Maxalt
General Information about Maxalt
Migraines are more than simply complications. They are debilitating, throbbing pains that may last for hours, if not days. For over 39 million individuals within the United States, migraines are a frequent reality, affecting their day by day lives and productiveness. However, due to developments in medicine, there are now efficient therapies obtainable to assist handle and alleviate the symptoms of migraines. One such treatment is Maxalt.
Another benefit of Maxalt is its ease of use. The orally disintegrating tablets, which dissolve rapidly in the mouth, are particularly useful for these who may battle to swallow pills throughout a migraine attack. This makes it a handy and accessible possibility for anybody experiencing a migraine.
In conclusion, Maxalt has been a game-changer for migraine sufferers. Its fast-acting formula, ease of use, and effectiveness in treating extreme migraines have made it a preferred choice for many. However, it's always important to seek the advice of a well being care provider before taking any treatment, even for migraine remedy. With proper medical steering, Maxalt can go a good distance in serving to people handle and relieve the symptoms of migraines, allowing them to reside their lives to the fullest.
Available in each tablet and orally disintegrating pill form, Maxalt is taken as quickly as the migraine begins to take impact. It works by constricting the blood vessels in the brain to minimize back the discharge of drugs that may cause inflammation and pain. This helps to alleviate not only the ache but in addition other symptoms of migraines, such as nausea and sensitivity to gentle and sound.
Maxalt is a drugs used to treat migraines that have already began. It belongs to a category of drugs generally recognized as triptans, which work by narrowing the blood vessels in the brain and reducing irritation. This helps to alleviate the intense and pulsating ache associated with migraines.
Before taking Maxalt, it is essential to consult a physician first, especially in case you have a history of coronary heart issues, hypertension, or some other underlying medical situations. It just isn't beneficial for pregnant or breastfeeding women, as properly as individuals under the age of 18.
One of the important thing advantages of Maxalt is its fast-acting method. Unlike some other migraine drugs, Maxalt starts to work inside 30 minutes. This is crucial for migraine sufferers as early intervention can help cut back the severity and length of the attack. Additionally, Maxalt is efficient even for extreme migraines and can be used up to 4 instances a day, with a minimum of two hours between doses.
Like any medicine, Maxalt additionally has its potential side effects. The most typical ones embody dizziness, drowsiness, and dry mouth. It is important to notice that these side effects are often mild and resolve on their own. However, in the event that they persist or become extreme, it is essential to seek the advice of a well being care provider.
High salt increased urinary cystine Limitation of substrate for All patients: limited compliance cystine production Reduction of cystine excretion Increased urinary cystine solubility Thiol-disulphide exchange with cysteine All cystinuric patients (> 250 mg/day) Severely cystinuric patients (> 500 mg/ day) or moderate cystinuric patients (250500 mg/day) when fluid and alkali treatment are ineffective Severely cystinuric patients (> 500 mg/ day) or moderate cystinuric patients (250500 mg/day) when fluid and alkali treatment are ineffective Unproven effectiveness Patient intolerant of first- and second-generation chelating agents Controversial: it is useful with high sodium intake First-generation chelating agents (D-penicillamine) Second-generation chelating agents (tiopronin) Thiol-disulphide exchange with cysteine Captopril Ascorbic acid Thiol-disulphide exchange with cysteine Converts cystine to cysteine Reduces cystine excretion via renal tubular competitive inhibition dose for adults is 1520 mEq twice a day kneecap pain treatment order maxalt 10 mg fast delivery. Chelating agents Chelating agents such as D-penicillamine (di-methyl cysteine) and -mercaptopropionylglycine must be used in subjects who are non-responsive to urinary alkalization and in those with severe cystinuria (> 500 mg/day). Both of these agents are thiol derivatives which cleave a single cystine molecule into two cysteine molecules to make a soluble disulphide compound consisting of the respective drug and cysteine molecules and lowers the excretion of sparingly soluble cystine (Crawhall et al. D-penicillamine (Cuprimin, Depen) was the first chelating agent found to lower urinary cystine (Crawhall et al. D-penicillamine bears the risk