Parlodel
General Information about Parlodel
Parlodel is available in the type of tablets and is often taken a couple of times a day, with or without food, depending on the condition being treated. It could take a few weeks to see the complete advantages of the drug, and dosage may must be adjusted based on the individual�s response. It is essential to comply with the prescribed dosage and never discontinue the treatment without consulting a doctor, as all of a sudden stopping Parlodel can result in a worsening of symptoms.
Parkinson�s illness is a neurological disorder that impacts the central nervous system and causes tremors, rigidity, and problems with coordination and mobility. It is caused by a deficiency of dopamine within the brain. Parlodel helps within the remedy of Parkinson�s by stimulating dopamine receptors within the brain, which helps to alleviate symptoms corresponding to tremors, stiffness, and slow movements.
Like some other treatment, Parlodel might trigger side effects in some people. Common unwanted effects embrace nausea, dizziness, headache, and fatigue. In some instances, it may additionally cause low blood stress, hallucinations, and confusion. It is necessary to tell a physician if these signs become bothersome or if any new or unusual symptoms develop.
Acromegaly is a rare condition that occurs due to an extra production of development hormone in adults, resulting in an abnormal enlargement of certain body parts, such as hands, ft, and facial features. In some cases, it could additionally affect internal organs like the guts and intestines. Parlodel works by lowering the degrees of progress hormone in the body, thereby stopping further growth of affected physique elements and bettering symptoms corresponding to complications, joint ache, and extreme sweating.
Menstrual problems, similar to irregular or absent periods, could be caused by hormonal imbalances in the physique. Parlodel helps in the treatment of those issues by lowering the levels of prolactin, a hormone that stimulates milk manufacturing in ladies. High ranges of prolactin can interfere with the normal menstrual cycle and trigger irregular intervals. By reducing the degrees of this hormone, Parlodel can help to manage menstruation and restore a normal monthly cycle.
Prolactinomas are benign tumors of the pituitary gland that secrete extreme quantities of prolactin, which might result in a situation generally identified as hyperprolactinemia. This can cause a variety of symptoms, including irregular durations, infertility, and milk production in non-pregnant ladies. Parlodel is effective in treating hyperprolactinemia by inhibiting the manufacturing of prolactin, thereby decreasing the dimensions of the tumor and relieving symptoms associated with it.
Parlodel, also called bromocriptine, is a medicine that belongs to a class of medication called dopamine agonists. It works by mimicking the action of dopamine, a neurotransmitter within the mind that is responsible for controlling movement and feelings. Parlodel is primarily used within the therapy of Parkinson�s disease, acromegaly, menstrual issues, and excessive levels of prolactin in the blood. Let�s take a more in-depth take a glance at these situations and the way Parlodel helps in their administration.
In conclusion, Parlodel is a dopamine agonist that's broadly used within the therapy of Parkinson�s disease, acromegaly, menstrual issues, and situations caused by excessive levels of prolactin in the blood. It helps to alleviate symptoms and improve the standard of life for individuals with these situations. Like any other treatment, you will need to use Parlodel as prescribed and to report any side effects to the physician for correct administration.
