Nemasole
General Information about Nemasole
Nemasole is a extensively used drug within the medical subject for treating intestinal parasitic infections. It falls beneath the class of anthelmintic drugs, which are used to kill and remove parasitic worms from the body. Nemasole is known for its broad-spectrum action in opposition to varied types of worms and has been discovered to be significantly effective towards enterobiasis and trichuriasis.
One of the ways in which Nemasole works is by depleting the glycogen stores in the tissues of the worms. Glycogen is a form of glucose that is stored within the liver and muscle tissue. It is the main source of energy for many organisms, together with parasites. Nemasole interferes with the enzymes concerned in the breakdown of glycogen, resulting in its depletion in the tissues of the worms. This, in flip, impacts the energy metabolism of the worms, making them weak and eventually causing their dying.
Apart from these two primary actions, Nemasole additionally inhibits the synthesis of ATP (adenosine triphosphate) in parasitic worms. ATP is the primary supply of power for cellular processes, and without it, the worms cannot survive. By inhibiting ATP synthesis, Nemasole successfully cuts off the vitality provide of the worms, resulting in their demise.
In conclusion, Nemasole is a potent anthelmintic drug that has proven to be extremely effective towards enterobiasis and trichuriasis. Its ability to disrupt the glucose utilization course of, deplete glycogen shops, inhibit tubulin synthesis, and ATP synthesis makes it a formidable weapon in opposition to parasitic worms. With its broad-spectrum motion and minimal side effects, Nemasole continues to be the go-to drug for treating numerous kinds of worm infections.
The major mechanism of action of Nemasole is its capability to disrupt the conventional glucose utilization course of in parasitic worms, leading to their demise. This is achieved by two main actions - depletion of glycogen stores in the tissues of the worms and inhibition of the synthesis of mobile tubulin. Let us delve deeper into the small print of how Nemasole exerts its effect on these tiny undesirable creatures.
Another major mechanism of motion of Nemasole is the inhibition of the synthesis of cellular tubulin. Tubulin is an essential protein that makes up the cytoskeleton of cells, offering structure and stability. In parasitic worms, tubulin is concerned in cell division and growth. Nemasole disrupts the synthesis of tubulin, resulting in the formation of abnormal cells and inhibition of worm development. This ultimately leads to the demise of the worms.
One of the significant advantages of utilizing Nemasole is its broad-spectrum action towards varied kinds of worms. This signifies that it's efficient towards a variety of parasites, making it a preferred alternative for treating parasitic infections. Moreover, Nemasole can additionally be secure and well-tolerated by most sufferers, with minimal unwanted effects reported.
Nemasole is thought to have a excessive effectiveness price in opposition to enterobiasis, also referred to as pinworm an infection. This infection is the most common kind of worm infection in humans and is attributable to a tiny worm called Enterobius vermicularis. The symptoms of enterobiasis embody itching around the anus, stomach ache, and discomfort. Nemasole can additionally be highly efficient towards trichuriasis, a type of an infection brought on by the whipworm, Trichuris trichiura. Whipworm infections may cause severe diarrhea, stomach ache, and anemia in some instances.
However, like some other treatment, Nemasole also has its limitations. It is not effective against all kinds of worm infections and will not work for certain individuals. Additionally, it's essential to seek the assistance of a doctor earlier than taking Nemasole and follow the prescribed dosage to avoid any adverse effects.
