Movfor
General Information about Movfor
In a phase 2/3 medical trial involving over 1,200 individuals with delicate to moderate COVID-19, Movfor showed vital progress in lowering the duration of signs. The research found that patients who acquired the medication recovered from the virus in a median of 6.8 days, in comparability with 9.7 days for many who received a placebo. This discount in recovery time could probably be essential in preventing extreme sickness and potential hospitalization.
BioNTech plans to file for emergency use authorization for Movfor in the second quarter of 2021, and if permitted, the treatment might turn out to be obtainable for use later this yr. This might have a big impact on the continuing pandemic, as an efficient oral medicine might probably decrease the burden on healthcare systems and save numerous lives.
The improvement of Movfor as an oral antiviral therapy for COVID-19 is a serious breakthrough in the battle in opposition to the pandemic. Its unique mode of action and promising outcomes from medical trials give hope for a more effective treatment for the virus. If permitted, Movfor could have a significant influence on the worldwide effort to manage and mitigate the consequences of COVID-19.
One of the key benefits of Movfor is that it might be taken orally, in contrast to different COVID-19 therapies that require intravenous infusion. This is a significant game-changer within the struggle towards the virus, because it allows for extra handy and less invasive administration of the medication. This is particularly beneficial for those in distant or underserved areas who could not have access to hospital services.
Movfor works by targeting the main protease of the virus, an enzyme that is important for the virus to duplicate and unfold. The medicine binds to this protease, preventing it from functioning and in the end stopping the virus from multiplying in the physique. This distinctive mode of motion units Movfor other than other COVID-19 remedies at present out there, which largely target the signs of the disease rather than the virus itself.
Additionally, the trial also showed a major reduction in viral load in sufferers who obtained Movfor, indicating that the medicine was successful in inhibiting the replication of the virus. This might also potentially reduce the prospect of transmission to others, thus serving to to manage the spread of the virus.
Another necessary side of oral administration is that it could probably be taken at an earlier stage of the illness, as patients wouldn't must be hospitalized to receive the therapy. This could result in higher outcomes and probably prevent extra severe instances of COVID-19.
Movfor is an oral antiviral remedy developed by the pharmaceutical firm BioNTech, recognized for growing the extremely successful Pfizer-BioNTech COVID-19 vaccine. This revolutionary treatment is designed to inhibit the replication of the SARS-CoV-2 virus, which causes COVID-19, and therefore prevent it from spreading and causing additional harm.
In addition to its impression on COVID-19, Movfor has the potential for use as a preventative therapy for other kinds of coronavirus infections. This could probably be notably helpful as more variants of the virus emerge and pose a threat to public health.
The COVID-19 pandemic has swept the world and introduced with it immense challenges and devastation. As scientists and researchers scramble to search out efficient treatments and vaccines, the pharmaceutical industry has been racing to develop drugs that can alleviate symptoms and help in restoration. One such remedy that has been making headlines is Movfor, an oral antiviral medication that has shown promising leads to the fight against COVID-19.
N-Stage N0 No regional lymph node metastases N1 Regional lymph node metastases Note: Regional lymph nodes are along the common bile duct hiv infection essay purchase movfor 200 mg visa, common hepatic artery, back toward the coeliac trunk, posterior and anterior pancreaticoduodenal nodes, and along the superior mesenteric vein and the right lateral wall of the superior mesenteric artery. Histological examination of a regional lymphadenectomy specimen will ordinarily include 12 or more lymph nodes. N-Stage N0 No regional lymph node metastases N1 Regional lymph node metastasis, including nodes along the cystic duct, common bile duct, hepatic artery and portal vein N2 Metastasis to periaortic, pericaval, superior mesenteric artery and/or coeliac artery lymph nodes M-Stage M0 No distant metastases M1 Distant metastases Staging groups for perihilar cholangiocarcinoma Stage 0 1 M-Stage M0 No distant metastases M1 Distant metastases this T1 N0 N0 M0 M0 Continued Pathology and staging 443 Stage 2 3a 3b 4a 4b T2ab T3 T13 T4 Any T Any T N0 N0 N1 Any N N2 Any N M0 M0 M0 M0 M0 M1 Stage 3 4a 4b T3 T4 Any T Any T N0 N0 N1 Any N M0 M0 M0 M1 Gallbladder cancer [13] T-Stage this Carcinoma in situ T1 Tumor invades lamina propria (T1a) or muscular layer (T1b) T2 Tumor invades perimuscular connective tissue; no extension beyond serosa or into liver T3 Tumor perforates the serosa (visceral peritoneum) and/or directly invades the liver and/or one other adjacent organ or structure, such as the stomach, duodenum, colon, pancreas, omentum or extrahepatic bile ducts T4 Tumor invades main portal vein or hepatic artery or invades at least two extrahepatic organs or structures N-Stage N0 No regional lymph node metastasis N1 Metastases to nodes along the cystic duct, common bile duct, hepatic artery and/or portal vein N2 Metastases to periaortic, pericaval, superior mesenteric artery and/or coeliac artery lymph nodes Note: Histological examination of a regional lymphadenectomy specimen will ordinarily include three or more lymph nodes. If the regional lymph nodes are negative, but the number ordinarily examined is not met, classify as pN0. Intrahepatic