The kidneys treatment 4 pimples order online parlodel, heart, and liver are the most frequently involved organs, while isolated pulmonary involvement is rare. The lung cysts often have traversing blood vessels and with no preferential zone distribution. The diagnosis is established based on histopathological findings and features that allow it to be distinguished from pulmonary amyloidosis. Biopsy will show eosinophilic granular amorphous deposits that stain positively for kappa light chains, on a background of lymphocytic infiltrates within the alveolar walls, small airways, and vessels. The amorphous material lacks the typical fibrillary structure, -pleated configuration, and Congo red stain features typical of amyloidosis. Treatment is directed at the underlying lymphoproliferative disorder, when present, with cytotoxic chemotherapy or stem cell transplantation. Case 41 A 57-year-old male with a history of severe chronic obstructive pulmonary disease undergoes single left lung transplantation without any complications. His immunosuppressive maintenance regimen consists of prednisone, mycophenolate mofetil, and azathioprine. Three weeks after his transplant, he presents with a 3-day history of fevers, fatigue, diarrhea, and a pruritic maculopapular rash on his arms and legs. Surveillance bronchoscopy with transbronchial lung biopsies done a few days prior to symptom onset did not show any evidence of rejection. Laboratory analysis reveals new onset pancytopenia and transaminitis (all previously normal). A skin biopsy is performed and reveals dermal perivascular lymphocytic infiltration with apoptotic cells. It is commonly reported after hematopoietic stem cell transplantation, but has also been described following transfusion of blood products and after solid organ transplantation, such as liver and small bowel. Symptoms may often be mistakenly attributed to side effects of immunosuppressive medication or an infection. Diagnosis is established based on clinical suspicion and biopsy (usually of the skin) demonstrating donor lymphocytes chimerism in the host. Mortality is high and is frequently related to infectious complications, which result from escalated immunosuppressive therapy. Diagnosis is established on tissue biopsy with evidence of donor lymphocyte chimerism within the host. Mortality is high despite corticosteroids and other immunosuppressive agents, likely related to delayed recognition. Severe acute graft versus host disease after lung transplant: report of a case successfully treated with high dose corticosteroids. Graft-versus-host disease in lung transplantation: 4 case reports and literature review. Case 42 A 78-year-old male presents with a history of progressive dyspnea on exertion and a nonproductive cough. He has been treated for recurrent pneumonias in the lower lobes over the last few years. He has a history of coronary artery disease, stroke with residual deficit and functional dysphagia, diabetes mellitus, and chronic constipation for which he uses mineral oil. A chest X-ray shows infiltrates in the lower lobes and he is treated with antibiotics for presumed pneumonia. It was first described by Laughlen in 1925 in patients with a history of use of chronic laxatives or oil-based nasal drops. Exogenous lipoid pneumonia may be acute or chronic in onset depending on the etiology and extent of exposure. Acute lipoid pneumonia has been reported as the result of accidental poisoning due to aspiration or inhalation of petroleum-based products (gas siphoning) as well as in "fire-eater" performers who may inhale the petroleum-based fluid kerdan as part of their act. Chronic lipoid pneumonia on the other hand has been reported in individuals with a history of prolonged use of fat-containing products or oils such as laxatives, mineral oils, lip balm, and nose drops, often in the setting of an anatomical or functional swallowing impairment. Endogenous lipoid pneumonia occurs as a result of lipid accumulation within the alveoli and intraalveolar macrophages. It has been reported in the setting of a postobstructive process (lung cancer), pulmonary alveolar proteinosis, chronic pulmonary infections, or a lipid storage disorder (Neiman-Pick syndrome). Patients with acute onset of lipoid pneumonia may present with acute onset cough, dyspnea, and respiratory failure and may be misdiagnosed as having a community-acquired pneumonia. The chronic form of the disease has a more indolent presentation with patients being asymptomatic or presenting with gradually progressive cough, dyspnea on exertion, and lowgrade fevers. The nodules, masses, or consolidations may contain areas with low attenuation (<-30 Hounsfield units), consistent with the presence of fat. The finding of large cytoplasmic vacuoles within the foamy macrophages may help distinguish exogenous lipoid pneumonia from the endogenous type that may have small cytoplasmic vacuoles. Treatment for the lipoid pneumonia is supportive or may be directed at the underlying etiology (chronic aspiration, infection, pulmonary alveolar proteinosis). Patients should be educated to avoid exposure to potential inciting agents, and aspiration risk should be assessed and minimized. In cases of chronic repetitive aspiration, lipoid pneumonia may progress to pulmonary fibrosis. Case 43 A 49-year-old male presents with complains of a nonproductive cough, low-grade fevers, chills, and unintentional weight loss over a period of 6 months. He is a nonsmoker with a history of coronary artery disease and rheumatoid arthritis. His sputum cultures and acid-fast bacilli stains are negative and antineutrophil cytoplasmic antibodies testing is negative.
