease, a condition associated with fluctuating hearing loss and tinnitus, recurrent episodes of abrupt and often severe vertigo, and a sensation of fullness or pressure in the ear.
On clinical examination gastritis diet ÷ĺëîâĺę cheap macrobid 100 mg on-line, inspection should assess evidence of trauma, muscle wasting, fasciculations, erythema, rashes, and scars. Palpation is directed to areas of point tenderness during evaluation for more diffusely tender regions, muscle spasm, and masses. If light percussion of the spinous process evokes significant pain, a focal process, such as fracture, malignant neoplasm (Chapter 189), or infection (Chapter 413), should be considered because such a finding is unusual in typical mechanical spine pain. Finally, the active and passive range of motion for flexion, extension, rotation, and tilt should be noted. Many provocative tests have been described for the evaluation of neck and back pain, but few have undergone formal evaluation of their diagnostic accuracy. Downward pressure on the top of the head by the examiner will reproduce arm dysesthesias (Video 400-2). No evidence of intoxication-Patients should be considered intoxicated if they have either of the following: a recent history provided by the patient, or an observer of intoxication or intoxicating ingestion, or evidence of intoxication on physical examination such as an odor of alcohol, slurred speech, ataxia, dysmetria, or other cerebellar findings, or any behavior consistent with intoxication. Patients may also be considered to be intoxicated if tests of bodily secretions are positive for alcohol or drugs that affect level of alertness. A normal level of alertness-An altered level of alertness can include the following: a Glasgow Coma Scale score of 14 or less; disorientation to person, place, time, or events; an inability to remember three objects at five minutes; a delayed or inappropriate response to external stimuli; or other findings. No focal neurological deficit-A focal neurological deficit is any focal neurological finding on motor or sensory examination. No painful distracting injuries-No precise definition of painful distracting injury is possible. This category includes any condition thought by the clinician to be producing pain sufficient to distract the patient from a second (neck) injury. Such injuries may include, but are not limited to , any long-bone fracture; a visceral injury requiring surgical consultation; a large laceration, degloving injury, or crush injury; large burns; or any other injury causing acute functional impairment. Validityofasetof clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. Self-assessment of interference with daily activities Physical exam: Neurological and other Triage: What kind of neck pain Clinical practice implications of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. For back and neck pain that persists for 6 weeks, electrodiagnostic testing can demonstrate compromise of spinal root function but is not usually helpful in axial spine pain without neurologic symptoms. Acute mechanical neck pain is most often caused by a neck strain, a herniated nucleus pulposus, or whiplash; for pain of insidious onset, osteoarthritis and myelopathy are the leading causes. For back pain, muscle strain and a herniated nucleus pulposus are acute causes; insidious causes include osteoarthritis, spinal stenosis, spondylolisthesis, and scoliosis. Abdominal aortic aneurysms (Chapter 78) can present with a mid- to low back ache that may radiate to the hips or anterior thighs. Genitourinary disorders (Chapter 123) can cause colicky referred pain to the flanks and costovertebral angle. Bladder disorders (Chapter 123) may occasionally refer pain to the sacral area, as can prostate problems (Chapter 129). Pelvic disorders in women that can cause referred low back pain include endometriosis (Chapter 236), ectopic pregnancy, and pelvic inflammatory disease (Chapters 299 and 318). Most of these disorders have additional signs and symptoms to aid in the diagnosis. Myocardial ischemia (Chapters 71 to 73) can be associated with anterior neck pain, although less commonly than with left arm or jaw pain. Arterial dissections (Chapter 78) are more commonly associated with neck pain; for example, up to 20% of patients with carotid dissections complain of anterolateral pain, and about 80% of patients with vertebral dissections have posterior or occipital pain. Patients with arterial dissections frequently but not necessarily have signs and symptoms of stroke (Chapter 407). Disorders of the esophagus (Chapter 138) and mass lesions of the throat (Chapters 190 and 429) can also present as neck pain. Acute spine pain can precede the rash in herpes zoster (Chapter 375) or can be seen in the vaso-occlusive crisis of sickle cell anemia (Chapter 163). Arachnoiditis (Chapter 412), an inflammatory process of the arachnoid space, can cause diffuse chronic back pain, often after the introduction of foreign substances or manipulation of the intrathecal space. Finally, 20 to 50% of patients with depression (Chapter 397) will complain of back pain that often is diffuse and described in emotionally laden terms. For chronic neck pain, yoga therapy yields significant pain relief with the possible added benefits of improving quality of life and psychological well-being. In one randomized trial, tanezumab (10 to 20mg intravenously, repeated 8 weeks later), a humanized monoclonal antibody that specifically inhibits nerve growth factor, reduced pain better than naproxenorplacebo. Inmorefocaldisor- Between 50 and 85% of patients who have neck pain that persists for more than 1 day report recurrence of symptoms in 1- and 5-year follow-up. Slightly more than 50% of patients recover within 3 months, and those who remain symptomatic generally have relatively little pain and disability. Prior neck injury or pain, coexistent low back pain, and selfperceived poor general health are risk factors for symptoms persisting past 3 months or recurrence. Mechanical spine pain, even with radicular symptoms, resolves without specific intervention within 30 days in many patients and within 3 months in 90% of patients. Recurrence is frequent, however, especially in patients with spondylosis, because the underlying process persists and further degeneration of the spinal elements can be expected.