of dermatological (pemiphigus), haematologic (agranulocytosis, thrombocytopenia), renal (nephrotic syndrome), and rheumatological (polymyositis) complications (Halperin et al. The dosage must be adjusted to reduce the urinary cystine concentration below its solubility limit of < 250 mg/L (1 mmol/L). Generally, the appropriate dosage in adults is approximately 1000mg/day, which reduces the urinary cystine excretion by 360 mg/day (Pak et al. In children, the recommended dose is 2040 mg/kg body weight/day (Fjellstedt et al. Since cystine excretion is higher at night, it is also preferred that one dose is administered at bedtime (Fjellstedt et al. One may initially use the lowest dose of drug with a gradual, incremental increase over a 4-week period until the optimal tolerated dosage is attained. Both drugs are equally effective in reducing kidney stone incidence when compared with conservative management, tiopronin is preferred because of lower incidences of side effects (Linari et al. With oral dosing, one-quarter of the administered dose appeared unchanged in the urine. Mediated by a thiol-disulphide exchange mechanism, this participates in the interaction with cystine which leads to lowered urinary cystine excretion (Pak et al. Tiopronin is effective in causing stone remission and reducing the individual stone formation rates in patients with and without prior D-penicillamine treatment (Pak et al, 1986a). In patients with stone relapse on D-penicillamine, tiopronin was shown to significantly decreased new stone formation by 71% and 61. Side effects including skin reactions, oral ulcers, gastrointestinal intolerance, and nephrotic syndrome (Tasic et al. One study in a total of 27 adult patients with cystine stones reported a significant decrease in stone episodes and urological procedures when thiol drugs (D-penicillamine and tiopronin) were added to conservative management (Barbey et al. This finding suggests a 65% decrease in yearly stone event rate during thiol treatment compared to conservative management. Captopril is an angiotensin-converting enzyme inhibitor which possesses a thiol component which has been suggested to form a thiol-cysteine mixed disulphide and reduce urinary cystine excretion (Sloand and Izzo, 1987). In one report, 75100 mg/day of captopril reduced urinary cystine excretion (Perazella and Buller, 1993). However, the effect was not confirmed by other investigators (Dahlberg and Jones, 1989; Barbey et al. The lack of efficacy of captopril was not unexpected considering that two molecules of captopril is required to bind one molecule of cystine. Therefore, due to this stoichiometry, a sufficient amount of captopril could not be safely administered to adequately lower urinary cystine excretion. It has been suggested that ascorbic acid is an effective treatment for cystinuria. The recommended dose is 3 g/day for children and 5 g/ day for adults (Lux and May, 1983; Knoll et al. However, it is argued that its effectiveness is due to provision of alkali from the effervescent ascorbic acid tablet which contains bicarbonate (Birwe et al. Additionally, excessive ascorbic acid ingestion may increase the risk of CaOx stone formation since this acid is one of the major precursors of oxalate formation (Traxer et al. Oral and intravenous glutamine was shown to lower urinary cystine excretion (Miyagi et al. This was suggested to be due to increased renal tubular cystine reabsorption or reduced renal tubular cystine secretion (Miyagi et al. However, the result of this study remained unverified by other investigators (Van Den Berg et al. Unfortunately, there is still a tendency for practitioners to consider a spontaneous stone passage as a resolution and failure to do so as a surgical disease. There is a dire need for pathophysiologic investigation of kidney stones not only to unveil underlying causes but to direct therapy to normalize urinary chemistry. Empirical manipulation of urinary risk factors by dietary and pharmacologic means is very effective in prevention of recurrence and this approach should be adopted and mastered by physicians. Additive hypocalciuric effects of amiloride and hydrochlorothiazide in patients treated with calcitriol. Resolution of medullary nephrocalcinosis in children with metabolic bone disorders. Incidence and clinical importance of renal tubular defects in recurrent renal stone formers. Randomized double-blind study of potassium citrate in idiopathic hypocitraturic calcium nephrolithiasis. Citrate, malate and alkali content in commonly consumed diet sodas: implications for nephrolithiasis treatment. Pharmacological interventions for preventing complications in idiopathic hypercalciuria. Long-term treatment with potassium citrate and renal stones in medullary sponge kidney.