Treatment Prompt and complete surgical excision of necrotic tissue and removal of foreign material are essential medications 126 purchase parlodel 2.5mg online. Management of shock, fluid and electrolyte imbalance, hemolytic anemia, and other complications is crucial. Clindamycin, metronidazole, meropenem, ertapenem, and chloramphenicol can be considered as alternative drugs for patients with a serious penicillin allergy or for treatment of polymicrobial infections. The combination of penicillin G and clindamycin may be superior to penicillin alone because of the theoretical benefit of clindamycin inhibiting toxin synthesis. Hyperbaric oxygen may be beneficial, but efficacy data from adequately controlled clinical studies are not available. Clinical Manifestations Onset is heralded by acute pain at the site of the wound, followed by edema, increasing exquisite tenderness, exudate, and progression of pain. Systemic findings initially include tachycardia disproportionate to the degree of fever, pallor, diaphoresis, hypotension, renal failure, and then, later, alterations in mental status. Crepitus is suggestive but not pathognomonic of Clostridium infection and is not always present. Diagnosis is based on clinical manifestations including the characteristic appearance of necrotic muscle at surgery. Untreated gas gangrene can lead to disseminated myonecrosis, suppurative visceral infection, septicemia, and death within hours. Etiology Clostridial myonecrosis is caused by Clostrid ium species, most often Clostridium perfrin gens. These organisms are large, gram-positive, spore-forming, anaerobic bacilli with blunt ends. Other Clostridium species (eg, Clostrid ium sordellii, Clostridium septicum, Clostrid ium novyi) have also been associated with myonecrosis. Disease manifestations are caused by potent clostridial exotoxins (eg, C sordellii with medical abortion; C septicum with malignancy). Epidemiology Clostridial myonecrosis usually results from contamination of open wounds involving muscle. The sources of Clostridium species are soil, contaminated foreign bodies, and human and animal feces. Dirty surgical or traumatic wounds, particularly those with retained foreign bodies or significant amounts of devitalized tissue, predispose to disease. Early and complete surgical excision of necrotic tissue and careful management of shock, fluid balance, and other complications are crucial for survival. Mild to moderate illness is characterized by watery diarrhea, low-grade fever, and mild abdominal pain. Pseudomembranous enterocolitis is characterized by diarrhea with mucus in feces, abdominal cramps and pain, fever, and systemic toxicity. Occasionally, children have marked abdominal tenderness and distention with minimal diarrhea (toxic megacolon). Disease often begins while the child is hospitalized receiving antimicrobial therapy but can occur up to 10 weeks after therapy cessation. Community-associated C difficile disease is less common but is increasing in frequency. The illness usually, but not always, is associated with antimicrobial therapy or prior hospitalization. Complications, which occur more commonly in older adults, can include toxic megacolon, intestinal perforation, systemic inflammatory response syndrome, and death. Severe or fatal disease is more likely to occur in neutropenic children with leukemia, infants with Hirschsprung disease (congenital megacolon), and patients with inflammatory bowel disease. Colonization with C difficile, including toxin-producing strains, occurs in children younger than 5 years and is most common in infants. It is unclear how frequently C difficile causes disease in infants younger than 1 year. Etiology Clostridium difficile is a spore-forming, obligate anaerobic, gram-positive bacillus. Epidemiology C difficile can be isolated from soil and is commonly found in the hospital environment. C difficile is acquired from the environment or from stool of other colonized or infected people by the fecal-oral route. Intestinal colonization rates in healthy infants can be as high as 50% but usually are less than 5% in children older than 5 years and adults. Hospitals, nursing homes, and child care facilities are major reservoirs for C difficile. Risk factors for acquisition of the bacteria include prolonged hospitalization and exposure to an infected person in the hospital or the community. Risk factors for C difficile disease include antimicrobial therapy, repeated enemas, gastric acid suppression therapy, prolonged nasogastric tube placement, gastrostomy and jejunostomy tubes, underlying bowel disease, gastrointestinal tract surgery, renal insufficiency, and humoral immunocompromise. C difficile colitis has been associated with exposure to almost every antimicrobial agent. Incubation Period Unknown; colitis usually develops 5 to 10 days after initiation of antimicrobial therapy. Diagnostic Tests the diagnosis of C difficile disease is based on the presence of diarrhea and detection of C difficile toxins in a diarrheal specimen.