In most patients who survive an infarction or the initial 36-month period of frequent episodes herpes zoster antiviral drugs nemasole 100 mg online, the condition stabilizes, and there is a tendency for symptoms and cardiac events to diminish with time. Mortality is approximately fourfold higher in elderly patients (>75 years) in comparison with younger patients. Following disruption of a vulnerable plaque, patients experience ischemic discomfort resulting from a reduction of flow through the affected epicardial coronary artery. The flow reduction may be caused by a completely occlusive thrombus (right) or subtotally occlusive thrombus (left). Once converted to its functional state, this receptor develops a high affinity for amino acid sequences on soluble adhesive proteins. Since fibrinogen is a multivalent molecule, it can bind to two different platelets simultaneously, resulting in platelet cross-linking and aggregation. Fluid-phase and clot-bound thrombin participate in an autoamplification reaction leading to further activation of the coagulation cascade. The culprit coronary artery eventually becomes occluded by a thrombus containing platelet aggregates and fibrin strands. The amount of myocardial damage caused by coronary occlusion depends on (1) the territory supplied by the affected vessel; (2) whether or not the vessel becomes totally occluded; (3) the duration of coronary occlusion; (4) the quantity of blood supplied by collateral vessels to the affected tissue; (5) the demand for oxygen of the myocardium whose blood supply has been suddenly limited; (6) native factors that can produce early spontaneous lysis of the occlusive thrombus; and (7) the adequacy of myocardial perfusion in the infarct zone when flow is restored in the occluded epicardial coronary artery. A mural thrombus forms at the site of plaque disruption, and the involved coronary artery becomes occluded. After agonist stimulation of platelets, thromboxane A2 (a potent local vasoconstrictor) is released, further platelet activation occurs, and potential resistance to fibrinolysis develops. The pain is deep and visceral; adjectives commonly used to describe it are heavy, squeezing, and crushing, although occasionally it is described as stabbing or burning (Chap. Typically the pain involves the central portion of the chest and/or the epigastrium, and on occasion it radiates to the arms. The pain may commence when the patient is at rest, but when it begins during a period of exertion, it does not usually subside with cessation of activity, in contrast to angina pectoris. A transient midsystolic or late systolic apical systolic murmur due to dysfunction of the mitral valve apparatus may be present. The arterial pressure is variable; in most patients with transmural infarction, systolic pressure declines by 1015 mmHg from the preinfarction state. However, Q waves in the leads overlying the infarct zone may vary in magnitude and even appear only transiently, depending on the reperfusion status of the ischemic myocardium and restoration of transmembrane potentials over time. The precordium is usually quiet, and the apical impulse may be difficult to palpate. In patients with anterior wall infarction, an abnormal systolic pulsation caused by dyskinetic bulging of infarcted myocardium may develop in the periapical area within the first days of the illness and then may resolve. The rate of liberation of specific proteins differs depending on their intracellular location, their molecular weight, and the local blood and lymphatic flow. Cardiac biomarkers become detectable in the peripheral blood once the capacity of the cardiac lymphatics to clear the interstitium of the infarct zone is exceeded and spillover into the venous circulation occurs. Cardiac-specific troponin T (cTnT) and cardiac-specific troponin I (cTnI) have amino acid sequences different from those of the skeletal muscle forms of these proteins. While it has long been recognized that the total quantity of protein released correlates with the size of the infarct, the peak protein concentration correlates only weakly with infarct size. The nonspecific reaction to myocardial injury is associated with polymorphonuclear leukocytosis, which appears within a few hours after the onset of pain and persists for 37 days; the white blood cell count often reaches levels of 12,00015,000/µL. The erythrocyte sedimentation rate rises more slowly than the white blood cell count, peaking during the first week and sometimes remaining elevated for 1 or 2 weeks. However, these imaging modalities are used less often than echocardiography because they are more cumbersome and lack sensitivity and specificity in many clinical circumstances. Myocardial perfusion imaging with 201Tl or 99mTc-sestamibi, which are distributed in proportion to myocardial blood flow and concentrated by viable myocardium (Chap. Myocardial infarction can be detected accurately with high-resolution cardiac magnetic resonance imaging (Chap. This delay can best be reduced by health care professionals educating the public concerning the significance of chest discomfort and the importance of seeking early medical attention. Increasingly, monitoring and treatment are carried out by trained personnel in the ambulance, further shortening the time between the onset of the infarction and appropriate treatment. Plotted sequentially from left to right are shown the times for patients to recognize symptoms and seek medical attention, transportation to the hospital, in-hospital decisionmaking, implementation of reperfusion strategy, and restoration of flow once the reperfusion strategy has been initiated. The time to initiate fibrinolytic therapy is the "door-to-needle" (D-N) time; this is followed by the period of time required for pharmacologic restoration of flow. At the bottom are shown a variety of methods for speeding the time to reperfusion along with the goals for the time intervals for the various components of the time delay. Rapid inhibition of cyclooxygenase-1 in platelets followed by a reduction of thromboxane A2 levels is achieved by buccal absorption of a chewed 160325 mg tablet in the emergency department. This measure should be followed by daily oral administration of aspirin in a dose of 75162 mg. However, when hypoxemia is present, O2 should be administered by nasal prongs or face mask (24 L/min) for the first 612 h after infarction; the patient should then be reassessed to determine if there is a continued need for such treatment. Nitrates should not be administered to patients who have taken the phosphodiesterase-5 inhibitor sildenafil for erectile dysfunction within the preceding 24 h since it may potentiate the hypotensive effects of nitrates. These hemodynamic disturbances usually respond promptly to elevation of the legs, but in some patients volume expansion with intravenous saline is required. The patient may experience diaphoresis and nausea, but these events usually pass and are replaced by a feeling of well-being associated with the relief of pain. Morphine also has a vagotonic effect and may cause bradycardia or advanced degrees of heart block, particularly in patients with posteroinferior infarction.