cholangiocarcinoma [13] T-Stage this Carcinoma in situ T1 Solitary tumor without vascular invasion T2a Solitary tumor with vascular invasion T2b Multiple tumors, with or without vascular invasion T3 Tumor(s) perforating the visceral peritoneum or involving the local extrahepatic structures by direct invasion T4 Tumor with periductal invasion Note: Intrahepatic cholangiocarcinoma is a tumor within the liver, arising from the bile ducts proximal to the second-order bile ducts. N-Stage* N0 No regional lymph node metastases N1 Regional lymph node metastases * Right-liver intrahepatic cholangiocarcinoma regional lymph nodes include the hilar (common bile duct, hepatic arteries, portal vein and cystic duct), periduodenal and peripancreatic lymph nodes. Left-liver intrahepatic cholangiocarcinoma regional lymph nodes include the hilar and gastrohepatic lymph nodes. Histological examination of a regional lymphadenectomy specimen will ordinarily include three or more lymph nodes. M-Stage* M0 No distant metastases M1 Distant metastases * M-Stage M0 No distant metastases M1 Distant metastases Spread to the coeliac or periaortic and caval lymph nodes is distant metastasis. State-of-the-art imaging techniques are vital for accurate assessment of resectability and, thus, for treatment planning. Diagnosis and preoperative staging 445 part of the tumor is typically enhanced on delayed images obtained approximately 5 min a er contrast injection. Capsule retraction is o en seen, although it is not pathognomonic for cholangiocarcinoma. For tumor staging, contrast-enhanced images are important to demonstrate vascular invasion, satellite nodules and peritoneal spreading [17,18]. Moreover, biliary decompression induces biliary in ammation, which can severely interfere with the delineation of the longitudinal tumor extent into the biliary system. In this patient with a small distal cholangiocarcinoma, stent-induced artefacts impair visualization of the tumor. Early gallbladder cancer may present as an incidental nding during ultrasound work-up for abdominal complaints, with non-speci c ndings such as a small polypoid lesion or wall thickening. On the other hand, a variety of benign gallbladder diseases may mimic gallbladder cancer. Especially focal wall thickening due to fundal type of adenomyomatosis or mass-forming xanthogranulomatous cholecystitis may be di cult to di erentiate by imaging [21]. Typical imaging features include a discrete mass or focal wall thickening or, less commonly, di use wall thickening [22]. In the hepato-biliary phase (d) extensive tumor infiltration into the liver is depicted (arrows). Palliative drainage of hilar cholangiocarcinoma is necessary in the majority of patients, who are diagnosed at a stage when surgical resection is not an option. In general, selfexpanding metal stents are superior to plastic biliary stents because of longer median patency times [26]. However, local expertise o en guides the treatment approach in these patients and multimodality treatment is o en required. If one of the above is present preservable volume should be kept above 40% of the total liver volume; otherwise 30% is accepted. Major hepatectomy has to be done with an anaesthesiology team that is aware of low-volume anaesthesia, intraoperative use of vasopressors to maintain minimum arterial blood pressure (around 100 mmHg) during liver transection and the speci c postoperative volume management a er intraoperative volume depletion. Liver resection including biliary duct resection and reconstruction should include postoperative local anastomotic drainage to detect potential leakage at an early stage. Radical surgical removal with clear margins is the only accepted curative therapy. Prior to 448 Carcinoma of the biliary tree and gallbladder where the cancer lies, has to be removed in any potential curative procedure. Vascular resections at the hilum are possible and recommended by some groups, but their invasion a ects immediate (postoperative morbidity and mortality) and long-term prognosis. Similar to the gallbladder cancer the involvement of ligamentary vascular structures often determines potential local radical surgery and can often only be explored intraoperatively. As long as minimum remaining liver volume is guaranteed with adequate in- and out ow, liver dysfunction is seldom a problem due to normal regenerating remnant liver [30]. If the gallbladder was not removed with a bag during laparoscopic resection or the gallbladder perforated (a bad prognostic factor) the port sides should be re-excised during a second procedure. Advanced T-stage including T4 tumors is not a contraindication for resectability as long as the tumor is located in the fundus; these tumors require major liver resection with potential resection of the transverse colon. Segment I which is draining into the ductal bifurcation, Locally advanced and metastatic disease 449 e achievement of a curative resection of an advanced tumor located at the infundibulum is much more di cult because it requires the resection of the bile duct, at least the bulbus duodeni and potentially the pancreatic head, together with a major hepatectomy, especially if right-sided vessels (right hepatic artery, right portal vein) are involved. In a recently published paper, a nomogram was designed in which a possible bene t of an adjuvant radiochemotherapy in patients with resected gallbladder cancer was shown [41]. Further clinical prospective randomized trials are urgently needed to de ne a standard approach a er surgery. Patients have to be in a good performance status without severe comorbidities, and it is necessary that a su cient biliary decompression was performed before starting palliative chemotherapy in jaundiced patients. In most of the studies patients with intrahepatic, extrahepatic, gallbladder cancer, cancer of the ampulla Vateri and even pancreatic cancer are included.
