Mycelex-g
General Information about Mycelex-g
Symptoms of a vaginal yeast infection can include itching, burning, and irritation within the vaginal area, in addition to irregular vaginal discharge that is usually thick and white, resembling cottage cheese. While these infections aren't thought of serious, they are often uncomfortable and disruptive to daily life.
This is where Mycelex-G comes into play. This treatment is specifically designed to deal with vaginal yeast infections and has been proven to be extremely efficient in doing so. Its lively ingredient, Clotrimazole, works by inhibiting the expansion of the fungus, thus relieving the signs of the infection.
It can also be a secure and well-tolerated medication, with minimal potential unwanted facet effects. Some women might expertise mild burning or irritation during use, however these results are normally momentary and subside because the physique adjusts to the treatment.
One of the most important advantages of Mycelex-G is that it's out there over-the-counter, meaning it doesn't require a prescription from a physician. This makes it simply accessible to girls who might expertise frequent yeast infections, saving them a trip to the doctor's workplace and the associated costs.
In addition to treating vaginal yeast infections, Mycelex-G may also be used to forestall them. Women who are prone to recurrent yeast infections may profit from utilizing this treatment on the first signal of symptoms to prevent the infection from absolutely creating.
This treatment works by stopping the expansion of fungus that causes the an infection. It belongs to the azole family of medications, which additionally consists of other commonly used antifungal medicine such as fluconazole and ketoconazole.
Vaginal yeast infections, also referred to as vulvovaginal candidiasis, are one of the most common kinds of fungal infections skilled by women. According to the Centers for Disease Control and Prevention (CDC), roughly 75% of women will experience a minimal of one vaginal yeast an infection of their lifetime. These infections are caused by an overgrowth of a fungus known as Candida albicans, which is of course current within the vagina. However, when the balance of bacteria and yeast in the vagina is disrupted, it could lead to an overgrowth of the fungus, leading to an an infection.
Like all medications, Mycelex-G does have some contraindications and precautions. Women who are pregnant or trying to become pregnant, in addition to those who are allergic to any of the ingredients within the medication, should seek the assistance of with their physician before utilizing Mycelex-G.
In conclusion, Mycelex-G is a highly effective and accessible treatment for vaginal yeast infections. Its confirmed outcomes and minimal unwanted facet effects make it a preferred selection for so much of women. However, as with every treatment, you will want to seek the assistance of with a doctor if symptoms persist or worsen. Overall, Mycelex-G offers a convenient and reliable resolution for treating and stopping vaginal yeast infections, serving to women to regain their comfort and confidence.
However, you will want to observe that if symptoms do not enhance after seven days of therapy, or in the event that they worsen, a physician should be consulted. This might indicate that the infection is attributable to a different sort of fungus or that the an infection is more extreme and requires a special therapy.
Mycelex-G is available in two varieties – as a cream and as a vaginal pill. The cream is applied directly to the affected space, while the tablet is inserted into the vagina. Both forms of the treatment are used once a day for seven days to successfully deal with the an infection. It is necessary to finish the complete course of therapy, even when symptoms enhance, to prevent the an infection from returning.
