Phenytoin
General Information about Phenytoin
Phenytoin can work together with a number of other medications, so you will need to inform a healthcare skilled about all current drugs, including over-the-counter and natural dietary supplements, before starting phenytoin. It is also essential to observe the beneficial dosage directions and to not cease taking the medication abruptly, as this could result in a rebound enhance in seizure activity. Lowering or stopping phenytoin ought to solely be carried out underneath the steering of a healthcare professional.
While phenytoin is usually well-tolerated, it can cause a spread of unwanted effects, including dizziness, drowsiness, nausea, and headache. Some people could expertise more critical side effects, similar to blurred or double imaginative and prescient, confusion, or hassle respiratory. It is essential to seek the guidance of a healthcare professional if any of these unwanted facet effects occur. Additionally, it is very important observe that phenytoin may cause modifications in mood or habits, especially in youngsters and younger adults. Regular monitoring of signs is really helpful to ensure proper dosage and to minimize side effects.
One of the key advantages of phenytoin is its long-lasting impact. Once taken, it stays in the body for a very lengthy time, allowing for once every day dosing. This is particularly beneficial for patients who have issue adhering to a quantity of daily medicine schedules. On the other hand, it may possibly take as a lot as a number of days for phenytoin to achieve its peak effectiveness, so it isn't recommended for treating acute seizures.
In conclusion, phenytoin has been a extensively used and efficient medicine for controlling seizures for a couple of years. It is on the market in numerous forms, have a long-lasting impact and cut back the probability of seizures by stabilizing irregular electrical activity within the brain. It is important to follow prescribed dosage and to report any unwanted facet effects to a healthcare professional. While it will not be suitable for everyone, it has helped numerous individuals lead seizure-free lives and continues to be a vital software within the remedy of epilepsy.
Dilantin’s mechanism of action isn't fully understood, however it's believed that it stabilizes the neuronal membranes by inhibiting sodium channels within the mind. This prevents the unfold of irregular electrical exercise and reduces the occurrence of seizures. It is mostly used to treat generalized tonic-clonic seizures (formerly generally known as grand mal seizures) and partial seizures. It can also be used to forestall seizures after mind surgical procedure or trauma.
Phenytoin, marketed underneath the model name Dilantin, is a widely used medication in the remedy of seizures. It belongs to a category of drugs known as anticonvulsants, which work to regulate irregular electrical activity within the brain that can set off seizures. While there are many different medications available for seizure control, phenytoin has been a go-to choice for healthcare professionals for over half a century.
Phenytoin was first launched in the Nineteen Thirties and rapidly gained recognition as an effective treatment for epilepsy. It was the first anticonvulsant to be particularly developed for the therapy of seizures, and has since turn into one of the extensively pharmaceuticals on this category. It is on the market in each brand name and generic varieties, and is taken orally in the form of tablets, capsules or suspension.
Orthostasis can initially be treated by lifestyle modifications and limiting drugs that lower blood pressure medicine for the people quality phenytoin 100 mg. As dysautonomia worsens, pharmacologic interventions with midodrine or fludrocortisone may become necessary. In appropriate patients, erectile dysfunction can be managed with phosphodiesterase inhibitors. Therefore, patients should be screened for sleep apnea because treatment can improve daytime alertness. Nonpharmacologic treatments include removal of sharp objects from around the bed, creating barriers between bed partners, or even bed alarms. Clonazepam is often used a second line option at low doses but this should be monitored carefully as benzodiazepines are typically avoided in dementia. Clinical characteristics include autonomic dysfunction with any combination of parkinsonism and/or ataxia. Autonomic symptoms may manifest as cardiovascular in the form of orthostatic hypotension, urogenital or gastrointestinal dysfunction. Neuropsychological testing can often detect executive deficits and slowed processing speed. Autonomic reflex screen testing may