Orlistat
General Information about Orlistat
In conclusion, Orlistat is a lipase inhibitor that helps people with obesity or weight-related situations to shed weight and maintain it off. It is an efficient weight reduction software that works by blocking the absorption of dietary fat, increasing satiety, and affecting hormones that regulate urge for food. While it may come with some side effects, these may be managed by following a low-fat diet. With the correct steerage and life-style modifications, Orlistat is normally a beneficial option for people seeking to obtain and maintain a wholesome weight.
The main means during which Orlistat helps with weight loss is by lowering the amount of dietary fat absorbed by the body. On average, it blocks round 30% of the fat consumed in a meal, which then passes by way of the body without being absorbed. This results in a lower in calorie intake and a rise in weight reduction.
Orlistat, also referred to as tetrahydrolipstatin, is a medication that's used for weight reduction. It is a lipase inhibitor, that means that it works by blocking the enzyme lipase, which is liable for breaking down fat in the gut. This results in the prevention of fats absorption by the body, permitting for weight reduction.
As with any medicine, Orlistat does come with potential unwanted effects. The commonest unwanted effects embody belly ache, oily stools, and diarrhea. These may be managed by following a low-fat food regimen, as recommended by the treatment. Other much less frequent unwanted effects embody headache, flatulence, and low blood sugar in individuals with diabetes.
Orlistat was initially accredited by the US Food and Drug Administration (FDA) in 1999 for long-term use in people with obesity. It is available in both prescription and over-the-counter (OTC) types. The prescription kind, generally generally identified as Xenical, is taken 3 times a day with meals, whereas the OTC version, generally recognized as Alli, is taken with every meal containing fat, as much as 3 times a day.
Orlistat just isn't a magic pill for weight reduction, and it may be very important perceive that it works greatest when combined with healthy lifestyle habits similar to a balanced diet and common exercise. It can be important to notice that it is most effective when used in individuals with a body mass index (BMI) of 30 or above, or a BMI of 27 or above with weight-related well being circumstances.
Numerous research have proven that Orlistat is an effective weight loss device. In a 2013 analysis of 11 medical trials, it was discovered that individuals taking Orlistat lost on average 2.9 kg (6.4 pounds) more weight than these on a placebo over the course of a yr. In addition, it has been proven to have a optimistic effect on different weight-related health points, similar to hypertension, sort 2 diabetes, and excessive ldl cholesterol.
Besides its effect on fat absorption, Orlistat additionally helps with weight loss in two different ways. Firstly, it will increase satiety, making people feel full and reducing the desire to overeat. Secondly, it has been shown to increase the discharge of a hormone referred to as glucagon-like peptide 1 (GLP-1), which performs a role in regulating appetite.
It is essential to consult with a healthcare professional before beginning Orlistat, as it might interact with different drugs similar to blood thinners and thyroid medication. It must also be avoided throughout pregnancy and while breastfeeding.
