Prinivil
General Information about Prinivil
One of the principle benefits of using Prinivil is its capability to loosen up and widen blood vessels, making it easier for the guts to pump blood throughout the physique. This results in a decrease in blood strain, reducing the pressure on the center and decreasing the danger of heart illness.
As with any medicine, there are some potential unwanted effects which will occur when taking Prinivil. These can embrace a dry cough, dizziness, headache, nausea, and fatigue. In uncommon circumstances, more extreme side effects, such as allergic reactions, kidney issues, or liver damage, could occur. It is crucial to notify a health care provider if any of these unwanted effects persist or worsen.
Before starting Prinivil, it is important to tell your physician of some other medications you are taking, in addition to any pre-existing medical circumstances. Patients with a history of kidney illness or diabetes might require a lower dosage of Prinivil or cautious monitoring whereas taking this medication.
High blood pressure, also called hypertension, is a typical condition that affects millions of individuals worldwide. If left untreated, it could lead to severe health issues such as coronary heart attack, stroke, and even coronary heart failure. Prinivil is an efficient therapy for hypertension, and it has been confirmed to considerably lower blood strain ranges.
Moreover, Prinivil is also recommended for use after a heart assault to extend the chances of survival. When taken within the first 24 hours after a coronary heart assault, this medicine might help stop additional injury to the heart and enhance the heart's capacity to recover. It does this by decreasing blood stress and lowering the workload on the heart, permitting it to heal extra efficiently.
Prinivil, additionally recognized by its generic name Lisinopril, is a medication generally used to deal with high blood pressure, congestive heart failure, and to enhance survival after a heart assault. This drug belongs to a class of medicines referred to as ACE inhibitors, which work by relaxing blood vessels and serving to the heart to operate more efficiently.
Prinivil is available in pill type and is often taken as quickly as a day. The dosage and length of treatment will rely upon the individual's condition and response to the medicine. It is essential to observe the prescribed dosage and not to stop taking the medication without consulting a doctor, as abruptly stopping Prinivil may cause a sudden increase in blood strain.
In conclusion, Prinivil is a broadly prescribed and effective treatment for controlling high blood pressure, managing congestive coronary heart failure, and bettering survival charges after a coronary heart assault. Its ability to loosen up blood vessels and cut back blood pressure makes it an important medicine for coronary heart well being. With proper utilization and monitoring, Prinivil can considerably improve the standard of life for those suffering from these situations. However, it is important to all the time consult a health care provider and talk about any concerns before beginning any new medicine.
In addition to treating hypertension, Prinivil can also be prescribed for sufferers with congestive coronary heart failure. This condition occurs when the heart is unable to pump sufficient blood to meet the physique's needs. Prinivil can help improve coronary heart perform by dilating blood vessels, which permits for higher blood circulate to the guts. This not only reduces symptoms of heart failure but additionally improves the general quality of life for sufferers.
Th1/Th2 balance: the hypothesis blood pressure medication good for kidneys purchase prinivil now, its limitations, and implications for health and disease. Assessment of chemokine receptor expression by human Th1 and Th2 cells in vitro and in vivo. Update on the extended family of chemokine receptors and introducing a new nomenclature for atypical chemokine receptors. Host protective roles of type 2 immunity: parasite killing and tissue repair, flip sides of the same coin. Immunoregulation of cytokines in infectious diseases (leprosy), future strategies. Active tuberculosis in Africa is associated with reduced Th1 and increased Th2 activity in vivo. Relationship between immunity to Borrelia burgdorferi outer-surface protein A (OspA) and Lyme arthritis. Risk factors for recurrence, complications and mortality in Clostridium difficile infection: a systematic review. Innate lymphoid cells as regulators of immunity, inflammation and tissue homeostasis. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Terms of Use · Privacy Policy · Notice · Accessibility Page 20 / 20 Countway Medical Library Access Provided by: Williams Hematology, 10e Chapter 77: Classification and Clinical Manifestations of Lymphocyte and Plasma Cell Disorders Yvonne A. The second is caused by disorders that result from factors extrinsic to lymphoid cells. The third is composed of disorders caused by neoplastic or preneoplastic lymphoid cells and are further delineated in Chapter 89 using the World Health Organization classification of tumors of lymphoid tissues. The clinical manifestations of diseases in any one of the three groups may be difficult to distinguish, but this grouping can provide a framework with which to proceed in evaluating patients with known or suspected lymphocyte and plasma cell disorders. This article introduces the framework and presents a roadmap to other chapters in this book that discuss each of the disorders in greater detail. These disorders primarily result from inherited disorders in lymphocyte metabolism (Chaps. The second group listed under "acquired disorders," consists of disorders caused by factors extrinsic to lymphocytes, resulting in immune dysfunction. These conditions most commonly result from an infection with viruses, bacteria, or other pathogens (Chaps. The third group of diseases is composed of neoplastic lymphocyte disorders and is discussed in detail in Chapter 89. Associated with plasma cell myeloma, heavy-chain disease, light-chain amyloid, Waldenström macroglobulinemia, or chronic lymphocytic leukemia (Chaps. IgG and IgA deficiencies and impaired cellular immunity (type I dysgammaglobulinemia)83 5. Sarcoidosis105 Countway Medical Library Access Provided by: Some categories of lymphocyte and plasma cell disorders may be difficult to distinguish clinically because lymphocyte disorders can have many clinical manifestations that are not restricted to cells of the immune system, and disparate disorders can have similar clinical manifestations, with any one disorder associated with a diverse array of clinical pathologies. In some cases, the classification of lymphocyte disorders is influenced by the manifestations of the disease. The blood cell that is coated with autoantibody presumably is normal, yet we classify the disease that can result from hemolytic autoantibodies as an acquired hemolytic anemia because that aspect of the disease is more visible and better understood than is the inappropriate synthesis of antierythrocyte antibody by the disturbed lymphocyte population(s). Many diseases, especially infection (eg, tuberculous adenitis), inflammatory states (eg, rheumatoid arthritis), autoimmune disease (eg, systemic lupus erythematosus, Sjögren syndrome), and metastatic carcinoma can involve lymph nodes or the spleen as a secondary alteration. These disorders also may be associated with abnormal production of antibodies, such as those resulting in the lupus anticoagulant (Chap. These disorders also are not considered here because the primary disease is not generally considered a lymphocyte disorder. The manifestations may consist of a specific deficiency of one of the immunoglobulin (Ig) isotypes or of several or all Ig molecules (panhypogammaglobulinemia; Chap. Inability to synthesize or secrete antibodies impairs the clearance of pathogens because of the inability to opsonize microorganisms for phagocytosis, resulting in immune dysregulation and dysfunction (Chap. Abnormal Immunoglobulin Production the development of a B-cell clone can result in excess production of a molecularly restricted isotype of Ig that represents essential monoclonal gammopathy (Chap. Monoclonal gammopathy is a nonprogressive neoplasm that can undergo clonal evolution to a B-cell malignancy such as chronic lymphocytic leukemia (Chap. Deposition of Ig or Ig fragments can contribute to primary amyloid formation (Chap. Abnormal Immunoglobulin Production Countway Medical Library Access Provided by: the development of a B-cell clone can result in excess production of a molecularly restricted isotype of Ig that represents essential monoclonal gammopathy (Chap. Production of abnormal Ig molecules or Ig fragments can also be seen in association with chronic infection or to a manifestation of Ig heavy-chain disease (Chap. Reactivity of the Ig with self-antigen(s), such as those found on the red cell membrane (Chap. A deficit or functional disturbance in these T cells can impair the cellular immune response to Mycobacteria spp, Listeria, Brucella, fungi, or other intracellular organisms associated with formation of immune granulomas. Eosinophilia, hypergammaglobulinemia, development of autoantibodies, and plasmacytosis can occur. A similar qualitative reaction, albeit more limited, is seen in mononucleosis resulting from Epstein-Barr virus infection (Chap. Complete defects can result in early death, typically during the first year of life, from uncontrolled infection. Advances in gene therapy and allogeneic stem cell transplantation offer hope in some cases (Chap. Patients typically have neutropenia, anemia, vasculitic syndromes, fever of unknown origin, constitutional symptoms, cutaneous lesions, and autoimmune disorders, including rheumatoid arthritis, lupus erythematosus, Sjögren syndrome, and/or polymyalgia rheumatica. Studies seeking to define this condition as a clonal disorder using X-linked gene analysis have not yielded consistent findings (Chap.
