Propecia
General Information about Propecia
In conclusion, Propecia is an efficient remedy for hair loss in men caused by male sample baldness. It works by inhibiting the enzyme responsible for changing testosterone into DHT, which contributes to hair loss. Additionally, it is also accredited for the therapy of prostate most cancers and BPH. While it may take time to see results, Propecia has been proven to be a safe and effective therapy for hair loss, giving men again their confidence and shallowness.
Propecia is generally secure and well-tolerated, with gentle unwanted effects reported in some people. These side effects could include decreased libido, erectile dysfunction, and decreased ejaculate volume. However, these unwanted facet effects are uncommon and usually resolve once the treatment is stopped. In uncommon instances, some people have reported depression and breast tenderness while taking Propecia. It is essential to discuss any potential side effects with a healthcare provider earlier than starting the medicine.
Propecia, additionally recognized by its generic name finasteride, is a drugs used to treat hair loss in males, particularly male sample baldness. Male pattern baldness is a hereditary condition that impacts roughly 50 million males in the United States alone. It is characterised by a receding hairline and thinning of the hair on the crown and temples. Propecia works by inhibiting the enzyme 5-alpha reductase, which converts testosterone into dihydrotestosterone (DHT). DHT is understood to contribute to hair loss in individuals who are genetically predisposed to male pattern baldness.
As with any treatment, it's essential to make use of Propecia as directed by a healthcare supplier. It is not recommended to be used in women, because the medication may be absorbed by way of the pores and skin and trigger hurt to a developing fetus. Women who're pregnant or might become pregnant shouldn't deal with crushed or damaged Propecia tablets. It can additionally be not beneficial for use in children.
Hair loss is usually a distressing experience for a lot of individuals, notably males. As we age, it is pure for our hair to thin and finally fall out. However, for some men, hair loss can occur at a younger age and have a major impression on their self-esteem and confidence. Fortunately, there's a solution – Propecia.
Apart from getting used to treat hair loss, Propecia can also be approved by the FDA for the remedy of prostate most cancers and benign prostatic hyperplasia (BPH). BPH is a non-cancerous enlargement of the prostate gland, generally seen in men over the age of fifty. Finasteride helps to scale back the size of the prostate gland and alleviate signs corresponding to problem urinating, frequent urination, and urinary retention. Just like in hair loss therapy, Propecia works by inhibiting the conversion of testosterone into DHT, which contributes to the expansion of the prostate gland.
Propecia is on the market in a capsule kind and is usually taken once a day. It takes time to see the outcomes, and it's important to proceed taking the medicine as prescribed for at least three months before figuring out its effectiveness. Most males will begin to see enchancment of their hair development after six months, and the total impact could be seen after one yr of steady use. It is crucial to notice that Propecia is just efficient in treating hair loss on the scalp and will not help regrow hair on different parts of the physique.
Management · History: is there a family history of similar convulsions with benign prognosis Epileptic encephalopathy If no cause is evident consider the investigations for epileptic encephalopathy (see Box 14 hair loss on mens lower legs cheap 1 mg propecia mastercard. Benign myoclonic epilepsy of infancy this form of epilepsy requires no further investigation or therapy providing that what is observed meets the following criteria. Investigations Take a thorough history and examination and make sure that you have excluded tuberous sclerosis (see b pp. Then, use the series of investigations on the previous page for epileptic encephalopathy. Prednisolone therapy · Step 1: 15mg* oral/tds for the first week · Step 2: Continuing seizures. However, if negative and the clinical picture is atypical, then use the screening investigations for epileptic encephalopathy (b p. Treatment the treatment should follow a sequence, adding anticonvulsants if there is no response. Myoclonic astatic epilepsy A condition with: · myoclonic astatic seizures; · myoclonic jerks; · generalized tonicclonic seizures. Seizures in this condition are likely to be unresponsive, so consider using the ketogenic diet early in refractory cases. LennoxGastaut syndrome A condition with: · Tonic seizures with trunk flexion (often evolving out of infantile spasms). Seizures include combinations of: · typical absences; · myoclonia; · tonic seizures and