Epithelioid Hemangioendothelioma Epithelioid hemangioendothelioma has biologic behavior and histologic features intermediate between benign hemangioma and angiosarcoma fungus gnats wood order 100 mg mycelex-g. It has a tendency to extend through tributaries of the portal and hepatic veins to form multifocal nodules. These nodules vary in size and tend to coalesce into large confluent masses, usually in the periphery of the liver. Tumor nodules characteristically have a peripheral hyperemic rim surrounding a dense fibrotic hypovascular central core. Epithelioid hemangioendothelioma may sclerose and elicit a desmoplastic response, thereby causing inward retraction of the overlying hepatic surface. Microscopically the tumors are composed of epithelioid round cells and dendritic spindle cells within an abundant myxoid and fibrous stroma. Undifferentiated Embryonal Cell Sarcoma Undifferentiated embryonal cell sarcoma is usually a large (ranging from 10 to 30 cm in size), solitary, wellcircumscribed, encapsulated mass with variable areas of hemorrhage, necrosis, and cystic degeneration. At histopathology, undifferentiated embryonal cell sarcoma is composed of undifferentiated mesenchymal cells. These patterns differ from that of hemangioma, which characteristically shows progressive centripetal discontinuous nodule-like enhancement. Peripheral lesions are associated with hepatic surface retraction in 25% of cases. The cystic appearance has been attributed to high water content in the abundant myxoid stroma and may lead to misinterpretation of the solid tumor as an echinococcal cyst or abscess. The appearance is suggestive of a hypervascular malignancy but does not permit a specific diagnosis. Axial T2-weighted (A), precontrast T1-weighted (B), and dynamically enhanced T1-weighted images in the arterial (C), portal venous (D), and delayed phases (E) show multiple peripherally located masses in the liver that are heterogeneously hyperintense on the T2-weighted images. There is associated capsular contraction with several of the masses (arrows in A). The masses have peripheral enhancement in the arterial phase with delayed irregular central enhancement due to the presence of a central fibrous stroma. In the portal venous phase, the mass appears to be a multiloculated cyst with internal septations. Differential Diagnosis Hemangioma: Is T2 bright with T2 shine-through on diffusion-weighted imaging; it typically shows incomplete nodular enhancement peripherally with progressive fill-in. Metastases: Typically in the setting of a known primary malignancy, such as breast cancer. The may also cause capsular retraction but rarely have a predominant peripheral hepatic location. Hepatic abscess typically appears in older patients with associated suggestive symptomatology or demographics, such as fever and elevated white blood cell count and origin from an endemic area. The lesions tend to resemble metastases at imaging; it usually is not possible, based on imaging findings alone, to differentiate mesenchymal liver tumors from metastases or to differentiate the various histologic types (angiosarcoma, epithelioid hemangioendothelioma, undifferentiated embryonal cell sarcoma) from each other. Occasionally imaging features in conjunction with clinical and laboratory findings may suggest the correct diagnosis. A hemorrhagic mass with central progressive enhancement at dynamic imaging suggests the diagnosis of hepatic angiosarcoma. Peripheral confluent masses with "target" or complete halo-like enhancement and inward retraction of the overlying hepatic surface suggest the diagnosis of hepatic epithelioid hemangioendothelioma. Hypervascular Metastases Definition Hepatic metastases may be classified radiographically as hypervascular or hypovascular depending on their degree of enhancement relative to background hepatic parenchyma during the vascular phases after administration of contrast agents. Hypervascular metastases of the liver are those with intense late arterial-phase enhancement. Demographic and Clinical Features Metastases are the most common malignant hepatic tumors and occur 18 to 40 times more frequently than primary neoplasms. Their imaging appearance can be variable depending on the degree of underlying hepatic arterial supply. Although most liver metastases are hypovascular, some are hypervascular and thus are, in whole or in part, vividly hyperintense or hyperattenuating to the background liver parenchyma in the hepatic late arterial phase. Breast carcinoma and pancreatic adenocarcinoma metastases are occasionally hypervascular. Pathology Regardless of their origin, hypervascular liver metastases develop a rich capillary network due to tumor neoangiogenesis. This abnormal capillary network communicates with both the hepatic arterioles and sinusoids. Blood within the high-pressure hepatic arterioles quickly drains through the tumor capillary network into the sinusoids, raising pressure within the sinusoids and suppressing portal venous flow. Even though the primary tumors form a solid mass, hypervascular liver metastasis can have a cyst-like appearance ("cystic metastases"). This cyst-like appearance is more frequent in metastases from neuroendocrine tumors and sarcomas. Most hypervascular metastases are moderately hypointense on T1-weighted images, but they may be hyperintense due to hemorrhage or melanin deposition (melanoma). On T2-weighted and diffusion-weighted images, hypervascular metastases are usually moderately to markedly hyperintense. Hypervascular metastases enhance early and vividly after administration of contrast agents and tend to be more conspicuous in the late arterial phase than on more delayed phases. Small hypervascular metastases usually show homogeneous enhancement in the late arterial phase and then either fade to become isoenhanced or wash out to become hypoenhanced relative to liver in the venous phases.