One explanation for this controversy may be the impact of e ective adjuvant (or neoadjuvant) chemotherapy hiv infection rates over time 200 mg movfor buy fast delivery. Tumor factors Microscopically negative surgical margins (R0) have traditionally been considered an important prognostic factor. It has been argued that it is biology, not millimetres, that dictates prognosis following resection. Recently, attention has turned to the use of biological and molecular markers as a more accurate means to predict long-term outcomes. Patient and tumorspeci c markers may provide more accurate predictions of survival a er hepatic resection for colorectal metastases. Preoperative chemotherapy is being increasingly used, to allow previously unresectable patients to become resectable as well to increase the chance of cure of truly resectable patients. In addition to assessment on preoperative imaging, tumor response can be assessed on pathological examination a er liver resection. Using a semi-quantitative scale of the number of residual cancer cells may allow classi cation of patients according to complete response (no residual cancer cells), major response (149% of residual cancer cells) or minor response (50% residual cancer cells), respectively. For the liver, contrast enhancement of the arterial and portal phases is required. Several intravenous contrast agents are available to improve detection and characterization of liver lesions. In per-lesion analysis, the di erence is higher when liver-speci c contrast agents are administered and for lesions smaller than 10 mm. It should be considered in all patients with metastatic disease con ned to the liver, irrespective of the size, number or multilobar localization of the lesions, as long as all lesions can be removed adequately while leaving enough functional liver reserve. Detailed knowledge of the segmental structure of the liver is essential for a safe surgical procedure. A large variety of resections can be undertaken, following the distribution of the metastases. A liver-sparing approach o ers signi cant better opportunities for secondary liver surgery and facilitates postoperative recovery. Surface-oriented metastases can be excised by non-anatomic wedge resections, whereas deeper solitary lesions can be treated by segmentectomy or bisegmentectomy. Large or multiple metastases are treated by right or le hepatectomy or multiple segmentectomies in case of bilobar disease. Several methods of vascular clamping can be applied to control intraoperative hemorrhage, such as non-selective intermittent clamping of the portal triad (Pringle maneuver); complete vascular exclusion of the liver, including clamping of the hepatic pedicle and infra- and suprahepatic vena cava; and selective vascular occlusion or ligation of the hepatic artery, portal vein and hepatic vein of the depending site of the parenchymal resection. Smaller vessels that are encountered are coagulated, while larger vessels and biliary structures are ligated. Several instruments are available on the market to facilitate parenchymal dissection such as ultrasonic dissectors and water-jet dissectors. More recently, coagulation equipment has been developed to transect the liver tissue, by sealing the vascular structures or by coagulation of liver tissue with the help of radiofrequency energy. Perioperative mortality and morbidity Although the mortality rate a er hepatic resection has declined to less than 5%, in most major centres over the past 20 years, as a result of advances in operative techniques and perioperative care, it has been shown that actual population-based mortality rates for liver resection are higher than those reported in the literature from highvolume centres. Furthermore, most studies have quoted inhospital or 30-day mortality, which may be as little as half the 90-day mortality rate that has now become the standard metric. In a recent population-based study from France, the in-hospital and 90-day mortality rates were 3. It has also recently been emphasized that the risk of death following hepatic surgery is lower at highvolume hospitals and patients treated at low-volume hospitals who have a complication are 40% more likely to die than patients with a complication