Pantoprazole
General Information about Pantoprazole
GERD, also referred to as acid reflux disease disease, is a situation during which the abdomen acid flows back into the esophagus. This causes a selection of symptoms together with heartburn, chest pain, and problem swallowing. If left untreated, GERD can lead to extra severe issues similar to esophageal ulcers, strictures, and even esophageal cancer. Pantoprazole helps to alleviate these symptoms and stop these issues by decreasing the quantity of acid within the stomach.
In conclusion, Pantoprazole is a broadly prescribed medicine that helps to lower the amount of acid produced within the abdomen. It is an efficient remedy for circumstances associated to excessive stomach acid, such as GERD and erosive esophagitis. With proper use and monitoring by a healthcare skilled, Protonix can present reduction to sufferers and prevent long-term problems. However, like all treatment, it ought to be taken with warning and beneath the guidance of a doctor.
Pantoprazole is usually well tolerated by most patients, with widespread unwanted effects being delicate and momentary. These could include headache, diarrhea, nausea, and abdomen ache. However, as with all medicine, there is a risk of rare however severe side effects, corresponding to liver damage, bone fractures, and infections. It is important to inform your doctor if you expertise any uncommon signs while taking Protonix.
Pantoprazole is particularly effective in healing erosive esophagitis, a situation in which the liner of the esophagus turns into infected and damaged as a outcome of persistent publicity to abdomen acid. This can occur as a end result of untreated GERD or other components such as smoking, weight problems, or being pregnant. Erosive esophagitis may cause severe pain and discomfort, leading to difficulty swallowing and significant impairment of daily actions. Pantoprazole helps to heal the broken mucous membrane of the esophagus by suppressing acid production.
It can be important to note that Pantoprazole might interact with different drugs. It is crucial to tell your doctor about some other drugs you're taking, together with over-the-counter medication and herbal supplements, to avoid potential interactions.
Pantoprazole, additionally known by its model name Protonix, is a medication that is generally used to deal with situations associated to the abdomen and esophagus. It belongs to a class of drugs referred to as proton pump inhibitors (PPIs), which work by reducing the amount of acid produced in the abdomen. Pantoprazole is prescribed to patients that suffer from acid-related conditions corresponding to gastroesophageal reflux disease (GERD) and erosive esophagitis.
Protonix is on the market as a tablet or an oral suspension and is usually taken as quickly as a day, preferably before a meal. It is necessary to follow the prescribed dosage and duration of treatment to see the full benefits of the medication. Depending on the severity of the condition, treatment with Protonix can final from a few weeks to several months.
Protonix shouldn't be used for instant aid of heartburn signs. It isn't meant to be a rescue medicine and should take a few days to show its full effect. For quick relief of heartburn symptoms, antacids or H2 blockers may be more appropriate.
Scrapings of seborrhea have revealed Malassezia furfur (Pityrosporum ovale) gastritis nerviosa best order for pantoprazole, implying that the seborrhea is caused by this fungus. Consistent with the isolation of this fungus is the clinical finding that seb orrhea responds well to topical clotrimazole (1 % cream) as well as hydrocortisone (1 % cream). Patients with primary central ner vous system lymphoma are treated with radiation. Treat ment is with emollients (eg, absorption base cream) and antipruritic lotions (eg, camphor 9. Epidemiologic studies have shown that between 1 973 and 1987 among single men in San Francisco, the risk of Kaposi sarcoma increased more than 5000-fold and the risk of non-Hodgkin lymphoma more than 1 0-fold. The increase in incidence of malignancies is probably a func tion of impaired cell-mediated immunity. In light-skinned individuals, Kaposi lesions usually appear as purplish, nonblanching lesions that can be papular or nodu lar. In the mouth, lesions are most often palatal papules, though exophytic lesions of the tongue and gingi vae may also be seen. Kaposi lesions may be confused with other vascular lesions such as angiomas and pyogenic granulomas. In this situation, Kaposi sar coma is likely to be an immune reconstitution reaction (see Inflammatory Reactions below). An anal Papanicolaou smear is performed by rotating a moistened Dacron swab about 2 em into the anal canal. However, there is no evidence that screening for anal cancer with Papanicolaou smears decreases the incidence of invasive