This instrument is easily accessible on the Internet or in mobile calculator applications for smart phones blue sky pain treatment center/health services 10 mg maxalt order otc. Patients seem to want to be informed about prognosis and survival data (Schell et al. Additional prognostic scoring approaches have been published and several administrative database studies are underway. They identified nine risk factors and assigned points to them with increase in mortality correlating with increased number of points. One of the limitations of their score was that the population did not account for elderly patients not yet on dialysis and the authors suggested that this score be used to evaluate patients with no obvious contraindications for dialysis (Couchoud et al. A point score was assigned to these characteristics and increased in the point system correlated with mortality (Cheung and Kurella Tamura, 2011). Other studies using large administrative databases like the United Kingdom Renal Registry database and the United States Renal Data System database have looked at predicting mortality using co-morbidities and they have showed similar findings (Liu et al. It is our hope that larger multicentre randomized control trials can be performed to provide a more solid basis for recommendations and to generate new hypothesises for improving care. Differentiating suicide from life-ending acts and end-of-life decisions: a model based on chronic kidney disease and dialysis. No Good Deed: a Story of Medicine, Murder Accusations, and the Debate Over How We Die. Practical considerations in dialysis withdrawal: "To have that option is a blessing". A comparison of methods to communicate treatment preferences in nursing facilities: traditional practices versus the physician orders for life-sustaining treatment program. The need for end-oflife care training in nephrology: national survey results of nephrology fellows. Currently this is done with advance care planning documents completed by the patient. The completion of these documents and their fidelity to the decisions has generally been poor (Perkins, 2007). Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis (2nd ed. Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis. Predicting mortality in incident dialysis patients: an analysis of the United Kingdom Renal Registry. Stopping long-term dialysis: an empirical study of withdrawal of life-supporting treatment. Conventional haemodialysis performed three times a week for 4 hours per treatment filters the blood for only 12 of 168 hours each week, and removes < 10% of small solutes like urea than does the normal kidney. It is therefore not surprising that haemodialysis patients suffer high morbidity and mortality. For example, a woman aged 4044 years old in the general population can expect on average 40 more years of life, but if she is on dialysis her life expectancy is only 8. She is also more likely to have co-morbid disease, including hypertension, cardiovascular disease, metabolic bone disease, anaemia, sepsis, depression, malnutrition and inflammation, and physical and cognitive impairment. Session length In addition to urea removal, session length itself may be a measure of dialysis dose. A more recent observational study of thrice-weekly haemodialysis demonstrated an inverse association between haemodialysis session length and mortality independent of the effects of session duration on the urea clearance. Brunelli and colleagues analysed data from a national cohort of 8552 incident patients on thrice-weekly haemodialysis using marginal structural analysis to adjust for time-dependent confounding (Brunelli et al. They found that shorter haemodialysis sessions were associated with higher mortality and there was a dose-dependent relationship between session duration and mortality. These studies have focused on the hours of dialysis and the efficiency of solute removal. The National Cooperative Dialysis Study, a randomized trial published in 1981, showed that increased urea removal improved morbidity. There also was a trend to decreased morbidity with increased dialysis session time, but this result did not attain statistical significance (Lowrie et al. In this study, patients were randomized in a 2 by 2 factorial design to high versus standard dose (as measured by urea clearance) and to high- or low-flux dialysers. In this trial, the high doses were achieved primarily by slightly increasing dialysis time. Despite adequate statistical power, patients receiving the higher dose did not have any improvement in mortality compared to the standard dose group. Women randomized to the lower-dose group had a higher mortality than women treated with the higher dose (Depner et al. A subsequent post hoc analysis demonstrated that if the dose was normalized to body surface area rather than volume, the dose of dialysis delivered to women Session frequency For more than 40 years, conventional chronic haemodialysis has been delivered three times a week. Patients receive treatments Monday, Wednesday, and Friday, or Tuesday, Thursday, and Saturday. This model of dialysis provides a 2-day interval between dialysis treatments once a week-Friday to Monday, or Saturday to Tuesday. Several studies suggest that the long 2-day dialysis-free interval each week for conventional thrice-weekly haemodialysis is particularly dangerous. Cardiac arrests occur more frequently on Mondays and Tuesdays, after the long interdialytic interval (Bleyer et al.