High-dose cytosine arabinoside and daunorubicin induction therapy for adult patients with de novo non M3 acute myelogenous leukemia: impact of cytogenetics on achieving a complete remission blood pressure chart free printable purchase genuine prinivil on line. The impact of karyotype on remission rates in adult patients with de novo acute myeloid leukemia receiving high-dose cytarabine-based induction chemotherapy. High-dose cytarabine in acute myeloid leukemia treatment: a systematic review and meta-analysis. Timed sequential chemotherapy for previously treated patients with acute myeloid leukemia: longterm follow-up of the etoposide, mitoxantrone, and cytarabine-86 trial. Timed-sequential chemotherapy as induction and/or consolidation regimen for younger adults with acute myelogenous leukemia. Treatment of core-binding-factor in acute myelogenous leukemia with fludarabine, cytarabine, and granulocyte colony-stimulating factor results in improved event-free survival. Addition of cladribine to daunomycin and cytarabine increases remission rate after a single course of induction treatment in acute myeloid leukemia. Comparison of idarubicin + ara-C, and topotecan + ara-C-, and topotecan + ara-C-based regimens in treatment of newly diagnosed acute myeloid leukemia, refractory anemia with excess blasts in transformation, or refractory anemia with excess blasts. Use of hematopoietic growth factors in the treatment of acute myelogenous leukemia. A strategy of day14 bone marrows and early intervention is not superior to a strategy of noDay14 bone marrows and delayed intervention in patients with acute myeloid leukemia. Factors predicting complete remission and subsequent disease-free survival after a second course of induction therapy in patients with acute myelogenous leukemia resistant to the first. Predictors of response to reinduction chemotherapy for patients with acute myeloid leukemia who do not achieve complete remission with frontline induction chemotherapy. Midostaurin in combination with intensive chemotherapy is safe and associated with improved remission rates and higher transplantation rates in first remission-a multi-center historical control study. Novel methylation targets in de novo acute myeloid leukemia with prevalence of chromosome 11 loci. Treatment with a 5-day versus a 10-day schedule of decitabine in older patients with newly diagnosed acute myeloid leukaemia: a randomised phase 2 trial. Genome-wide methylation profiling in decitabine-treated patients with acute myeloid leukemia. Clinical response and miR-29B predictive significance in older patients treated with a 10-day schedule of decitabine. Safety and preliminary efficacy of venetoclax with decitabine or azacitidine in elderly patients with previously untreated acute myeloid leukaemia: a non-randomised, open-label, phase 1b study. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Venetoclax combined with low-dose cytarabine for previously untreated patients with acute myeloid ©2021 McGraw Hill. Safety and preliminary efficacy of venetoclax with decitabine or azacitidine in elderly patients with previously Access Provided by: untreated acute myeloid leukaemia: a non-randomised, open-label, phase 1b study. Why are hypomethylating agents or low-dose cytarabine and venetoclax so effective Association of leukemia genetics with response to venetoclax and hypomethylating agents in relapsed/refractory acute myeloid leukemia. Real-world experience of venetoclax with azacitidine for untreated patients with acute myeloid leukemia. Venetoclax in patients with acute myeloid leukemia refractory to hypomethylating agents-a multicenter historical prospective study. Venetoclax with azacitidine disrupts energy metabolism and targets leukemia stem cells in patients with acute myeloid leukemia. Randomized comparison of low dose cytarabine with or without glasdegib in patients with newly diagnosed acute myeloid leukemia or high-risk myelodysplastic syndrome. Pathophysiology-directed therapy for acute hypoxemic respiratory failure in acute myeloid leukemia with hyperleukocytosis. Infectious complications in pediatric acute myeloid leukemia: analysis of the prospective multi-126 / 173 758. Beliefs and practice patterns in hyperleukocytosis management in acute myeloid leukemia: a large U. Antifungal prophylaxis with itraconazole in neutropenic patients with acute leukaemia. Posaconazole vs fluconazole or itraconazole prophylaxis in patients with neutropenia. Acyclovir prophylaxis and fever during remission-induction therapy of patients with acute myeloid leukemia: a randomized, double-blind, placebo-controlled trial. Outpatient management following intensive induction or salvage chemotherapy for acute myeloid leukemia. Granulocyte colony-stimulating factor and granulocyte-macrophage colony-stimulating factor in the treatment of myeloid leukemia. Platelet transfusion for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. The value of combination therapy in adult acute myeloid leukemia with central nervous system involvement. Safety of lumbar puncture for adults with acute leukemia and restrictive prophylactic platelet trans-fusion. Management of extramedullary leukemia as a presentation of acute myeloid leukemia. Clinico-pathological characteristics of myeloid sarcoma at diagnosis and during follow-up: report of 12 cases from a single institution. Autologous or allogeneic bone marrow transplantation compared with intensive chemotherapy in acute myelogenous leukemia. Comparison of autologous bone marrow transplantation and intensive chemotherapy as postremission therapy in adult acute myeloid leukemia.