After contrast administration fungus mulch discount mycelex-g 100 mg free shipping, tumor enhancement is observed, more pronounced on the arterial phase, with an irregular outer margin. Polypoid lesions are usually of intermediate signal intensity on T1-weighted images and moderately hyperintense on T2-weighted images. Management/Clinical Issues Surgery is considered to be the only curative treatment for gallbladder carcinoma. It is estimated to be approximately 10% at 5 years in cases with serosal involvement with or without lymph node metastasis. Extended and complete resection in highly selected patients with advanced disease may increase survival up to 31%. Differential Diagnosis Adenomyomatosis: May be difficult to distinguish from gallbladder cancer when there is pronounced gallbladder wall thickening. Gallbladder polyps: Large gallbladder polyps and those associated with focal gallbladder wall thickening or adenopathy should raise concern for malignancy in the polyp. Xanthogranulomatous cholecystitis: Often indistinguishable from gallbladder carcinoma preoperatively because it may have associated extension into the adjacent liver. Gallbladder metastases: Generally occur in the setting of a known primary cancer and widespread metastasis. Gallstones larger than 3 cm are thought to increase the risk for carcinoma 10-fold. May present as a subhepatic mass, frequently with trapped gallstones, as asymmetric and irregular gallbladder wall thickening, or as a polypoid lesion. Gallbladder carcinoma update: multimodality imaging evaluation, staging and treatment options. Gallbladder Metastases Key Points Uncommon malignancy despite being the most common malignancy of the biliary tract. Definition Gallbladder metastases stem from tumor growth in the gallbladder due to the transmission of neoplastic cells from a primary tumor located elsewhere in the body. Malignant melanoma is the most frequent cause of gallbladder metastasis, accounting for up to 60% of all cases. Other primary tumors that have a tendency to involve the gallbladder include renal cell carcinoma and hepatocellular carcinoma. When symptomatic, gallbladder metastases from melanoma are reported to cause acute cholecystitis, obstructive jaundice, external biliary fistula, and hemobilia. Pathology Metastatic melanoma to the gallbladder may present as multiple flat nodules or infiltrative lesions, but it may also manifest as a single polypoid lesion in the gallbladder. Differentiation between metastatic melanoma and primary melanoma may be difficult. Some 3% to 5% of patients present with metastatic melanoma in the gallbladder in the absence of a clinically detectable primary lesion. Imaging Findings Metastatic disease to the gallbladder may simulate the patterns of gallbladder carcinoma. However, the amount of melanin within the lesions is variable, and necrosis or hemorrhage may alter the signal characteristics of these lesions. After intravenous contrast administration, subtraction images may be needed to observe lesion enhancement, because these lesions may show inherent T1-weighted hyperintensity. Management/Clinical Issues Symptomatic patients and patients in whom melanoma is isolated to the gallbladder may benefit from cholecystectomy. Survival is estimated to be 39 months for patients in whom disease is confined to the gallbladder and 10 months for patients with multiple metastatic sites. Differential Diagnosis Gallbladder carcinoma: Is more common and has an identical appearance to metastatic melanoma and metastatic lesions from other sites. Clinically history is usually necessary to establish the diagnosis of primary versus metastatic disease. Gallbladder polyps: Benign gallbladder polyps such as adenomas may be identical when metastatic lesions present as a polypoid mass. Malignant melanoma is the most common primary tumor to metastasize to the gallbladder. Yeh Introduction the bile ducts are essential conduits that channel bile produced by the hepatocytes to the duodenum to aid in the emulsification and digestion of food. Normal Anatomy Tiny nonendothelialiized channels extend between cords of hepatocytes and coalesce into bile duct canaliculi and ducts in the portal triad. Normal intrahepatic bile ducts are slender, gracefully branching structures with smooth, uniform walls; they are less than 3 mm in diameter. The right and left bile ducts normally are less than 5 mm in diameter, and the common hepatic and common bile ducts are less than 7 mm in diameter. Although anatomic variants are common, the Couinaud segments 1, 2, 3, and 4 usually converge to form the left bile duct; segments 5 and 8 converge to form the right anterior bile duct, and segments 6 and 7 converge to form the right posterior bile duct. The right anterior and right posterior bile ducts converge to form the right bile duct. The left and right bile ducts then emerge from the liver parenchyma at the liver hilum and join to form the common hepatic duct, which runs parallel to the main portal vein. At a variable distance from the hilum, the cystic duct from the gallbladder joins the common hepatic duct to form the common bile duct, which then traverses the pancreatic head and drains into the ampulla of Vater. The cystic duct may run parallel to the common hepatic duct and give a false appearance of dilatation of the common hepatic bile duct at imaging.