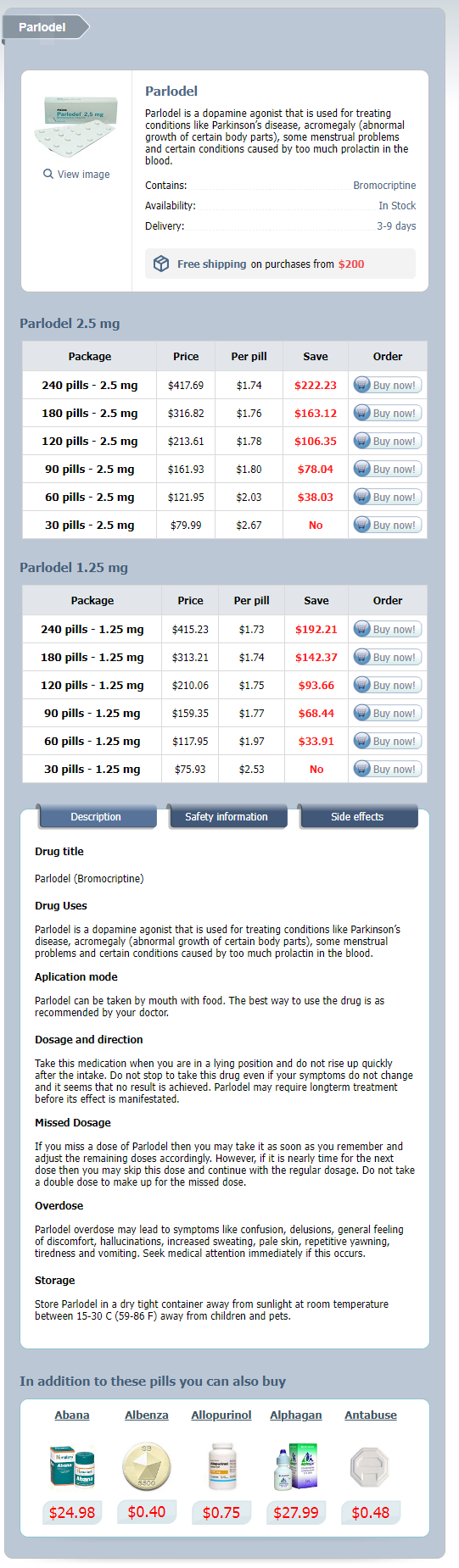
Parlodel Dosage and Price
Parlodel 2.5 mg
- 240 pills - $417.69
- 180 pills - $316.82
- 120 pills - $213.61
- 90 pills - $161.93
- 60 pills - $121.95
- 30 pills - $79.99
Parlodel 1.25 mg
- 240 pills - $415.23
- 180 pills - $313.21
- 120 pills - $210.06
- 90 pills - $159.35
- 60 pills - $117.95
- 30 pills - $75.93
In severe forms treatment 3rd degree burns parlodel 2.5 mg purchase visa, early mechanical ventilation and inotropic and pressor support are necessary. Extracorporeal membrane oxygenation should be considered when pulmonary wedge pressure and cardiac indices have deteriorated and may provide short-term support for the severe capillary leak syndrome in the lungs. Courtesy of Centers for Disease Control and Prevention/Photo credit: Cynthia Goldsmith. The virion contains 2 glycoproteins, G1 and G2, located on the outer surface, which are the nucleoprotein and the viral polymerase. The clinical manifestations of hantavirus infection vary and depend largely on the strain of the infecting virus. Courtesy of Centers for Disease Control and Prevention/ Emerging Infectious Diseases. The virus is horizontally transmitted between rodents through intraspecific aggressive behaviors, such as biting. The virus is transmitted to humans from aerosolized rodent excreta, particularly urine. Transmission to humans can also occur from inhalation of secondary aerosols and from rodent bites or other direct contact of infectious material with mucous membranes or broken skin. The deer mouse is a carrier of Sin Nombre virus, an etiologic agent of hantavirus pulmonary syndrome. The cotton rat is a hantavirus carrier that becomes a threat when it enters human habitation in rural and suburban areas. Number of reported cases by survival status and year in the united States, 19972006. Diffuse nodular confluent alveolar opacities with some consolidation consistent with adult respiratory distress syndrome. Histopathologic features of lung in hantavirus pulmonary syndrome include interstitial pneumonitis and intra-alveolar edema. Findings usually include interstitial edema, Kerley B lines, hilar indistinctness, and peribronchial cuffing with normal cardiothoracic ratios. Hantavirus pulmonary syndrome begins with minimal changes of interstitial pulmonary edema and rapidly progresses to alveolar edema with severe bilateral involvement. Pleural effusions are common and are often large enough to be evident radiographically. Notable hematologic findings include low platelet count, immunoblasts, left shift on white blood cell count differential, elevated white blood cell count, and elevated hematocrit. The large atypical lymphocyte shown here is an example of one of the laboratory findings that, when combined with a bandemia and dropping platelet count, are characteristic of hantavirus pulmonary syndrome. Notable blood chemistry findings include low albumin, elevated lactate dehydrogenase, elevated aspartate aminotransferase, and elevated alanine aminotransferase. The onset of the immune