It presents with unilateral proptosis and hyperaemia and oedema of the conjunctiva of the affected eye hiv timeline of infection nemasole 100 mg on line. Treatment is by occlusion of the fistula with balloons, coils or glue through a catheter passed up the carotid artery. Anosmia (loss of sense of smell) is common after basal fractures of the anterior cranial fossa and is untreatable. Headache, irritability and lack of attention are common after all serious head injuries but tend to improve with time. Post-traumatic stress disorder with depression and anxiety is often diagnosed but difficult to prove. Neurodisability occurs in many patients with severe brain injuries and requires prolonged treatment in Physiotherapy and Occupational Therapy Departments, preferably dedicated to head-injured patients. Many may require long-term care at home or need to be looked after permanently in facilities for the chronically disabled. Conscious patients without neck symptoms have never been found to have an unstable cervical spine or have subsequently progressed to develop neurological deterioration. It is, therefore, unnecessary to go to great lengths to maintain spinal cord protection in a conscious patient who has not had a head injury and does not complain of neck pain. There is no need for further investigations if all neck movements are full and pain-free and there are no neurological signs in the limbs. Difficulties arise in the unconscious patient, especially if they are intubated and ventilated. In these circumstances the management options include: Maxillofacial trauma is often associated with airway problems, haemorrhage, neck and head injuries, and fractures of the mandible, maxilla, zygoma, nasal bones and orbit. Investigation Clinical diagnostic routines When examining the skull, eye and orbit: inspect and palpate the cranium palpate the orbital margins test visual acuity examine the eyelids note the pupil size inspect the corneae and anterior chamber test the red reflex check for diplopia and eye movements test for infra-orbital nerve paraesthesia. When examining the nose check for: Treat the cervical spine as if it is unstable until the patient regains full consciousness. Carry out dynamic flexion and extension cervical spine X-rays using an image intensifier. When examining the Zygoma (cheek) check for: the spine should be considered unstable if both the anterior and posterior columns have been disrupted. Displaced unstable injuries are treated by halo traction until surgical stabilization can be undertaken (see Chapter 10). Nasal X-rays, plain X-rays and orthopantomographs are required for fractures of the nose and mandible. Angiography may be used to diagnose and manage major bleeding by therapeutic embolization of the external carotid artery or its branches. Undisplaced fractures of the angle or body of the mandible are treated conservatively if there is no mobility or malocclusion but, if these are present, open reduction and fixation by microplates is indicated. The orbit can be reached through the conjunctiva and fractures of the upper maxilla and zygoma can be dealt with through incisions made above the hairline. Undisplaced maxillary fractures these can be treated Airway obstruction at the time of injury or by an acutely deviated nasal septum. Growth retardation and deformity can follow condylar fractures of the mandible in children and the condyle may fuse with the temporal bone, making it impossible to open the jaw. If a broken tooth is found, a chest X-ray should be considered as it might have been inhaled. Displaced fractures require open reduction and internal fixation with microplates. All deep neck wounds used to be explored but this approach has been challenged in recent years with improved imaging and endoscopy. The mandible can be immobilized with mandibulomaxillary wires if there is evidence of malocclusion. For simplicity, it is easier to consider both separately but it must be remembered that the pleura extends above the clavicle and that the lower chest and upper abdomen overlap. At the very least, this allows a tamponade to be released, a cardiac puncture to be