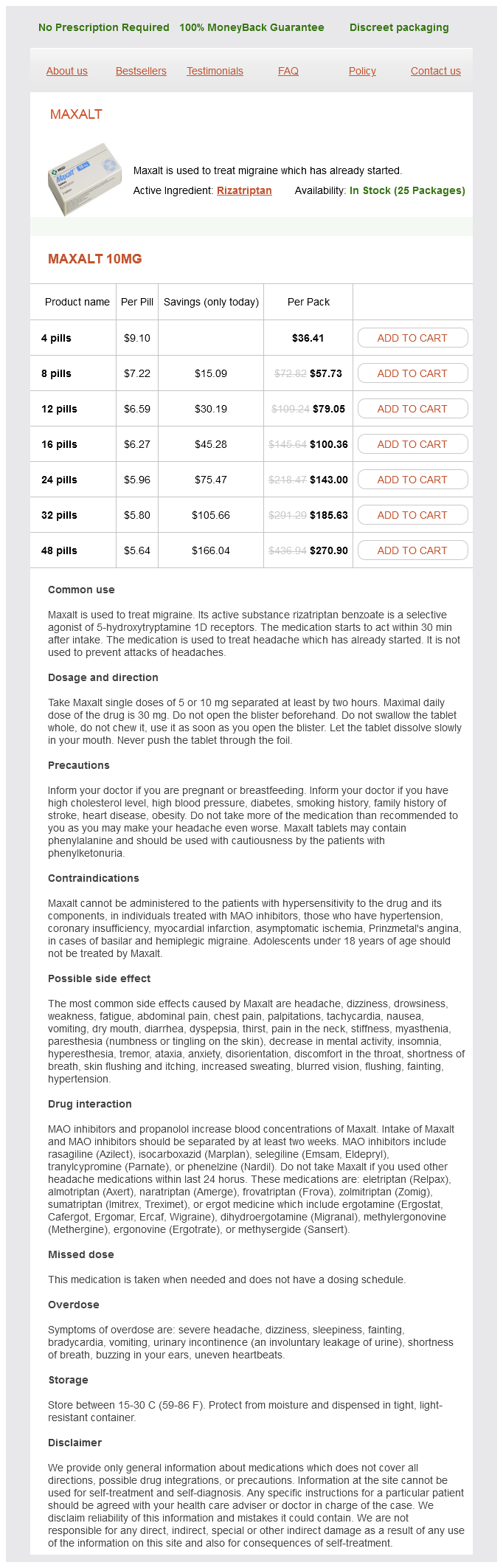
Maxalt Dosage and Price
Maxalt 10mg
- 4 pills - $36.41
- 8 pills - $57.73
- 12 pills - $79.05
- 16 pills - $100.36
- 24 pills - $143.00
- 32 pills - $185.63
- 48 pills - $270.90
The Marmara earthquake: epidemiological analysis of the victims with nephrological problems pain medication for dogs advil 10 mg maxalt order otc. The Marmara earthquake: admission laboratory features of patients with nephrological problems. Clinical findings in the renal victims of a catastrophic disaster: the Marmara earthquake. Renal replacement therapies in the aftermath of the catastrophic Marmara earthquake. Lessons learned from the catastrophic Marmara earthquake: factors influencing the final outcome of renal victims. Earthquakes and crush syndrome casualties: lessons learned from the Kashmir disaster. Studies of mechanisms and protective maneuvers in myoglobinuric acute renal injury. Combined mannitol and deferoxamine therapy for myohemoglobinuric renal injury and oxidant tubular stress. Iron, heme oxygenase, and glutathione: effects on myohemoglobinuric proximal tubular injury. Medical support in the Tangshan earthquake: a review of the management of mass casualties and certain major injuries. Rhabdomyolysis and myoglobinuric renal failure in trauma and surgical patients: a review. Intervention of the Renal Disaster Relief Task Force in the 1999 Marmara, Turkey earthquake. Acute renal failure related to the crush syndrome: towards an era of seismo-nephrology The annual incidence of burns ranges between 11 and 52/10,000 population (Othman and Kendrick, 2010) and 422% of these require hospitalization (0. Nevertheless, severe burns are associated with a high risk for morbidity and mortality, due to often extensive wounds, the associated trauma. Since this meta-analysis, several recent, large studies have confirmed these findings (Mosier et al. Decreased kidney perfusion, secondary to burn shock and inflammation, are two important contributing factors (Colpaert and Hoste, 2008). The exact role of renal ischaemia and hypoperfusion is uncertain, but may be less prominent than presumed (Arturson, 1985; Langenberg et al. Instead, inflammation and apoptosis may be important causal factors (Jeschke et al. Inflammatory response and infection Local inflammation following injury is essential for wound healing and host defence against infection. Both of these phases are characterized by fever, the generation of acute phase proteins, and an overall state of catabolism, mediated by several local and systemic inflammatory mediators and stress hormones (Church et al. There is an increase in the levels of vasopressin, aldosterone, growth hormone, cortisol, glucagon, and catecholamines. The