Similar functional results and complications after ileal pouch-anal anastomosis in patients with indeterminate vs ulcerative colitis weight loss 30 day challenge purchase orlistat with mastercard. Effect of infliximab on short-term complications in patients undergoing operation for chronic ulcerative colitis. Infliximab in ulcerative colitis is associated with an increased risk of postoperative complications after restorative proctocolectomy. Systematic review and meta-analysis: vedolizumab and postoperative complications in inflammatory bowel disease. The effect of biologics on postoperative complications in children with inflammatory bowel disease and bowel resection. Total laparoscopic proctocolectomy and laparoscopy assisted proctocolectomy for inflammatory bowel disease: operative technique and preliminary report. Laparoscopic-assisted versus open ileal pouch-anal anastomosis: functional outcome in a case-match series. Safety, feasibility, and short-term outcomes of laparoscopic ileal-pouch-anal anastomosis: a single institutional case-matched experience. Dysplasia of the anal transitional zone after ileal pouch-anal anastomosis: results of prospective evaluation after a minimum of ten years. Laparoscopic ileal pouch-anal anastomosis in patients with chronic ulcerative colitis and primary sclerosing cholangitis: a case-matched study. Robotic-assisted surgery for low rectal dissection: from better views to better outcome. Randomized clinical trial comparing loop ileostomy and loop transverse colostomy for faecal diversion following total mesorectal excision. Sclerotherapy for massive enterostomy bleeding resulting from portal hypertension. Effect of systemic steroids on ileal pouch-anal anastomosis in patients with ulcerative colitis. A prospective evaluation of the long-term outcome of ileal pouch-anal anastomosis in patients with inflammatory bowel disease-unclassified and indeterminate colitis. Pouchitis and extraintestinal manifestations of inflammatory bowel disease after ileal pouch-anal anastomosis. Predictors of pouchitis after ileal pouch-anal anastomosis: a retrospective review. Pouchitis after ileal pouchanal anastomosis for ulcerative colitis occurs with increased frequency in patients with associated primary sclerosing cholangitis. Serologic responses in indeterminate colitis patient before ileal-pouch-anal anastomosis may determine those at risk for continuous pouch inflammation. Factors associated with disease activity of pouchitis after surgery for ulcerative colitis. Comprehensive evaluation of inflammatory and non-inflammatory sequelae of ileal pouch-anal anastomosis. Irritable pouch syndrome: a new category of diagnosis for symptomatic patients with ileal pouch-anal anastomosis. Long-term histomorphological surveillance of the pelvic ileal pouch: dysplasia develops in a subgroup of patients. Early transcriptomic changes in the ileal pouch provide insight into the molecular pathogenesis of pouchitis and ulcerative colitis. The colonic epithelium in chronic ulcerative colitis-An energy deficiency disease Pouchitis, similar to active ulcerative colitis, is associated with impaired butyrate oxidation by intestinal mucosa. Ileal pouch-anal anastomosis for chronic ulcerative colitis: complications and long-term outcome in 1310 patients. Four-week open-label trial of metronidazole and ciprofloxacin for the treatment of recurrent or refractory pouchitis. Efficacy of infliximab rescue therapy in patients with chronic refractory pouchitis: a multicenter study. Efficacy of adalimumab rescue therapy in patients with chronic refractory pouchitis previously treated with infliximab: a case series. Preservation of the anal transition zone in ulcerative colitis: long-term effects on defecatory function. Review article: the incidence and prevalence of colorectal cancer in inflammatory bowel disease. Quality of life after indefinite diversion/pouch excision in ileal pouch failure patients. A prospective evaluation of sexual function and quality of life after ileal pouch-anal anastomosis. Sexual function, body image, and quality of life after laparoscopic and open ileal pouchanal anastomosis. The effect of ageing on function and quality of life in ileal pouch patients: a single cohort experience of 409 patients with chronic ulcerative colitis. Three hundred cases of diffuse chronic ulcerative colitis treated by total colectomy and ileo-rectal anastomosis. Total abdominal colectomy and ileorectal anastomosis for inflammatory bowel disease. Long-term results of ileorectal anastomosis in ulcerative colitis in Stockholm County.