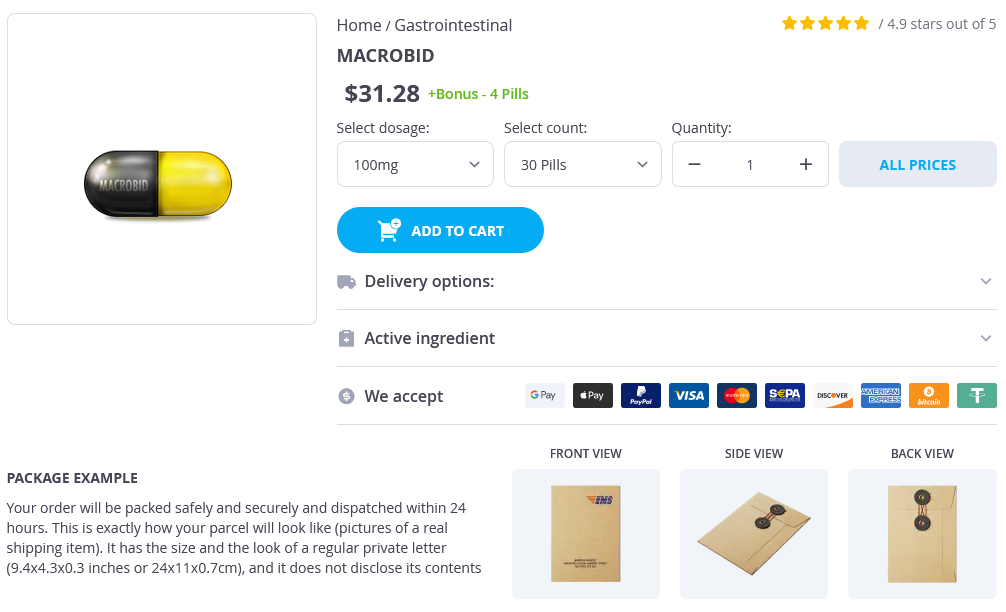
Macrobid Dosage and Price
Macrobid 100mg
- 30 pills - $34.76
- 60 pills - $58.49
- 90 pills - $80.29
- 120 pills - $80.19
- 180 pills - $125.19
- 360 pills - $214.49
Macrobid 50mg
- 120 pills - $118.99
- 180 pills - $157.99
- 360 pills - $305.99
Stem cells migrate and seed into white and grey matter to form a pool of adult progenitor cells gastritis foods macrobid 100mg with amex, which can later differentiate to replenish defunct oligodendrocytes, and possibly remyelinate axons in pathologically demyelinated regions. A sheath of astrocytic end-feet wraps around the vessel and, in vessels larger than capillaries, its investment of pial meninges. Vascular endothelial cells are joined by tight junctions and supported by pericytes; perivascular macrophages lie outside the endothelial basal lamina (light blue). BloodÂbrain barrier Proteins circulating in the blood enter most tissues of the body except those of the brain, spinal cord and peripheral nerves. This concept of a bloodÂbrain or a bloodÂnerve barrier applies to many substances  some are actively transported across the bloodÂbrain barrier, others are actively excluded. The bloodÂbrain barrier is located at the capillary endothelium within the brain and is dependent on the presence of tight junctions (occluding junctions, zonulae adherentes) between endothelial cells coupled with a relative lack of transcytotic vesicular transport. The bloodÂbrain barrier develops during embryonic life but may not be fully completed by birth. The pale-staining axon (A) is ensheathed by oligodendrocyte myelin (arrow), apart from a short, exposed region at the node. Nodal axolemma is contacted by fine filopodia of perinodal cells, which have been shown in animal studies to have a presumptive adult oligodendrocyte progenitor phenotype; their function is unknown. SchmidtÂLanterman incisures are helical decompactions of internodal myelin where the major dense line of the myelin sheath splits to enclose a spiral of oligodendrocyte cytoplasm. Their structure suggests that they may play a role in the transport of molecules across the myelin sheath, but their function is not known. The oligodendrocyte soma is shown in the centre and its myelin sheaths are unfolded to varying degrees to show their extensive surface area. A single oligodendrocyte may ensheathe up to 50 separate axon segments, depending on calibre, whereas myelinating Schwann cells ensheathe axons on a 1: 1 basis. There is considerable overlap between the size of the smallest myelinated and the largest unmyelinated axons, and so axonal calibre is unlikely to be the only factor in determining myelination. Moreover, the first axons to become ensheathed ultimately attain larger diameters than those that are ensheathed at a later date. There is a reasonable linear relationship between axon diameter and internodal length and myelin sheath thickness: as the sheath thickens from a few lamellae to up to 200, the axon may also grow from 1 to 15 µm in diameter. The ultrastructural appearance of myelin is usually explained in terms of the spiral wrapping of an extensive, flat glial process (lamellipodium) around an axon, and the subsequent extrusion of cytoplasm from the sheath at all points other than incisures and paranodes. These lines, first described in early electron microscope studies of the myelin sheath, correspond to the intraperiod and