anti-inflammatory response and the subsequent immunosuppression following burn injury are characterized by a set of opposing cell types and cytokines. The primary therapeutic goal in treating hypovolaemic shock is to promptly restore vascular volume and to preserve tissue perfusion in order to minimize tissue ischaemia (Baker et al. The extent of gut oedema and amount of ascites, by increasing the volume of the abdominal cavity, might also be important contributing factors (Oda et al. Intra-abdominal hypertension leads to decreased renal arteriolar and microcirculatory blood flow and also increased renal venous pressure (Bradley and Bradley, 1947; Harman et al. Burn shock is caused by fluid losses through burned skin, and massive fluid shift from the blood into the interstitial compartment, especially in burned tissue, but to a lesser extent also in non-injured organs and tissues (Lund et al. Oedema development in burned skin is characterized by the extremely rapid onset of tissue water content, which can double within the first hour (Arturson, 1985). The amount of oedema formation depends on the type and extent of the injury, as well as the type and volume of fluid administration (Arturson, 1985; Lund et al. Burn shock is thus characterized by haemodynamic changes similar to those that occur after haemorrhage, including decreased plasma volume, cardiac output, and urine output, and increased system vascular resistance resulting in a reduction of peripheral blood flow. Intra-abdominal pressure can easily be measured by means of a urinary bladder catheter, and intra-abdominal hypertension can thus be detected in an early phase. Routine measurement of intra-abdominal pressure is thus recommended in patients with severe burn injury (Ivy et al. It is distributed in a plasmatic and extraplasmatic volume with slow transport to the plasmatic compartment; hence the dialyser clearance during high-flux dialysis is comparable with that of small solutes such as urea. Intercompartmental clearance of iodine is low and more comparable to that of beta-2 microglobulin, which mandates long treatment times. Nowadays it is well known that even moderate decreases in kidney function may have a negative impact on outcome (Hoste et al. Breakdown of damaged skeletal muscles leads to the release of breakdown products. Povidone-iodine Since complete wound closure by skin grafting following debridement often takes several days to weeks, the topical antimicrobial agent povidone-iodine for burn dressing is often used to avoid infection. Yet, in extensive burns, this may lead to elevated blood iodine concentrations, secondary to increased absorption in combination with hampered renal excretion (Lavelle et al.