response precedes severe organ failure, which is thought to be immunopathologic in nature. Hypotension does not result in shock until the onset of respiratory failure, but this may reflect the severe physiological effect of lung edema. In children, H pylori infection can result in gastroduodenal inflammation that can manifest as epigastric pain, nausea, vomiting, hematemesis, and guaiac-positive stools. Extraintestinal conditions in children that have been associated with H pylori infection can include iron deficiency anemia and short stature. Moreover, there is no clear association between infection and recurrent abdominal pain, in the absence of peptic ulcer disease. H pylori infection is not associated with secondary gastritis (eg, autoimmune, associated with nonsteroidal antiinflammatory agents). Etiology H pylori is a gram-negative, spiral, curved, or U-shaped microaerophilic bacillus that has single or multiple flagella at one end. Epidemiology H pylori organisms have been isolated from humans and other primates. Organisms are thought to be transmitted from infected humans by the fecal-oral, gastro-oral, and oral-oral routes. Infection rates are low in children in resource-rich, industrialized countries, except in children from lower socioeconomic groups. Most infections are acquired in the first 5 years of life and can reach prevalence rates of up to 80% in resource-limited countries. Approximately 70% of infected people are asymptomatic, 20% of people have macroscopic (ie, visual) and microscopic findings of ulceration, and an estimated 1% have features of neoplasia. Diagnostic Tests H pylori infection can be diagnosed by culture of gastric biopsy tissue on nonselective or selective media at 37°C (98. The organism can also be identified by polymerase chain reaction or fluorescence in situ hybridization of gastric biopsy tissue. Organisms can usually be visualized on histologic sections with Warthin-Starry silver, Steiner, Giemsa, or Genta staining. Because of production of urease by organisms, urease testing of a gastric specimen can give a rapid and specific microbiologic diagnosis. The first H pylori breath test for children 3 to 17 years of age became available in 2012. A stool antigen test (by enzyme immunoassay) is also available and can be used for children of any age, especially before and after treatment. Each of these commercially available tests for active infection (ie, breath or stool tests) has a high sensitivity and specificity. Treatment Treatment is recommended for infected patients who have peptic ulcer disease (currently or in the past 15 years), gastric mucosa associated lymphoid tissue-type lymphoma, or early gastric cancer. Screening for and treatment of infection, if found, can be considered for children with one or more primary relatives with gastric cancer, children who are in a highrisk group for gastric cancer (eg, immigrants from resource-limited countries or countries with high rates of gastric cancer), or children who have unexplained iron deficiency anemia.