in a high-volume hospital [16]. Sepsis, wound infection, urinary tract infection and organ space infection are the most common complications. Male gender, previous cardiac operation, American Society of Anesthesiologists class 3 or higher score and disseminated cancer are signi cantly associated with higher complication rates [17]. In a recent meta-analysis of 2280 patients, 35% of patients experienced at least one postoperative complication. Whether this association is the result of a direct causee ect relationship or the consequence of a more extensive surgery for a higher tumor burden is still under debate. Nevertheless, in order to reduce complication rates, e orts should be made to reduce preoperative chemotherapy duration to a maximum of eight cycles (4 months), to avoid combined major liver and primary resections in case of synchronous metastases, to avoid major resections and consider two-stage procedures for bilateral metastases, to use portal vein embolization to reduce the risk of liver failure, and to favor non-anatomic resections or ablation rather than sacri cing a huge volume of healthy parenchyma, in patients presenting with multiple metastases [19]. Repeat hepatectomy Repeat curative intent hepatectomy for recurrence is being increasingly performed with associated survival rates identical to those of the rst hepatectomy. More importantly, the recurrence-free bene t of repeat curative intent surgery is similar regardless of the number of times previous surgery has been performed. Non-anatomical resections should therefore be preferred, saving the maximum amount of normal liver parenchyma, provided that safe tumor margins can be achieved [25]. Attempting to convert unresectable into resectable disease is a worthwhile aim, with 5-year survival rates for patients with tumors chemo-converted to resectability being similar to those of patients who underwent resection at presentation [20]. As a result, it is recommended that patients with unresectable liver-only disease should be treated with the most aggressive regimen possible. Regional liver chemotherapy infusion Regional liver chemotherapy infusion is a logical approach since the liver represents the main site of relapse a er resection of hepatic metastases. In the future, it will be interesting to better evaluate locoregional chemotherapy regimens containing oxaliplatin or irinotecan. Additionally, in the intent-to-treat analysis, the di erence between the two arms was not statistically signi cant, probably as a result of a lack of power. Moreover, it is now likely that future trials will be carried out on selected subgroups of patients with a high risk of recurrence. Patients with steatohepatitis may have an increased postoperative 90-day mortality rates (14.
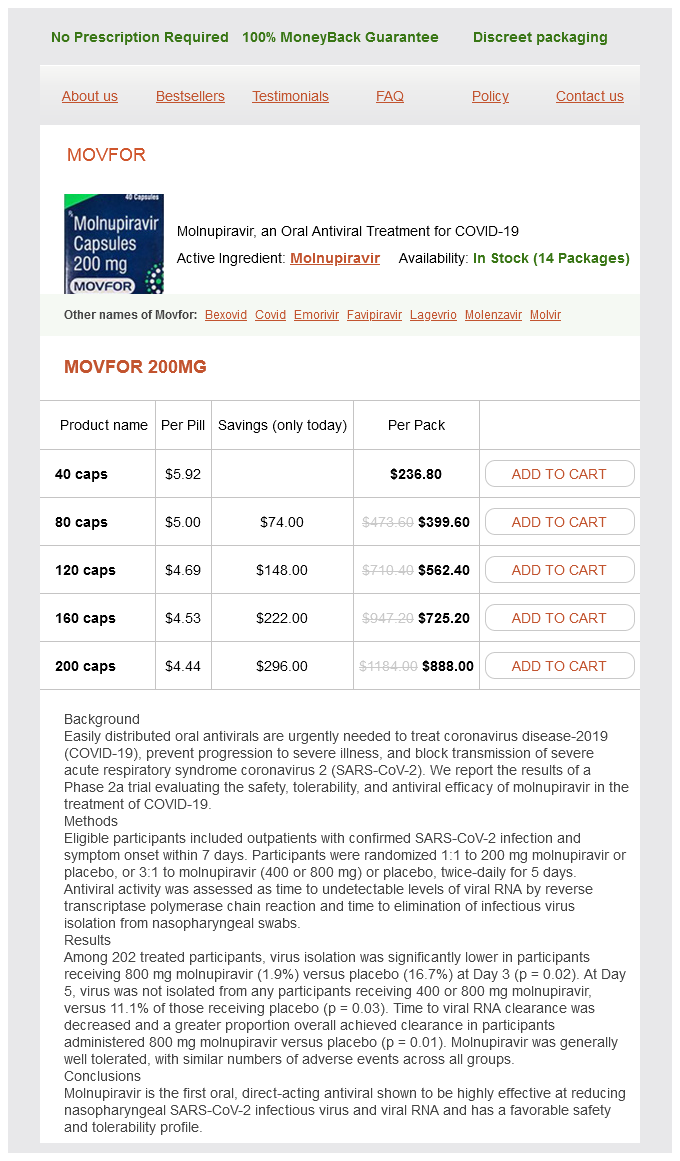
Movfor Dosage and Price
Movfor 200mg
- 40 caps - $236.80
- 80 caps - $399.60
- 120 caps - $562.40
- 160 caps - $725.20
- 200 caps - $888.00
The spectral responsivities of different photodiodes in hand held dosimeters vary considerably and typically have a bell shape hiv infection victoria order movfor 200 mg line. Such errors can also give rise to false conclusions about the spectral dependence of biological outcomes. A good spectroradiometer will have a dynamic range of about six orders of magnitude. When total irradiance is erythemally weighted (see section on action spectroscopy) this increases to 18%/1000 m [6]. This is a sealed glass tube that contains mercury and an inert gas, typically argon. However, it should be noted that in reality this is narrow band polychromatic radiation with a bell shape. It then eventually exits, unless it first collides with and is absorbed by an appropriately structured molecular moiety, known as a chromophore. Thus the basis of all skin photobiology, whether acute or long term, is photochemistry. The above examples are referred to as direct responses because the chromophore is also the target molecule that initiates the photobiological response. Indirect responses also occur, in which the chromophore is not the molecule that causes the response per se. The first is the identification of the chromophore that is responsible for the biological response and this is critical for the