The criteria of Wilson and Jungner (1968) for an implementation to newborn screening include: (1) reliable disease detection in a presymptomatic state of the disease weight loss journey order cheapest orlistat and orlistat, (2) treatability of the disease, and (3) the start of treatment in the presymptomatic children. Additional inborn errors such as maple syrup urine disease, galactosaemia, congenital hypothyroidism, and biotinidase deficiency were incorporated into newborn screening programmes of some countries. However, each novel candidate disease has to be evaluated with respect to whether this disease fulfils the criteria for a disease to be screened (see Chapters 2. As a consequence, the number of screened inborn errors of metabolism varies considerably ranging from two disorders (United Kingdom, Switzerland) up to more than 50 disorders (some parts of the United States of America). Notably, the United States screening panel also includes conditions that can be regarded as nondiseases or have at least a doubtful pathological meaning, such as the 3-methylcrotonyl CoA carboxylase deficiency. It should be appreciated that a liberal expansion of the screening panel burdens the healthcare system, the affected individuals, and the increasing number of false-positive individuals and their families. Given these difficulties, it is to be hoped that screening politics will become harmonized in a joint international effort. Aetiology, genetics, pathogenesis, and pathology the clinical manifestations of most protein-dependent inborn errors are thought to result from toxicity of the accumulating key metabolites to specific organs inducing selective or multiple organ failure. Despite increasing knowledge of pathophysiology, the most relevant concepts are derived from clinical research. A block in the next step of the pathway, 4-hydroxyphenylpyruvate dioxygenase, results in alkaptonuria (ochronosis, arthritis, heart disease), whereas deficiency of the last enzyme, fumarylacetoacetase, produces a disease deadly in early childhood, tyrosinaemia type I, presenting with failure to thrive, liver failure, hepatosplenomegaly, hepatocarcinoma, and porphyria-like crises. The distinct syndromes resulting from defective breakdown of aromatic amino acids could never have been inferred simply by biochemical exploration of the metabolic pathway. Epidemiology As a group, protein-dependent disorders are by far the most common, acutely life-threatening inborn errors of metabolism (estimated prevalence >1:2000 newborns). However, reliable epidemiological data are scarce as all reports suggest a significant portion of patients who evade diagnosis and are considered to have neonatal sepsis or sudden infant death syndrome. Most epidemiological data are available from European countries, Japan, and the United States of America, highlighting variations based on ethnic background, migrations, and/or genetic isolation. In a few communities, the prevalence of individual disorders may increase up to five times the cumulative prevalence of amino acid and organic acid disorders in European countries, Japan, and the United States of America. For example, glutaric aciduria type I is found in up to 1 in 300 newborns in the Amish Community (United States of America) and the Oji-Cree First Nations (Canada), and in Qatar the prevalence of classic homocystinuria is 1 in 600 newborns. Clinical considerations and diagnostic work-up History A careful family history may reveal important clues to the diagnosis of protein-dependent inborn metabolic diseases. Most disorders are inherited as autosomal recessive traits which may be suspected if the parents are consanguineous or the family has a confined ethnic or geographic background. Carriers for particular disorders and affected children may be more frequent in certain communities Ashkenazi Jews, Arabic tribes), or countries that have seen little immigration over many centuries Often specialist investigations are started only after a second affected child is born into a family. Notably, the disease course of the same disorder may vary considerably even within families depending on genotypephenotype correlation (if any), varying X-inactivation in female carriers As a result of the successful treatment of inborn errors of metabolism, an increasing number of affected women are reaching reproductive age. If they become pregnant, there may be a risk for their fetuses to be harmed by toxic metabolites from the mother. Here we focus on the clinical manifestation and differential diagnosis of disorders presenting with acute metabolic decompensations (Boxes 12. There is only a limited repertoire of pathophysiological sequences in the response to metabolic intoxication and, consequently, a limited Box 12. Timely and correct intervention during the initial episode is a critical prognostic factor. Many protein-dependent metabolic errors already manifest in the first days of life with progressive irritability or drowsiness. Most typically, a young infant may vomit or refuse to feed and then rapidly deteriorates. The initial erroneous diagnoses are usually neonatal sepsis or intracranial haemorrhage: a presumptive diagnosis of a protein-dependent inborn error should be considered with equal priority. Children with milder forms may be repeatedly admitted, for example, with unusual metabolic acidosis, hypoglycaemia, or neutropenia in the course of common infections especially gastroenteritis, before an inborn disorder of metabolism is considered, and routine clinical chemistry may be normal in between crises. A substantial number of patients with protein-dependent inborn errors of metabolism may present differently with acute encephalopathy or chronic and fluctuating progressive neurological disease. Chronic subdural effusions, haematomas, and retinal haemorrhages in infants and toddlers are characteristic findings in glutaric aciduria type I, although they are more commonly due to child abuse. Laboratory investigations the early consideration of metabolic diseases is of the utmost importance. Routine laboratory parameters Diagnostic clues can be obtained from routine laboratory investigations such as electrolytes (also required for the calculation of the anion gap), urinary ketones, serum transaminases, and creatine kinase. Any child admitted to an intensive care unit with lifethreatening nonsurgical illness should be tested for these parameters. Patients with genetic diseases that are prone to acute decompensations should carry an emergency card. Vaccinations should be carried out as recommended and should also include vaccinations against varicella, hepatitis A, pneumococcus, and influenza. Amino acid analysis Many metabolic parameters show considerable diurnal fluctuations. For example, plasma amino acid concentrations are highly dependent on the metabolic status, and standard samples should be obtained at least 4h postprandially. Regular amino acid analyses are required in patients on specific dietary treatments to adjust intake of amino acids and to recognize a deficiency of essential amino acids and micronutrients. For optimal results, it is important to separate plasma as soon as possible and to ship samples frozen on dry ice. Haemolysis or shipment of whole blood results in useless values for some amino acids.