demonstrate the orthostatic blood pressure drop and other signs of adrenergic or cardiovagal failure. Elevated post-void residual volumes are often seen in patients with urologic symptoms. These can be located in the cortex, subcortical areas, cerebellum, spinal cord, and dorsal root ganglia. Early in the course, lifestyle modifications can be effective including increasing salt and fluid intake, sleeping with the head of the bed elevated, learning physical maneuvers and wearing compression garments. Later, pharmacologic intervention may become necessary with fludrocortisone, midodrine, pyridostigmine, or droxidopa often providing a measure of symptomatic relief although they may cause supine hypertension. Physical and occupational therapy can be helpful with gait instability and safety evaluation. Referral to a sleep medicine specialist for evaluation of respiratory stridor should be considered as stridor carries a poor prognosis (Silber and Levine, 2000). Common neuropsychiatric features include depression, disinhibition and obsessive compulsive features. Neuropsychologic testing demonstrates prominent deficits in executive functions, language, and visual-spatial functions, with relative sparing of episodic memory at presentation (Murray et al. Tau accumulates in certain regions including cortex, basal ganglia, basal nucleus of Meynert, thalamus, and brainstem (Dickson et al. A minority of patients will have a modest response of rigidity and bradykinesia to dopaminergic therapy. If myoclonus is problematic, clonazepam, levetiracetam, and gabapentin can be considered. Physical and occupational therapy are important to prevent falls, provide adaptive equipment, and maximize function with appropriate exercises. Later the name changed to corticobasal ganglionic degeneration or corticobasal degeneration. The clinical syndrome of progressive asymmetric rigidity and apraxia became synonymous with corticobasal degeneration. Currently, corticobasal syndrome refers to the clinical syndrome characterized by asymmetric rigidity, apraxia, and alien limb phenomenon variably associated with cortical sensory loss, myoclonus, dystonia, and parkinsonism. The term corticobasal degeneration refers to the distinct pathologic entity which can present with a variety of clinical syndromes. The mean age of symptom onset is approximately 64 years, with average disease duration of 6. Language and speech difficulties can be present or even dominate the clinical presentation. Midbrain hypometabolism is also described and has been called the "pimple sign" (Botha et al. The pathology also affects motor cortex, striatum, pontine nuclei, inferior olive, and dentate nucleus. In 1911, Alois Alzheimer described the pathologic hallmark of this disorder, a rounded inclusion now called a Pick body (Alzheimer, 1911). A change in dietary preference, particularly an increased interest in sweets may occur, although indiscriminate overeating can also occur. Other features include apathy, decreased pain response, utilization behaviors, obsessive compulsive and perseverative behaviors. Agrammatism occurs and is characterized by telegraphic speech, misuse of pronouns, and errors in sentence construction. Patients will replace a specific word with a more general word such as "it" for "telephone". The speech is characterized by slow rate, sound distortions, distorted substitutions, and trial and error articulatory movements. When apraxia of speech occurs with or without agrammatism, the pathology is most often tau (Josephs et al. Other regions that can be involved include the orbitofrontal region, insula, anterior cingulate right anterior temporal lobe, and hippocampus (Rosen et al.
Isolated unilateral abducens cranial nerve palsy: a rare presentation of pituitary apoplexy medicine 4212 order phenytoin 100 mg without prescription. Radiographic evaluation of trigeminal neurovascular compression in patients with and without trigeminal neuralgia. The sensitivity of the Bielschowsky head-tilt test in diagnosing acquired bilateral superior oblique paresis. Unusual presentations of cavernous carotid aneurysms: further evidence for topographic organization of the oculomotor nerve. Management and outcomes of facial paralysis from intratemporal blunt trauma: a systematic review. Sudden headache, third nerve palsy and visual deficit: thinking outside the subarachnoid haemorrhage box. Factors affecting visual outcome in herpes zoster ophthalmicus: a prospective study. Teaching NeuroImages: internal carotid artery dissection presenting as Villaret syndrome. Hemilingual spasm: defining a new entity, its electrophysiological correlates and surgical treatment through microvascular decompression. Prediction of dysphagia severity: an investigation of the dysphagia patterns in patients with lateral medullary infarction. Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Orthostatic headache and bilateral abducens palsy secondary to spontaneous intracranial hypotension. Current neurosurgical management of glossopharyngeal neuralgia and technical nuances for microvascular decompression surgery. Abducens (sixth) nerve palsy presenting as a rare case of isolated brainstem metastasis from a primary breast carcinoma. Etiology, diagnosis, and management of facial palsy: 2000 patients at a facial nerve center. Facial nerve schwannomas of the cerebellopontine angle: the mayo clinic experience. Trigeminal neuralgia as the first clinical manifestation of anti-hu paraneoplastic syndrome induced by a borderline ovarian mucinous tumor. Neuralgia of the glossopharyngeal and vagal nerves: long term outcome following surgical treatment and literature review. Clinical course and characteristics of acute presentation of fourth nerve paresis. Brainstem manifestations in neuromyelitis optica: a multicenter study of 258 patients. The Dorello canal: historical development, controversies in microsurgical anatomy, and clinical implications. Midbrain syndromes of Benedikt, Claude, and Nothnagel: setting the record straight. Concomittant persistent pain in classical trigeminal neuralgia-evidence of different subtypes. Unilateral isolated hypoglossal nerve palsy associated with internal carotid artery dissection. Mental neuropathy as a manifestation associated with malignant processes: its significance in relation to patient survival. Bilateral pupil-sparing third nerve palsies as the presenting sign of multiple sclerosis. Surgical management of trigeminal neuralgia: use and cost effectiveness from an analysis of the medicare claims database. Hemifacial spasm, neuralgia, and syncope due to cranial nerve compression in a patient with vertebral artery ectasia. Unilateral headache attacks and ipsilateral atrophy of the tongue due to neurovascular compression of the hypoglossal nerve. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Adult hypertropia: a guide to diagnostic evaluation based on review of 300 patients. Immunoglobulin G4-related intracranial inflammatory pseudotumours along both the oculomotor nerves. Abducens nerve palsy and Horner syndrome due to metastatic tumor in the cavernous sinus. Dorello canal revisited: an observation that potentially explains the frequency of abducens nerve injury after head injury. Intramesencephalic course of the oculomotor nerve fibers: microanatomy and possible clinical significance. Trigeminal schwannomas: skull base approaches and operative results in 105 patients. Understanding skew deviation and a new clinical test to differentiate it from trochlear nerve palsy. The efficacy and safety of microvascular decompression for idiopathic trigeminal neuralgia in patients older than 65 years. Cisternal trochlear nerve schwannoma: improvement of diplopia after subtotal tumour excision.
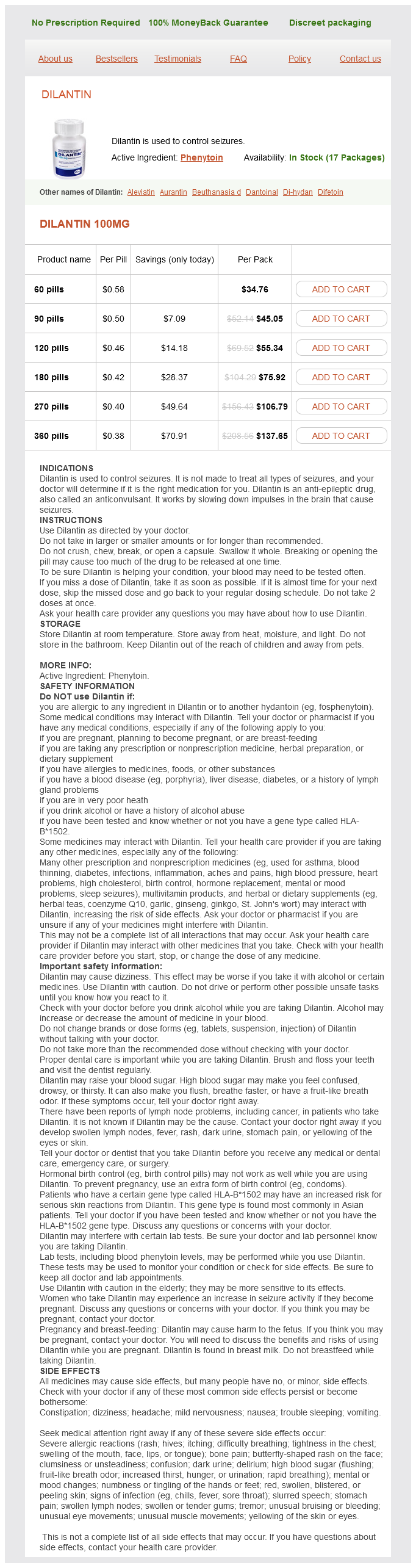
Phenytoin Dosage and Price
Dilantin 100mg
- 60 pills - $34.76
- 90 pills - $45.05
- 120 pills - $55.34
- 180 pills - $75.92
- 270 pills - $106.79
- 360 pills - $137.65
A common approach employs three exchanges (50 mL/kg) weekly for the first 2 weeks treatment of hemorrhoids buy discount phenytoin 100 mg online, followed by one or two exchanges per week from the third through the sixth week. Plasma exchange can only be performed in medical centers with special expertise in apheresis and requires secure vascular access. Venous access problems may be overcome by placement of central venous catheters, although this approach carries the risk of pneumothorax, hematoma, brachial plexus injury, and serious infection. Plasmapheresis may be difficult to maintain for months or years, and the majority of patients needing prolonged plasmapheresis require the addition of prednisone for lasting benefit and stabilization. Improvement was seen as early as the first week of treatment, whereas maximal benefit was reached at 6 weeks. Those patients who respond to the initial series of infusions may need maintenance infusions every 38 weeks. The study included a 24-week placebo-controlled phase, a response-conditional crossover phase for patients who failed to improve, and a 24-week extension phase. Infusion-related reactions include migraine attacks, aseptic meningitis, chills, nausea, and myalgias. These can be controlled by reducing the rate of infusion (<200 mL/h) or by pretreatment with acetaminophen and ibuprofen (see previous discussion). Diphenhydramine may