period lines respectively, defined in X-ray studies of myelin. B, A confocal micrograph of a mature myelin-forming oligodendrocyte in an adult rat optic nerve, iontophoretically filled with an immunofluorescent dye by intracellular microinjection. Schwann cell cytoplasm Basal lamina Inner mesaxon Outer mesaxon Axon the inner and outer mesaxons. There are significant differences between central and peripheral myelin, reflecting the fact that oligodendrocytes and Schwann cells express different proteins during myelinogenesis. Myelin membrane contains protein, lipid and water, which forms at least 20% of the wet weight. The major lipid species are cholesterol (the most common single molecule), phospholipids and glycosphingolipids. Minor lipid species include galactosylglycerides, phosphoinositides and gangliosides. The major glycolipids are galactocerebroside and its sulphate ester, sulphatide; these lipids are not unique to myelin but they are present in characteristically high concentrations. Gangliosides, which are glycosphingolipids characterized by the presence of sialic acid (N-acetylneuraminic acid), account for less than 1% of the lipid in myelin. A relatively small number of protein species account for the majority of myelin protein. Myelination does not occur simultaneously in all parts of the body in late fetal and early postnatal development. White matter tracts and nerves in the periphery have their own specific temporal patterns that relate to their degree of functional maturity. Mutations of the major myelin structural proteins have now been recognized in a number of inherited human neurological diseases. As would be expected, these mutations produce defects in myelination and in the stability of nodal and paranodal architecture that are consistent with the suggested functional roles of the relevant proteins in maintaining the integrity of the myelin sheath. They form a single-layered epithelium that varies from squamous to columnar in form. At the ventricular surface, cells are joined by gap junctions and occasional desmosomes. There is considerable regional variation in the 52 ependymal lining of the ventricles but four major types have been described. These are: general ependymal, which overlies grey matter; general ependymal, which overlies white matter; specialized areas of ependyma in the third and fourth ventricles; and choroidal epithelium. Each cell bears approximately 20 central apical cilia, surrounded by short microvilli. Beneath them there may be a subependymal (or subventricular) zone, from two to three cells deep, consisting of cells that generally resemble ependymal cells. In rodents, the subventricular zone contains neural progenitor cells, which can give rise to new neurones, but the existence of these stem cells in the adult human brain is controversial (Sanai et al 2011, Kempermann 2011). Where the ependyma overlies myelinated tracts of white matter, the cells are much flatter and few are ciliated. There are gap junctions and desmosomes between these cells, but their lateral margins interdigitate, unlike their counterparts overlying grey matter. Specialized areas of ependymal cells called the circumventricular organs are found in four areas around the margins of the third ventricle: namely, the lining of the median eminence of the hypothalamus; the subcommissural organ; the subfornical organ; and the vascular organ of the lamina terminalis.