closed, cardiac massage to be carried out and a clamp put on the aorta or the hilum of the lung, although few patients survive these heroic manoeuvres. Imaging An erect chest X-ray should be taken, with additional rib views if there are areas of local tenderness, to confirm the diagnosis. It is important to carry out the chest X-ray with the patient in the erect position, if possible, to detect a small pneumothorax at the apex and, more importantly, a moderate or even large haemothorax at the base of the chest cavity, which can be missed if the patient is lying down. Oral or intramuscular analgesics may be supplemented by local infiltration around the origins of the intercostal nerves, just below the fractures, with a long-acting local anaesthetic agent such as marcaine 0. When a number of adjacent ribs are fractured in two places, the segment between the breaks is sucked in during inspiration and pushed outwards during expiration. Blood gas monitoring, repeated chest radiographs and physiotherapy with appropriate analgesia should be instituted. In many cases conservative management with pain relief (see above), supplemental oxygen, physiotherapy and careful monitoring is sufficient, but intubation and ventilation may become indicated if the patient shows signs of increasing respiratory distress and respiratory failure (reduced oxygen saturation). The prognosis of rib fractures depends upon the associated intrathoracic injuries. Investigation Clinical diagnostic indicators Patients with a simple large closed pneumothorax present with difficulty in breathing and the physical signs of a collapsed lung no or reduced air entry and hyper-resonance to percussion. A tension pneumothorax causes respiratory distress, Small pneumothoraces with no signs of impaired oxygenation (normal blood gas saturations) can be treated by observation plus analgesia for any associated rib fracture, physiotherapy and blood gas saturation monitoring. A thoracostomy tube should be inserted if there are signs of respiratory distress. Tension pneumothoraces must be treated urgently by the immediate insertion of a tube to Lung contusion (direct injury) 135 relieve the tension.
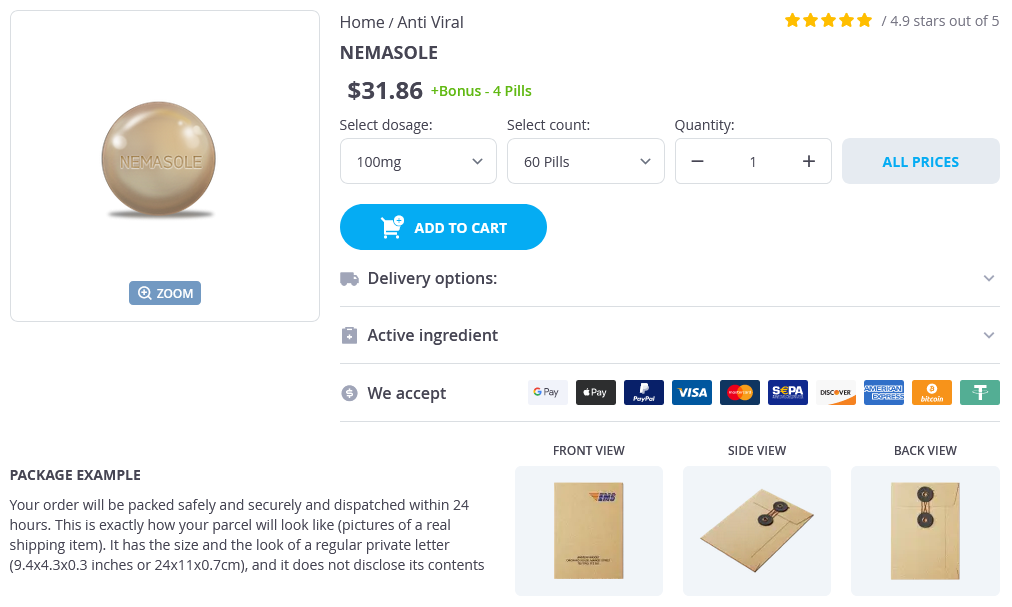
Nemasole Dosage and Price
Nemasole 100mg
- 60 pills - $35.40
- 90 pills - $46.73
- 120 pills - $58.06
- 180 pills - $80.71
- 270 pills - $114.70
- 360 pills - $148.68
Stable angina pectoris is characterized by chest or arm discomfort that may not be described as pain but is reproducibly associated with physical exertion or stress and is relieved within 510 min by rest and/or sublingual nitroglycerin (Chaps hiv infection versus aids cheap nemasole 100 mg without prescription. The "culprit lesion" on angiography may show an eccentric stenosis with scalloped or overhanging edges and a narrow neck. Typical pathways begin with assessment of the likelihood that the presenting symptoms are due to ischemia. If the patient remains painfree and the markers are negative, the patient may go on to stress testing. Anginal "equivalents" such as dyspnea and epigastric discomfort may also occur, and these appear to occur more often in women. T-wave changes are sensitive for ischemia but less specific, unless they are new, deep T-wave inversions (0. There is a direct relationship between the degree of troponin elevation and mortality. However, in patients without a clear clinical history of myocardial ischemia, minor troponin elevations have been reported and can be caused by congestive heart failure, myocarditis, sestamibi or thallium imaging can reduce unnecessary hospitalizations by excluding acute ischemia. If the patient has negative markers and no recurrence of pain, he/she is sent for exercise treadmill testing, with imaging reserved for patients with abnormal baseline electrocardiograms. If positive, the patient is admitted; if negative, the patient is discharged, with follow-up to his/her primary physician. Other risk factors include diabetes mellitus, left ventricular dysfunction, and elevated levels of creatinine, atrial natriuretic peptides, and C-reactive protein. Medical therapy involves simultaneous