cancer. Vaginal candidia sis may be treated with topical agents or a single dose of oral fluconazole (1 50 mg) (see Chapter 36). Recurrent vaginal candidiasis should be treated with fluconazole (1 00-200 mg) for at least 7 days. For women younger than 30 years, a Papanicolaou smear should be performed within a year of the onset of sexual activity but no later than 21 years of age. For women 30 and older, screening should continue beyond age 65 unlike the general population. Part of this increase in coronary artery disease is due to changes in lipids caused by antiretroviral agents (see Treatment sec tion on Antiretroviral Therapy below), especially stavudine and several of the Pis. Clinicians should aggressively treat con ditions that result in increased risk of heart disease, espe cially smoking, hypertension, hyperlipidemia, obesity, diabetes mellitus, and sedentary lifestyle. Tuberculosis may paradoxically worsen with new or evolving pulmonary infiltrates and lymphadenopathy. American Association for the Study of Liver Diseases and Infec tious Diseases Society of America. Younger adolescents and older adults who are at increased risk should also be screened. Although there is no proof that administration of antiret roviral medications following a sexual or parenteral drug use exposure reduces the likelihood of infection, there is suggestive data from animal models, perinatal experience, and a case-control study of health care workers who expe rienced a needle stick. The choice of antiretroviral agents and the duration of treatment are the same as those for exposures that occur through the occupational route; the preferred regimen is teno fovir 300 mg with emtricitabine 200 mg daily with raltegravir 400 mg twice a day. Some clinicians prescribe a two-drug regi men of tenofovir 300 mg and emtricitabine 200 mg (Truvada) because it is simpler for patients to take (single pill once a day), and more affordable for individuals and for public entities that provide this service to uninsured persons. In contrast to those with occupational exposures, some individuals may present very late after exposure. In addition, because the psychosocial issues involved with postexposure prophylaxis for sexual and drug use exposures are complex, it should be offered with preven tion counseling. Recommended regimens are zidovudine and lamivudine with either ritonavir-boosted lopinavir or ritonavir-boosted atazanavir. They should be made familiar with the use of condoms, including, specifically, the advice that condoms must be used every time, that space should be left at the tip of the condom as a receptacle for semen, that intercourse with a condom should not be attempted if the penis is only par tially erect, that men should hold on to the base of the con dom when withdrawing the penis to prevent slippage, and that condoms should not be reused. Women as well as men having sex with men should understand how to use condoms to be sure that their partners are using them correctly. Persons using injection drugs should be cautioned never to share needles or other drug paraphernalia. Because transmission of tuberculo sis may occur in health care settings, all patients with cough should be encouraged to wear masks. Epidemiologic studies show that needle sticks occur commonly among health care professionals, especially among surgeons performing invasive procedures, inexperi enced hospital housestaff, and medical students. Efforts to reduce needle sticks should focus on avoiding recapping needles and use of safety needles whenever doing invasive procedures under controlled circumstances. The risk is higher with deep punctures, large inoculum, and source patients with high viral loads. The preferred regimen is tenofovir 300 mg with emtricitabine 200 mg (Truvada) daily with raltegravir 400 mg twice a day. Providers who have exposures to persons who are likely to have antiretro viral medication resistance (eg, persons receiving therapy who have detectable viral loads) should have their therapy individualized, using at least two medications to which the source is unlikely to be resistant. Because reports have noted hepatotoxicity due to nevirapine in this setting, this agent should be avoided. Use of blood and blood products should be judicious, with patients receiving the least amount neces sary, and patients should be encouraged to donate their own blood prior to elective procedures. With currently available treatment, progression of disease has been markedly decreased. In addition to antiretroviral treatment, prophylactic regimens can prevent opportunis tic infections and improve survival. Prophylaxis and early intervention prevent several infectious diseases, including tuberculosis and syphilis, which are transmissible to oth ers. Recommendations for screening tests, vaccinations, and prophylaxis are listed in Table 3 1 -4.