understanding of a photobiological mechanism. Under ideal conditions, an action spectrum of a given biological response can be superimposed on the absorption spectrum of the chromophore that initiates the response. A good nondermatological example is similarity of the action spectrum for photosynthesis and the absorption spectrum of chlorophyll. Biological weighting with action spectra can often give surprising results, such that <1% of a given emission spectrum may be responsible for the vast majority of a given biological or clinical response [13]. The determination of good action spectra for human skin is technically demanding and very time consuming. Reliable biological weighting requires very high quality spectroradiometric measurements. The action spectrum for normal erythema can be altered by administration of an exogenous chromophore. The insertion of an incorrect base in proliferating epidermal cells may result in mutations that give rise to skin cancer. Pyrimidine dimers (also known as dipyrimidine lesions) form after the absorption of photon energy that splits the C5=C6 double bonds of two adjacent pyrimidine bases, and forms new covalent bonds linking the two pyrimidines at the C5 and C6 positions. In both processes, repair continues through a transcription factor replicosome complex consisting of 30 distinct proteins in human cells. This includes nuclear transcription factors and genes associated with inflammation, immunoregulation and the remodelling of extra cellular proteins. Cellular effects Ultraviolet radiation exposure of the skin results in a wide range of cellular effects. Their formation is regulated by p53 that can be readily demonstrated by immunostaining. This is followed by a thickening of the epidermis, particularly the stratum corneum. Erythema may be associated with pain, warmth and oedema (blanching) in severe cases. Erythema is also associated with increased sensitivity to pain from mechanical and thermal stimuli, resulting in the skin feeling tender after sunburn [26]. This suggests that those with fair skin resolve erythema less well than those who tan readily. Erythema action spectra have been studied for over 90 years and a library of such spectra has been compiled [28]. Melanogenesis Delayed tanning (facultative pigmentation or neomelanogenesis) is due to stimulation of new melanin synthesis by basal epidermal melanocytes, which is then transported via dendrites to adjacent keratinocytes and redistributed towards the surface of the skin. Melanin is synthesized either as darkcoloured brownblack insoluble eumelanin or lightcoloured redyellow, alkali soluble, sulphurcontaining phaeomelanin. There is in vitro and animal evidence that products relating to melanogenesis particularly phaeomelanin may have photosensitizing properties contributing to the skin cancer susceptibility of people with red hair. New melanin is redistributed with the transit of keratinocytes through the epidermis and is typically evident 3 days postirradiation. A small degree of tyrosinase stimulation also occurs through fibroblasts, neurons and mast cells. A similar role is likely to occur for humans, though this is impossible to test experimentally. It is clear that an intact immune system is important for skin cancer surveillance and tumour rejection because organ transplant patients, maintained on immunosuppressive drugs, have a high incidence of all types of skin cancer, especially on sunexposed sites. A major difference between druginduced immunosuppression and photoimmunosuppression is that the latter is antigen specific. This model is widely used to represent the photoimmunological events in skin cancer. The downside of the suppression of photoimmunosuppression is the failure of the immune system to reject potentially carcinogenic clones of keratinocytes and melanocytes. Selection pressure is likely to have had a preference for the prevention of allergic reactions, given that skin cancer typically occurs well past the age of reproduction and child rearing. However, this cannot be done for chronic effects for which an epidemiological approach is necessary. There has been extensive epidemiological research on skin cancer that has been supported by animal and in vitro studies.