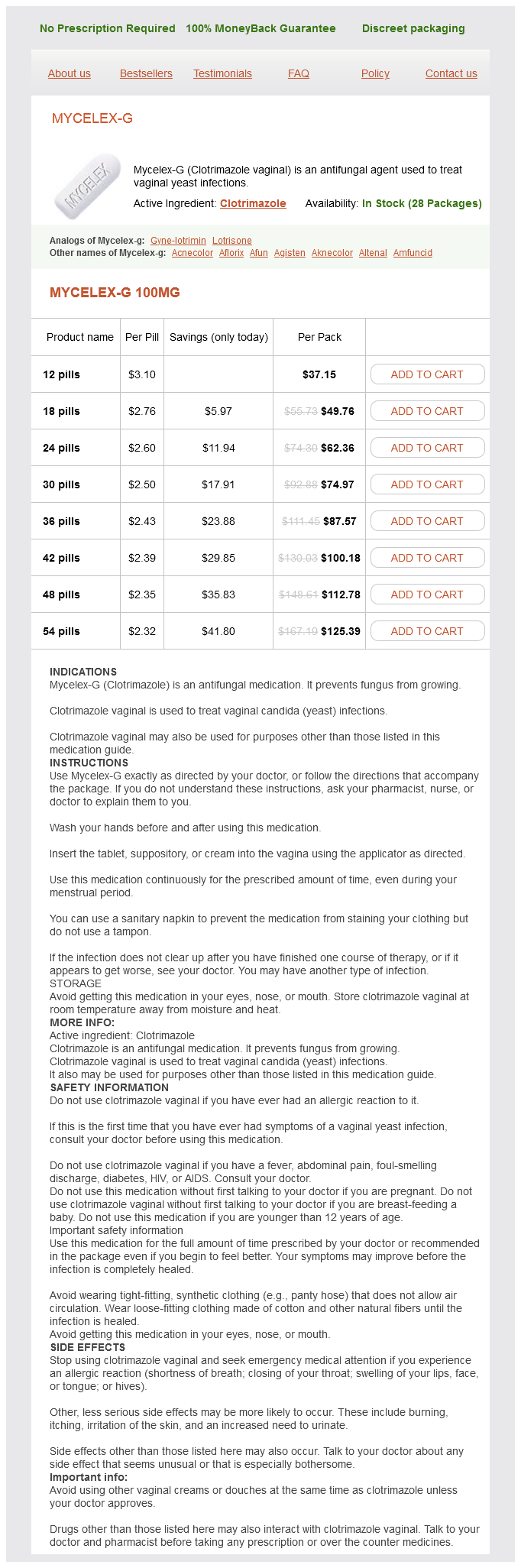
Mycelex-g Dosage and Price
Mycelex-g 100mg
- 12 pills - $37.15
- 18 pills - $49.76
- 24 pills - $62.36
- 30 pills - $74.97
- 36 pills - $87.57
- 42 pills - $100.18
- 48 pills - $112.78
- 54 pills - $125.39
Beta blockers can also produce hypoglycaemic unawareness because of their autonomic blockade antifungal oral medication order cheap mycelex-g. Only a minority of clinical trials with beta blockers report weight changes during treatment. In trials that do report weight changes, beta blockers are associated with a weight gain of. This may be attributed to the fact that beta blockade can decrease metabolic rate and also have other negative effects on energy metabolism. Obesity management in overweight hypertensive patients may therefore be more difficult in the presence of beta-blocker treatment. In black patients, efficacy of beta blockers in reducing systolic blood pressure is no different as compared to placebo and there are reports that beta blockers may even increase systolic blood pressure in these patients. Therefore, when beta-blocker therapy is not effective in reducing blood pressure, clinicians should discontinue therapy rather than increasing the drug dose. Pharmacodynamics of beta blockers in pregnant women is relatively well-studied, and serious maternal side effects are rare. Foetal pharmacodynamic and foetal side effects are less well known, and reports in the literature are sometimes contradictory. The safety of these agents, particularly atenolol and propranolol, is somewhat controversial because of individual reports of adverse effects on the foetus. A meta-analysis of 3 trials (480 women) comparing beta blockers with placebo or no beta blocker showed that beta-blocker therapy decreased the risk of severe hypertension and the need for additional antihypertensives. There was insufficient data for conclusions about the effect on perinatal mortality or preterm birth. Labetalol, a beta blocker that also has alpha-blocking properties, is a common second-line agent that is used. Beta blockers and their effect on quality of life the possible effects of beta blockers on various aspects of quality of life have been long debated, including an adverse impact on normal exercise capacity, cognitive function, sleep quality, overall mood, and sexual function (erectile failure in men and depressed libido in both sexes). Furthermore, there have been studies reporting impairment of memory function, particularly with the use of non-selective agents such as propranolol. Large-scale epidemiological studies also suggest a link between an increased use of antidepressant medications within 2 months of the prescription of a beta blocker, as compared to a reference group of patients treated for chronic diseases. However, such associations are frequently confounded and in one double blind, randomized, controlled cross-over study there appears to be no significant effect on cognitive function. Indeed, one placebo-controlled trial in 32 hypertensive patients suggested that propranolol causes no greater impairment of cognitive function than placebo. Beta-blocker therapy