generalized tonicclonic seizures; · myoclonic jerks. Myoclonic absence epilepsy · Typical absences with short symmetrical jerks of mainly the upper limbs with abduction and elevation. Juvenile absence epilepsy · Onset towards the end of the first and during the second decade. Treatment of idiopathic generalized epilepsies · First-line: sodium valproate is normally used as first-line therapy, except in childhood absence epilepsy, where ethosuximide can be considered. In girls aged >9yrs, families should be counselled that it is up to twice as likely to produce seizure freedom as other drugs. Some experts (but not others) consider it may stimulate appetite and increase the incidence of polycystic ovary syndrome. All experts agree that it is significantly more teratogenic than other anti-epileptic drugs if taken during pregnancy at a dose of more than 1000mg per day. Some clinicians advocate using a benzodiazepine and suggest clonazepam as the most effective. However, it is extremely difficult to withdraw if it is used in moderate to high dosage. The majority of children with this condition have infrequent, short seizures and the decision whether to treat or not is taken after discussion with the parents and child. Some clinicians feel strongly that therapy should be the same as in idiopathic generalized epilepsy, but others will consider using carbamazepine. Benign childhood occipital seizure syndrome (Panayiotopoulos syndrome) · Young children (aged 17yrs). At that point it is not possible to classify them if the onset has not been witnessed. Frontal lobe epilepsies these children tend to have short, but frequent seizures-particularly arising out of sleep. They are often associated with asymmetric dystonic posturing and brought on by loud noises. Occipital lobe epilepsies these episodes are associated with simple multicoloured blobs of light in one side of a visual field. However, sodium valproate is a logical choice amongst the older anticonvulsants (but not in girls >9yrs of age). Of the newer anticonvulsants, lamotrigine, topiramate, and levetiracetam could be used, but licensing conditions should be noted. These are almost always associated with focal signs on examination or a suggestive history (see b pp. History the headache may be reported to be severe enough to take time off school, but with few objective signs of pain. Treatment · Reassure the family that, with the thorough history and examination, migraine and tumours can be excluded. Sympathize with the family over the problem and suggest analgesia, but at best it is likely to make no difference. Encourage the child or young person to continue doing all the normal activities for somebody of their age. It is important to exclude secondary cases caused by: · Drugs: steroid withdrawal; vitamin A; thyroid replacement; oral contraceptive pills; phenothiazines. If they occur frequently (more than 4 times per month for more than 3mths), the diagnosis is unlikely. If the headache occurs daily then the term chronic headache should be used and managed as described on b p. Treatment · Exclude triggers: such as diet, dehydration, overtiredness, and stress. Sumatriptan may be used in children older than 12yrs at the onset of symptoms, if other treatments are ineffective.
Defined as hyperglycaemia requiring insulin therapy occurring in the first few weeks of life hair loss products for women propecia 1 mg buy amex, transient (5060%) and permanent forms are recognized. Chromosome 6 abnormalities are observed in many (paternal duplications; paternal isodisomy; methylation defects). It is primarily due to a defect in pancreatic insulin secretion, although modest insulin resistance is also recognized. Genetic mutations resulting in insulin receptor and post-receptor signalling defects underlie the mechanism of severe insulin resistance. Common clinical features include acanthosis nigricans and evidence of ovarian hyperandrogenism in females. Thyroid function may be normal (euthyroid), underactive (hypothyroid), or overactive (hyperthyroidism). Other rare causes include: · thyroid teratoma; · endemic iodine deficiency; · thyroid hormone biosynthetic defects. It is not associated with disturbance of thyroid function and is not associated with either inflammation or neoplasia. Potential causes of a solitary thyroid nodule include: · benign adenoma; · thyroglossal cyst; · ectopic, normal thyroid tissue; · single median thyroid gland; · thyroid cyst or abscess; · thyroid carcinoma. Cold nodules or nodules that feel hard on palpation, or are rapidly growing should raise suspicion of thyroid cancer. Many carcinomas of the thyroid in the past were associated with previous direct irradiation to the head and neck tissues for other conditions. Carcinomas of the thyroid are histologically classified as being either papillary, follicular, or mixed. Metastases to the lung may be observed radiologically, but are