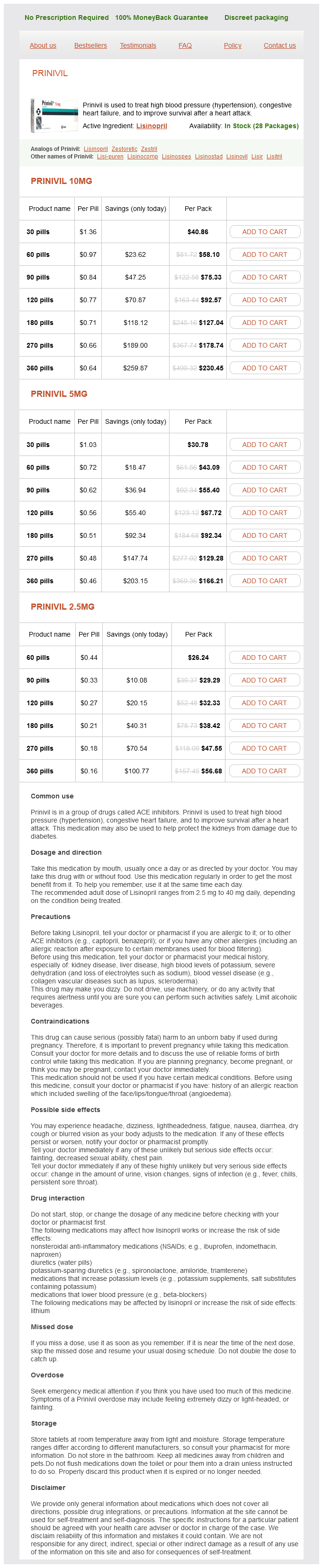
Prinivil Dosage and Price
Prinivil 10mg
- 30 pills - $40.86
- 60 pills - $58.10
- 90 pills - $75.33
- 120 pills - $92.57
- 180 pills - $127.04
- 270 pills - $178.74
- 360 pills - $230.45
Prinivil 5mg
- 30 pills - $30.78
- 60 pills - $43.09
- 90 pills - $55.40
- 120 pills - $67.72
- 180 pills - $92.34
- 270 pills - $129.28
- 360 pills - $166.21
Prinivil 2.5mg
- 60 pills - $26.24
- 90 pills - $29.29
- 120 pills - $32.33
- 180 pills - $38.42
- 270 pills - $47.55
- 360 pills - $56.68
In patients who have portal hypertension resulting from intrahepatic block or hepatic vein thrombosis and who have a hepatic venous pressure gradient well above the upper limits of normal (6 torr) blood pressure essentials purchase prinivil 5 mg with amex, a splenorenal shunt used to be performed,473 but to avoid abdominal surgery, a transjugular intrahepatic portosystemic shunt is used. Marrow transplantation therapy has been used increasingly in younger patients with a poor prognosis (eg, severe anemia and leukopenia or exaggerated leukocytosis) who have a histocompatible sibling. Lichtman Patients younger than age 50 years who are transplanted with stem cells from a matched-sibling donor have a lower posttransplantation mortality and ©2021 McGraw Hill. Terms of Use · Privacy Policy · Notice · Accessibility have better outcomes than those older than age 50 years. Although a large spleen may slightly delay the expression of donor granulopoiesis, on average the results in patients with a spleen is the same as those who had prior splenectomy. Patients younger than age 50 years who are transplanted with stem cells from a matched-sibling donor have a lower posttransplantation mortality and have better outcomes than those older than age 50 years. One study showed that the outcome of nonmyeloablative transplantation was dramatically better than myeloablative transplant. The transplantationrelated mortality was 10% in the nonmyeloablative group and 30% in the myeloablative group. There was no difference in survival for high- or low-risk patients or between sibling and unrelated donor transplantations. This study confirmed prior smaller comparisons of myeloablative and nonmyeloablative stem cell transplantation. Patients with intermediate-1risk disease and age younger than 65 years should be considered as candidates if they present with either transfusion-dependent anemia or greater than 2% blasts in the blood, or adverse cytogenetic findings. Abnormalities such as 13q or 20q did not affect patient survival compared with patients without cytogenetic alterations. Each retrospective study has found a different subset of these factors to be significant prognostic factors. The most consistent predictive variables appear to be advanced age, severity of anemia, and higher-risk clonal cytogenetic abnormality at the time of diagnosis, each of which represents a poor prognostic indicator. Lichtman were older than age 65 years, had a hemoglobin concentration less than 10 g/dL, a leukocyte count greater than 25 × 109/L, a blood blast cell count/ 52 ©2021 McGraw Hill. Terms of Use · Privacy Policy · Notice · Accessibility based on the number of risk factors