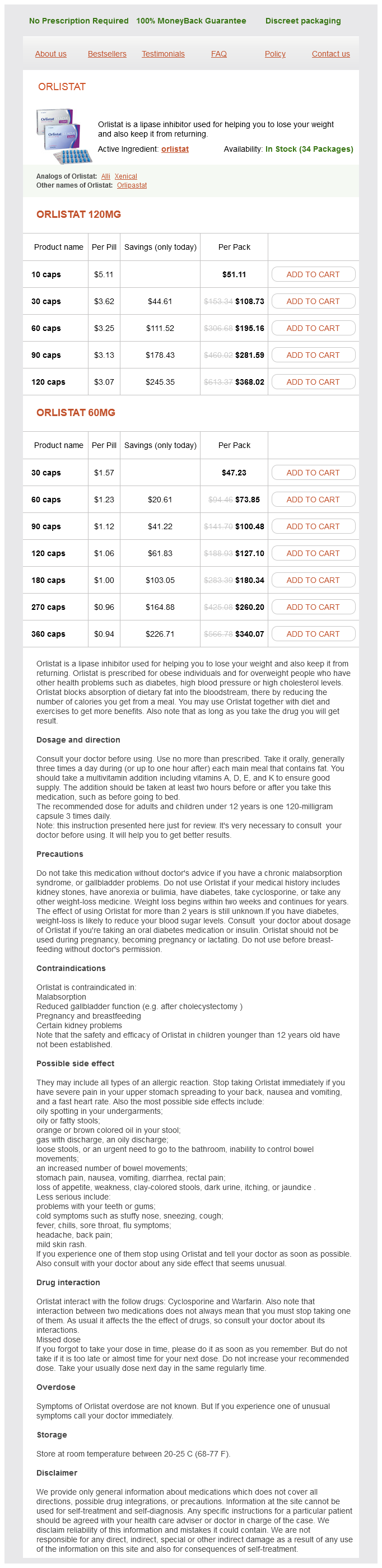
Orlistat Dosage and Price
Orlistat 120mg
- 10 caps - $51.11
- 30 caps - $108.73
- 60 caps - $195.16
- 90 caps - $281.59
- 120 caps - $368.02
Orlistat 60mg
- 30 caps - $47.23
- 60 caps - $73.85
- 90 caps - $100.48
- 120 caps - $127.10
- 180 caps - $180.34
- 270 caps - $260.20
- 360 caps - $340.07
In so doing weight loss pills similar to adderall cheap 120 mg orlistat with mastercard, a notation in the chart is made of the exact location of the opening of the papilla while the patient is awake, hydrated, and salivating. If no saliva is present, the patient can be given a salivary stimulant; a hard candy will suffice. The opening is then described in the electronic record to facilitate intubation in the future. The ease of visualization of the papilla opening of the awake patient is one of the reasons that some practitioners perform the procedure under a local anesthetic, in the office. The entire duct should be palpated after visualization and the gland should be examined with bimanual palpation to feel for stones as well as neoplasms, which will occasionally present with a longer history mimicking an inflammatory etiology. Patients with salivary gland pathology will often have abnormal characteristics of their saliva when viewed with the microscope. Patients with infection will have a very thick, purulent saliva; those with stones without infection will often have debris, and those with Sjögren and sialadenitis from I-131 will have very little saliva, and it is very thick. Size, shape, orientation, and location of stones should be noted, as these factors determine options for retrieval. Stones in the submandibular duct that are <4 mm in their maximum dimension are typically retrievable with a wire basket through an endoscope. The consensus is that most stones grow at about 1 mm per year1 and our own experience with several patients, who elected not to have extraction, bears this out. Stones become symptomatic when they either block the free flow of saliva (obstructive, meal-time symptoms) or when they get infected. While the development of infection with stones is relatively low, once it develops it can be hard to eradicate. Obstructive symptoms, on the other hand, may flare and abate over a period of years. The medical history should include asking about diabetes, dehydration, and xerostomia/xerophthalmia associated with Sjögren syndrome, as all are associated with stone formation. Sjögren patients may have intraglandular calcifications on imaging and most of these are not intraductal stones, but they may also have obstructive symptoms from intraductal stones as well. A history of radiation is important because of the secondary salivary effects of either radioactive iodine or external beam radiotherapy, even though neither is associated with stone formation. A combined procedure starts with endoscopic visualization and location of the stone followed by a standard external or intraoral approach to remove the stone, avoiding removal of the involved gland (see Chapter 18). Stone fragmentation using a laser (see Chapter 22), stone fragmentation using pneumatic lithotripsy (see Chapter 23), and extracorporeal lithotripsy (see Chapter 24) are other approaches that can be considered for stones not amenable to endoscopic wire basket retrieval alone. When there is a known sialolith, general anesthesia is chosen, unless there is a