In addition gastritis diet сексуальные effective pantoprazole 40 mg, transrectal ultra sound-guided, rather than digitally-guided, biopsy of the prostate is a more accurate way to evaluate suspicious lesions. Use of imaging should be tailored to the likelihood of advanced disease in newly diagnosed cases. Conventional radionudide (99-technetium) bone scans are superior to conventional plain skeletal radio graphs in detecting bony metastases. Most prostate cancer metastases are multiple and most commonly localized to the axial skeleton. Because of the high frequency of abnor mal scans in patients in this age group resulting from degenerative joint disease, plain films are often necessary in evaluating patients with indeterminate findings on bone scan. Intravenous urography and cystoscopy are not rou tinely needed to evaluate patients with prostate cancer. Despite application of modern, sophisticated tech niques, understaging of prostate cancer occurs in at least 20% of patients. Screening fo r Prostate Cancer Whether screening for prostate cancer results in a decrease in its mortality rates is controversial. Two large, randomized trials question the benefit of screening men for prostate cancer. Although screening resulted in a 12% increase in pros tate cancer detection, the cancer-specific mortality rate was similar in the screening and control arms (3. Most arise in the peripheral zone of the prostate, though a small percentage arise in the central (5- 1 0%) and transition zones (20%) of the gland. Pathologists utilize the Gleason grading system whereby a "primary" grade is applied to the architectural pattern of malignant glands occupying the largest area of the specimen and a "secondary" grade is assigned to the next largest area of cancer. Grading is based on architectural rather than histologic criteria, and five "grades" are possible. Adding the score of the primary and secondary grades gives a Gleason score from 2 to 10. Morbidity is limited, and the survival of patients with localized cancers (T l, T2, and selected T3) approaches 65% at 10 years. As with surgery, the likelihood of local failure correlates with technique and cancer characteristics. The likelihood of a positive prostate biopsy more than 1 8 months after radia tion varies between 20% and 60%. Patients with local recurrence are at an increased risk of cancer progression and cancer death compared with those who have negative biopsies. Ambiguous target definitions, inadequate radia tion doses, and understaging of the cancer may be respon sible for the failure noted in some series. Three-dimensional conformal radiation delivers a higher dose because of improved targeting and appears to be associated with greater efficacy as well as lower likelihood of adverse side effects compared with previous techniques. Brachyther apy-the implantation of permanent or temporary radio active sources (palladium, iodine, or iridium) into the prostate can be used as monotherapy in those with low grade or low-volume malignancies or combined with external beam radiation in patients with higher-grade or higher-volume disease. Cryosurgery In cryosurgery, liquid nitrogen is circulated through small hollow-core needles inserted into the prostate under ultra sound guidance. Local ized Disease Although selected patients may be candidates for active surveillance based on age or health and evidence of small volume or well-differentiated cancers, most men with an anticipated life expectancy in excess of 10 years should be considered for treatment. Newly introduced genomic tests may provide novel information to help guide treatment decisions. Both radiation therapy and radical prostatec tomy result in acceptable levels of local control. A large, prospective, randomized trial compared active surveillance with radical prostatectomy in 695 men with clinically local ized and well-differentiated to moderately differentiated cancers. Radical prostatectomy significantly reduced dis ease-specific mortality, overall mortality, and risks of metastasis and local progression. Active Surveilla nce the optimal treatment for patients with clinically localized prostate cancers remains controversial. A beneficial impact of treating localized prostate cancer has not been conclu sively demonstrated with respect to survival. Patients need to be advised of all treatment options, including active surveillance, with the specific benefits, risks, and limita tions. The goal of active surveillance is to avoid treatment in men who never experience disease progression while recognizing and effectively treating men with evidence of progression. Currently, treatment decisions are made based on stage and cancer grade (Gleason score) as well as the age and health of the patient. Such patients included are typically older with small volume, well-differentiated cancers. This approach is increasingly accepted and incorporated in routine clinical practice. Radical Prostatectomy During radical prostatectomy, the seminal vesicles, prostate, and ampullae of the vas deferens are removed. Refinements in technique have allowed preservation of urinary conti nence in most patients and erectile function in selected patients. Radical prostatectomy can be performed via open retropubic, transperineal, or laparoscopic (with or without robotic assistance) surgery. Local recurrence is uncommon after radical prostatectomy and related to pathologic stage. Organ-confined cancers rarely recur; however, cancers with adverse pathologic features (capsular penetration, seminal vesicle invasion) are associated with higher local (1 0-25%) and distant (20-50%) relapse rates. Ideal candidates for radical prostatectomy include healthy patients with stages T1 and T2 prostate cancers.