be used for allergic manifestations like hives, seen in about 6% of patients. Thrombotic events including stroke, myocardial infarction, retinal vein occlusion, and deep vein thrombosis may occasionally occur in patients with cardiovascular risk factors and increased serum viscosity, particularly with infusion rates of greater than 0. Patients with pre-existing renal disease, especially the elderly, and those with diabetes mellitus and hypovolemia are at risk of developing acute renal tubular necrosis. Close monitoring of renal function, correction of hypovolemia, discontinuation of concomitant nephrotoxic drugs, and the use of products without sucrose are measures to prevent renal tubular necrosis in patients with pre-existing kidney disease. The serum IgA level may be determined before the first infusion because those with very low IgA levels may have allergic or anaphylactic reactions during later infusions; however, current guidelines question the necessity of this precaution. Both treatments were equally efficacious but short lived, and most patients required Disorders of Peripheral Nerves 1831 continued intermittent treatment for sustained improvement. The interval of repeat infusions is determined by the expected duration of the clinical benefit and is done on a case-by-case basis. A second dose within 3 to 4 weeks should be given, since the positive effect may require 6 weeks and two courses (Latov et al. Following the initial two treatment courses, responders are monitored at monthly intervals. Plasma exchange is combined with prednisone for severely affected nonambulatory patients because of the slightly higher response rates to these treatments. None of the alternative agents, however, have proven efficacy in controlled trials. Azathioprine (23 mg/kg/day) or mycophenolate mofetil (1000 mg twice daily) may be used as corticosteroid-sparing adjunctive agents in long-term management. Use should be limited to patients with inadequate response to corticosteroids or those who require high corticosteroid maintenance doses with unacceptable side effects. The absence of any therapeutic response from these immune-modulating therapies should lead to a reappraisal of the diagnosis. The most common causes of treatment failure are incorrect diagnosis, inadequate dose and duration of treatment, and the negative effects of concomitant and underlying illness. About 50% of patients are severely disabled at some stage by their illness and 10% of patients remain disabled in spite of treatment. Despite the initial responsiveness, only 40% of patients remained in partial or complete remission without receiving any medication. The presence and degree of axonal loss have been considered responsible for incomplete recovery. Confirmation of this view was provided by a systematic study comparing clinical outcome and biopsy findings: Six years after onset of illness, 56% had good outcome, 24% deteriorated and failed to respond to all treatments, and 11% died of complications of the disease. Cranial nerve involvement is unusual, but rare involvements of ocular, facial, hypoglossal, and phrenic nerves-the latter resulting in respiratory failure-have been reported. Minor transient paresthesias are commonly reported by patients, but objective sensory deficits are usually absent or may involve small patchy areas in the distal limbs. The course is slowly or less often stepwise progressive over months to years (Nobile-Orazio et al. The selective vulnerability of motor fibers has not been satisfactorily explained. Other features of demyelination such as motor conduction slowing, temporal dispersion, and prolonged F-wave and distal motor latencies may be present in nerves without conduction block. Transient abnormal amplitude reduction with proximal stimulation (conduction block) may occasionally be seen in vasculitic neuropathy during the early stage of wallerian degeneration. Keep in mind, however, that conduction block in some nerves may vary significantly within patients and over time. These criteria share the following features: progressive, asymmetrical, predominantly distal limb weakness in the distribution of two or more peripheral nerves, developing over months to years, with a striking predilection for the upper extremities and particularly hands, without upper motor signs. The spinal fluid protein is frequently normal, although moderately increased protein levels (<100 mg/dL) can be found in a third of patients. In 1993, Kaji and colleagues reported a patient with pure motor weakness of the arm and proximal conduction block who underwent biopsy of a motor nerve branch adjacent to the site of focal conduction block (Kaji et al.