patient comorbidity that precludes it. Nasal intubation offers a wider exposure of the oral cavity, but there is a risk of epistaxis, and is traditionally reserved for bilateral cases or for patients with a challenging access to the oral cavity (obese patients, large tongue, small mouth opening, tori, or large teeth). Muscle relaxation is typically used for cases performed under general anesthesia for optimal intraoral access. A single intravenous dose of perioperative antibiotic to cover the oral flora is administered. The patient is positioned supine and the bed is rotated about 100 degrees, with a set-up similar to that of routine endoscopic sinus surgery. The right arm is tucked and the left armrest is positioned next to the bed to facilitate the surgeon and the assistant on opposite sides of the patient. Oval shape oriented along the length of the duct, free-flowing movement with irrigation, and a width no <4 mm were predictors for success. Palpable anterior floor of mouth stones or stones at the papilla may be removed transorally in the office without the need for endoscopy. Stones located elsewhere along the duct or that are not palpable are better served with endoscopic localization and retrieval using endoscopic or combined techniques. Indications for Surgery Sialendoscopy should be offered in all patients with submandibular sialolithiasis who have obstructive symptoms and/or recurrent acute sialadenitis with or without abscess formation. Asymptomatic patients with incidental sialoliths are offered endoscopy versus observation and counseled on the pros and cons of each. The pros of observation is the avoidance of surgical and anesthetic complications, and the cons include the future possibility of developing sialadenitis, neck abscess, and loss of the ability to retrieve the stone endoscopically as stone size increases over time. The only relative contraindication to interventional sialendoscopy is active sialadenitis due to an increased risk of ductal injury. Equipment There is a standard set of equipment in a custom interventional sialendoscopy set, to use for each case. A monopolar cautery with a Colorado tip is available, typically at a setting of 8. Disposable equipment includes: stone baskets, guidewires, indwelling access sheaths, 60 cc syringes with tubing, and local anesthetic. We prefer the "all-in-one" Marchal Miniature Endoscope for Diagnostic and Interventional Sialendoscopy with remote eyepiece, forward zero-degree telescope, semi-rigid, outer diameter of 1. The endoscope light strength is set very low, to about 10%, to allow optimum brightness while performing sialendoscopy; too much light causes reflection off the ductal wall and a virtual white out. The scope is focused and white balancing is done using a white gauze, while operating room lights overhead provide additional light. Intraoperative Technique Exposure is obtained using a mouth prop and sweetheart retractor. An injection or forceps are not routinely performed before securing the scope in the duct, in order to avoid creating pseudo-orifices that can mimic the true orifice. Doing so in an atraumatic fashion may be the most challenging portion of the procedure. Optimal exposure is attained with a mouth prop and the assistant retracts the tongue posteriorly using a sweetheart retractor. Application of methylene blue to help make the papilla more prominent can be used if necessary.