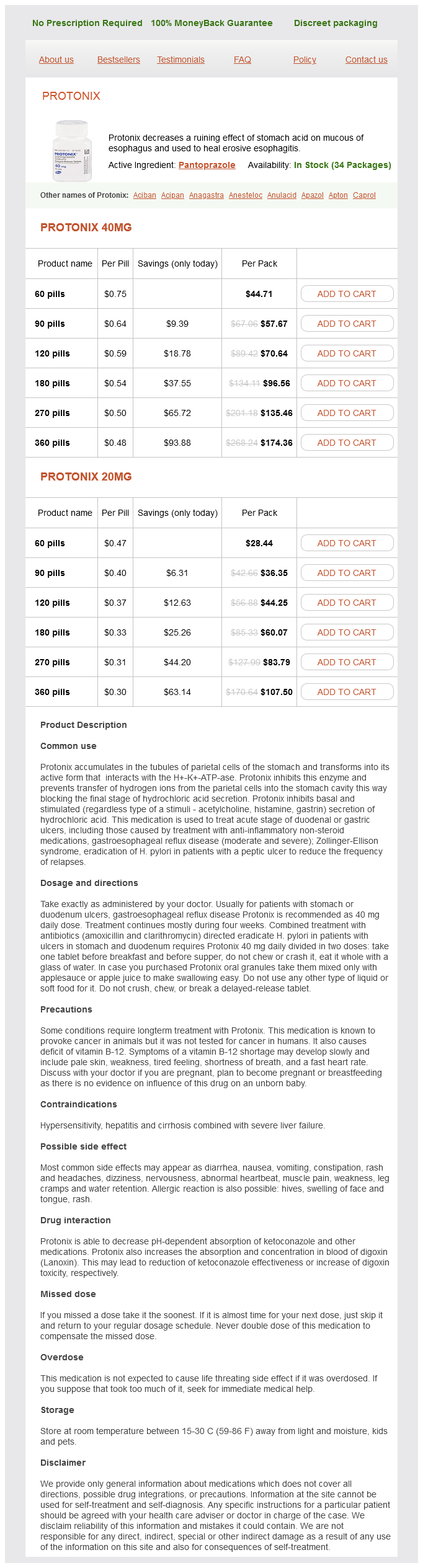
Pantoprazole Dosage and Price
Protonix 40mg
- 60 pills - $44.71
- 90 pills - $57.67
- 120 pills - $70.64
- 180 pills - $96.56
- 270 pills - $135.46
- 360 pills - $174.36
Protonix 20mg
- 60 pills - $28.44
- 90 pills - $36.35
- 120 pills - $44.25
- 180 pills - $60.07
- 270 pills - $83.79
- 360 pills - $107.50
Patients able to sit up in bed who can protect their airways can be fed into the stomach no xplode gastritis pantoprazole 20 mg with mastercard. B ecause of the increased risk of aspiration, patients who cannot ade quately protect their airways should be fed nasoduodenally (though, as noted below, this may not prevent all aspira tions, particularly if the pylorus is patulous). Feeding tubes can usually be passed into the duodenum by leaving an extra length of tubing in the stomach and placing the patient in the right decubitus position. Metoclopramide, 10 mg intravenously, can be given 20 minutes prior to insertion and continued every 6 hours thereafter to facili tate passage through the pylorus. Occasionally, patients will require fluoroscopic or endoscopic guidance to insert the tube distal to the pylorus. Placement of nasogastric and, particularly, nasoduodenal tubes should be confirmed radiographically before delivery of feeding solutions. Feeding tubes can also be placed directly into the gas trointestinal tract using tube enterostomies. Most tube enterostomies are placed in patients who require long-term enteral nutritional support. Gastrostomies have the advan tage of allowing bolus feedings, while j ejunostomies require Gastroi ntestinal tract can be used safely and effectively For undernourished patients, actual body weight should be used; for obese patients, ideal body weight should be used. Energy requirements can be estimated also by multiply ing actual body weight in kilograms (for obese patients, ideal body weight) by 30-35 kcal. Both of these methods provide imprecise estimates of actual energy expenditures, especially for the markedly underweight, overweight, and critically ill patient. Studies using indirect calorimetry have demonstrated that as many as 30-40% of patients will have measured expenditures 10% above or below estimated values. For accurate deter mination of energy expenditure, indirect calorimetry should be used. Gastrostomies-like nasogastric feeding-should be used only in patients at low risk for aspiration. Patients who require nutritional support but whose gastrointestinal tracts are nonfunctional should receive parenteral nutritional support. Most patients receive par enteral feedings via a central vein-most commonly the subclavian vein. Peripheral veins can be used in some patients, but because of the high osmolality of parenteral solutions this is rarely tolerated for more than a few weeks. Peripheral vein nutritional support is most com monly used in patients with nonfunctioning gastrointesti nal tracts who require immediate support but whose clinical status is expected to improve within 1-2 weeks, allowing enteral feeding. Peripheral vein nutritional sup port is administered via