anti-ischemic treatment and antithrombotic treatment. If pain persists after three doses given 5 min apart, intravenous nitroglycerin (510 µg/min using nonabsorbing tubing) is recommended. The rate of the infusion may be increased by 10 µg/min every 35 min until symptoms are relieved or systolic arterial pressure falls to <100 mmHg. The only absolute contraindications to the use of nitrates are hypotension or the use of sildenafil (Viagra) or other drugs in that class within the previous 24 h. Intravenous beta blockade followed by oral beta blockade targeted to a heart rate of 5060 beats/min is recommended. If pain persists despite intravenous nitroglycerin and beta blockade, morphine sulfate, 15 mg intravenously, can be administered every 530 min as needed. The typical initial dose is 325 mg daily, with lower doses (75162 mg daily) recommended for long-term therapy. No clear guidelines are available regarding evaluation or treatment, but the use of higher doses of aspirin and/or a thienopyridine (clopidogrel) appears to be logical in this situation. Four options are available for anticoagulation therapy to be added to aspirin and clopidogrel. The Factor Xa inhibitor fondaparinux is equivalent for early efficacy compared with enoxaparin but appears to have a lower risk of major bleeding and thus may have the best benefit risk ratio. For "upstream" management of high-risk patients in whom an invasive management is intended. Choice of the specific agent is not as important as ensuring that appropriate candidates receive this therapy. If there are concerns about patient intolerance owing to existing pulmonary disease, especially asthma, left ventricular dysfunction, risk of hypotension or severe bradycardia, initial selection should favor a short-acting agent, such as propranolol or metoprolol or the ultra-short-acting agent esmolol. Mild wheezing or a history of chronic obstructive pulmonary disease should prompt a trial of a short-acting agent at a reduced dose. Note: Several recommendations in this guide suggest the use of agents for purposes or in doses other than those specified by the U. Such recommendations are made after consideration of concerns regarding nonapproved indications. Where made such recommendations are based on more recent clinical trials or expert consensus. As with all antithrombotic agents, bleeding is the most important adverse effect of antiplatelet drugs, especially their combination. Thus, patients with a history of bleeding must be screened carefully and given fewer antithrombotic agents. Thus, a multifactorial approach to long-term medical therapy is directed at preventing the various components of atherothrombosis. The syndrome is due to focal spasm of an epicardial coronary artery, leading to severe myocardial ischemia. The exact cause of the spasm is not well defined, but it may be related to hypercontractility of vascular smooth muscle due to vasoconstrictor mitogens, leukotrienes, or serotonin. The anginal discomfort is often extremely severe and has usually not progressed from a period of chronic stable angina. Atherosclerotic plaques, which do not usually cause critical obstruction, in at least one proximal coronary artery occur in the majority of patients, and in them spasm usually occurs within 1 cm of the plaque. Risk factor modification is key, and the physician should discuss with the patient the importance of smoking cessation, achieving optimal weight, daily exercise following an appropriate diet, blood pressure control, tight control of hyperglycemia (for diabetic patients), and lipid management, as recommended for patients with chronic stable angina (Chap. There is evidence of benefit with long-term therapy with five classes of drugs that are directed at different components of the atherothrombotic process. Antiplatelet therapy, now recommended to be the combination of aspirin and 394 vasoconstrictor medications, and hyperventilation have been used to provoke and demonstrate focal coronary stenosis to establish the diagnosis. Philadelphia, Saunders, 2010 - et al: Intensive versus moderate lipid lowering with statins after acute coronary syndromes.