present. The patients were assigned to a risk group no risk factors were present, risk was low; if one factor was present, risk was low-intermediate; if two risk factors were present, risk was highintermediate; and if three or more risk factors were present, risk was high. The application of these variables could distinguish among patients with Each retrospective study has found a different subset of these factors to be significant prognostic factors. The most consistent predictive variables Countway Medical Library appear to be advanced age, severity of anemia, and higher-risk clonal cytogenetic abnormality at the time of diagnosis, each of which represents a poor prognostic indicator. Shorter survival was observed in patients who were older than age 65 years, had a hemoglobin concentration less than 10 g/dL, a leukocyte count greater than 25 × 109/L, a blood blast cell count equal to or greater than 1%, and constitutional symptoms. The patients were assigned to a risk group based on the number of risk factors present. If no risk factors were present, risk was low; if one factor was present, risk was low-intermediate; if two risk factors were present, risk was highintermediate; and if three or more risk factors were present, risk was high. The application of these variables could distinguish among patients with low risk with a survival of 135 months, low-intermediate risk with a survival of 95 months, high-intermediate risk with a survival of 48 months, and high risk with a survival of 27 months. The major causes of death are infection, hemorrhage, postsplenectomy mortality, and acute leukemic transformation. Treatment with erythropoietin or androgens is associated with increased risk of progression to acute leukemia, as well. Patients have been followed for decades without requiring significant treatment,523 and spontaneous remission has been described. Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Primary chronic myelofibrosis: clinical and prognostic evaluation in 336 Japanese patients. Idiopathic myelofibrosis: initial features, evolutionary pattern and survival in a series of 106 patients. Prognostic factors in agnogenic myeloid metaplasia: a report on 195 cases with a new scoring system. Primary myelofibrosis: a detailed analysis of the clinicopathologic variables influencing survival. Myelofibrosis with myeloid metaplasia in young individuals: disease characteristics, prognostic factors and identification of risk groups. Familial infantile myelofibrosis as an autosomal recessive disorder: preponderance among children from Saudi Arabia. Myelofibrosis with myeloid metaplasia in adult individuals 30 years old or younger: presenting features, evolution and survival. Familial myeloproliferative syndromes: study of 6 families and review of literature. Increased risks of polycythemia vera, essential thrombocythemia, and myelofibrosis among 24,577 first-degree relatives of 11,039 patients with myeloproliferative neoplasms in Sweden. Epidemiology of the myeloproliferative disorders: essential thrombocythaemia, polycythemia vera, and idiopathic myelofibrosis. Incidence of chronic myeloproliferative disorders in the city of Gotesborg, Sweden 19831992.