could be implicated in sexual dysfunction, both by vasodilator effects on male erection and more generally by decreased libido. There have been several cross-over studies reporting reduction of sexual activity in hypertensive men on treatment with beta blockers compared to active controls such as lisinopril or valsartan. Unfortunately, these frequently do not define the mechanical or psychosexual nature of the dysfunction. Nebivolol is a third-generation lipophilic beta blocker with distinct beta- selective and vasodilating properties. It also appears to have antioxidant properties, and studies have shown that it causes greater central aortic pressure reductions than atenolol in human subjects. The pharmocological profile is characterized by the significant antihypertensive effect as well as lowering of cardiac preload and afterload. These effects suggest that nebivolol may be beneficial in heart failure patients as well. In general, nebivolol is well tolerated and does not appear to significantly influence glucose or plasma lipid metabolism and this also is a major breakthrough in comparison with the older beta blockers. They should be used with caution in severe decompensated heart failure, in peripheral vascular disease and in patients with poorly controlled insulin dependent diabetes. They should also be used cautiously in patients suspected to have a phaeochromocytoma as unopposed alpha-adrenergic agonist action may lead to a serious hypertensive crisis. How strong is the evidence for use of beta-blockers as first-line therapy for hypertension? Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? Introduction Calcium-channel blockers have been a useful tool in the management of hypertension for many years. The term was first used by Fleckenstein in 969 to describe a compound which was both negatively inotropic and a coronary vasodilator. Verapamil was one of the very first calcium-channel blockers introduced but since then there have been several other agents with similar pharmacological modes of action. Unlike beta-adrenoceptor blockers, however, calcium-channel blockers do not share a common molecular structure. Conversely, reduction in the amount of intracellular calcium reduces myocardial contractility as well as inducing peripheral and coronary vasodilatation. Although all calcium-channel blockers by their very nature share the common property of inhibiting cellular calcium influx, they possess differing effects on vascular smooth muscle, cardiac myocytes, and the cardiac conductive tissue. Essentially, a calcium-channel blocker acts by inhibiting the cellular entry of calcium through voltage-dependent L- and T-type calcium channels. Despite sharing a common mechanism of action, the available agents possess differing molecular structure and site of binding. Three classes of agents have been identified: dihydropyridines (nifedipine and amlodipine), benzothiazepine (diltiazem), and phenylalkylamine (verapamil). Calcium-channel blockers thus possess chemical and pharmacological heterogeneity and are capable of blocking calcium channels in differing locations with varying degrees of intensity.