standard intravenous lines. Solu tions should always include lipid and dextrose in combination with amino acids to provide adequate non protein calories. Serious side effects are infrequent, but there is a high incidence of phlebitis and infiltration of intravenous lines. Central vein nutritional support is delivered via intra venous catheters placed percutaneously using aseptic tech nique. Proper placement in the superior vena cava is documented radiographically before the solution is infused. Catheters must be carefully maintained by experi enced nursing personnel and used solely for nutritional support to prevent infection and other catheter-related complications. As in the case of energy requirements, actual weights should be used for normal and underweight patients and ideal weights for patients with significant obesity. Patients who are receiving protein without adequate calories will catabolize protein for energy rather than uti lizing it for protein synthesis. If both energy and protein intakes are low, extra energy will have a more significant positive effect on nitrogen balance than extra protein. In most situations, solutions of equal nutrient value can be designed for delivery via enteral and parenteral routes, but differences in absorption must be considered. A complete nutritional support solution must contain water, energy, amino acids, electrolytes, vitamins, minerals, and essential fatty acids. Electrolytes & Minerals Requirements for sodium, potassium, and chloride vary widely. Patients receiving enteral nutritional support should receive adequate vitamins and minerals according to the recommended daily allowances. Most premixed enteral solutions provide adequate vitamins and minerals as long as adequate calories are administered. Patients receiving parenteral nutritional support require smaller amounts of minerals: calcium, 10- 1 5 mEq/day; phosphorus, 1 5-20 mEq per 1 000 nonprotein calories; and magnesium, 1 6-24 mEq/day. Most patients receiving nutritional support do not require supplemental iron because body stores are adequate. Iron nutrition should be monitored closely by following the hemoglobin concentra tion, mean corpuscular volume, and iron studies. Water For most patients, water requirements can be calculated by allowing 1 500 mL for the first 20 kg of body weight plus 20 mL for every kilogram over 20. Patients receiving parenteral nutritional support should be given the trace elements zinc (about 5 mg/day) and cop per (about 2 mg/day). Additional trace ele ments-especially chromium, manganese, and selenium are provided to patients receiving long-term parenteral nutrition. Standardized multivitamin solutions are currently available to provide adequate quantities of vitamins A, B 12, C, D, E, thiamine, riboflavin, niacin, pantothenic acid, pyridoxine, folic acid, and biotin. Vitamin K is not given routinely but adminis tered when the prothrombin time becomes abnormal. Essential Fatty Acids Patients receiving nutritional support should be given 2-4% of their total calories as linoleic acid to prevent essential fatty acid deficiency.