usually asymptomatic. Prognosis is usually very good, even with presence of cervical node and/or metastases at diagnosis. Congenital hypothyroidism is a relatively common condition, occurring in approximately 1/4000 births. Aetiology the causes of congenital hypothyroidism include the following: · Thyroid dysgenesis (85%): usually sporadic; resulting in thyroid aplasia/ hypoplasia, ectopic thyroid (lingual/sublingual). Clinical features Usually non-specific; they are difficult to detect in first month of life. They include: · umbilical hernia; · prolonged jaundice; · constipation; · hypotonia; · hoarse cry; · poor feeding; · excessive sleepiness; · dry skin; · coarse faecies; · delayed neurodevelopment. Diagnosis In most developed countries there are national neonatal biochemical screening programmes. Thyroid imaging is also recommended to determine whether the cause is due to thyroid dysgenesis or due to hormone biosynthetic disorder. The earlier the treatment with oral thyroid hormone replacement therapy is initiated the better the prognosis: levothyroxine (initial dose 1015micrograms/kg/day). Transient hyperthyrotropinaemia this is uncommon and is usually detected at the time of neonatal thyroid screening. It is probably due the transplacental transmission of maternal thyroid antibodies to the child in utero. Aetiology Acquired hypothyroidism may be due to a primary thyroid problem or indirectly to a central disorder of hypothalamicpituitary function. Clinical features the symptoms and signs of acquired hypothyroidism are usually insidious and can be extremely difficult to diagnose clinically. Diagnosis Diagnosis is dependent on biochemical confirmation of hypothyroid state. In this situation replacement thyroxine therapy is also necessary to achieve euthyroidism. Antithyroid therapy is usually given for 1224mths in children, before considering a trial off treatment. Prognosis Following completion of treatment 4075% of children will relapse over the next 2yrs. Relapses may be treated with a further course of antithyroid drugs, although definitive therapy with radioiodine is being offered as the first-line treatment. Following ablative treatment (either radioiodine or surgery), lifelong thyroxine replacement therapy will be required. Presentation Clinical presentation is usually insidious with a diffusely enlarged, nontender, firm goitre. Many children who are initially euthroid eventually develop hypothyroidism within a few months or years of presentation. Investigations · Diagnosis can be established by thyroid biopsy (but not indicated). Organisms include Staphylococcus aureus, streptococci, and Escherichia coli (rarely, fungal infection). Mineralocorticoid activity remains normal as this is mainly regulated by the angiotensinrenin system. Secondary · Defects of hypothalamus/pituitary structures: · congenital-pituitary hypoplasia; · intracranial masses: tumours. Typically, clinical features are gradual in onset with partial insufficiency leading to complete adrenal insufficiency with impaired cortisol responses to stress and illness (adrenal crises): · anorexia and weight loss; · fatigue and generalized weakness; · dizziness (hypotension); · salt craving (primary adrenal insufficiency); · hyperpigmentation (primary adrenal insufficiency); · reduced pubic/axillary hair (primary adrenal insufficiency); · hypoglycaemia (neonates/infants). Adrenal stimulation tests Usually required to establish a diagnosis of adrenal insufficiency and are used to demonstrate inappropriately low serum cortisol responses to physiological or pharmacological stimulation of the adrenal glands. Insulin-induced mild hypoglycaemia is used to assess the integrity of the entire hypothalamicpituitaryadrenal axis. Recent onset secondary adrenal insufficiency may produce a normal response to a short synacthen test.
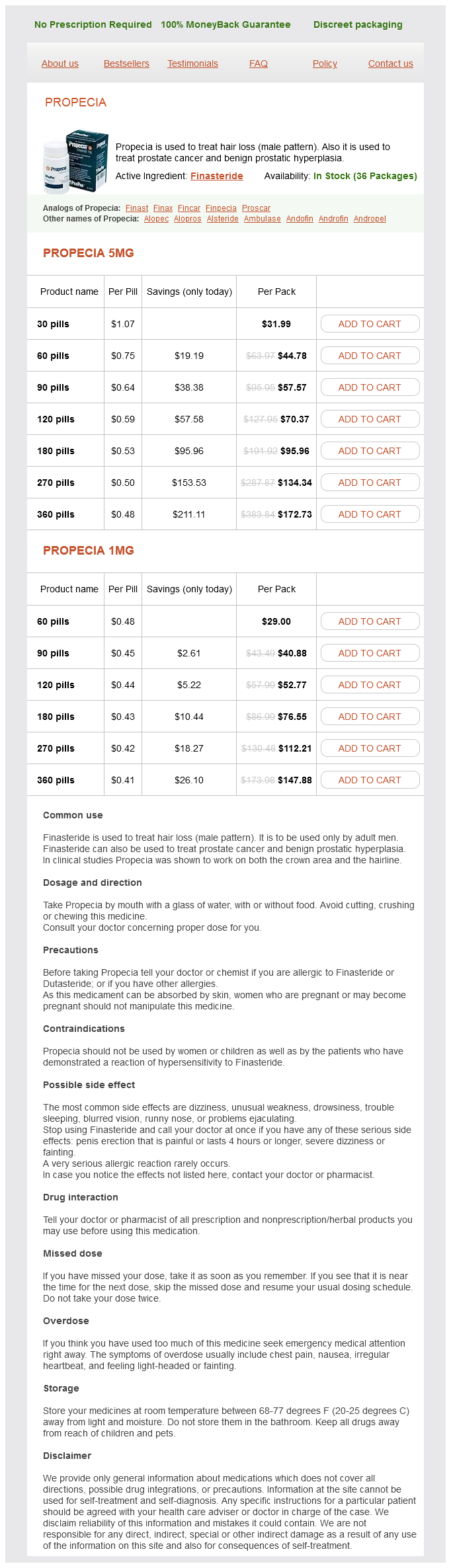
Propecia Dosage and Price
Propecia 5mg
- 30 pills - $31.99
- 60 pills - $44.78
- 90 pills - $57.57
- 120 pills - $70.37
- 180 pills - $95.96
- 270 pills - $134.34
- 360 pills - $172.73
Propecia 1mg
- 60 pills - $29.00
- 90 pills - $40.88
- 120 pills - $52.77
- 180 pills - $76.55
- 270 pills - $112.21
- 360 pills - $147.88
The camera port is changed and the appendix is grasped with forceps and simply delivered through the umbilical port site hair loss 60 year old woman propecia 1 mg buy without prescription, where a stoma is then created. A needle and thread is passed in to the colon, grasped, and delivered through the anus. This is attached to a gastrostomy tube, which is pulled up in to the colon until the flange on the tube pulls the colon to the abdominal wall. The V-flap is gradually sutured in to the defect until approximately 50 percent of the circumference of the conduit is complete. A 12 Fr Silastic Foley catheter is left in situ for 4 weeks after the surgery prior to commencing catheterization. Once the child and carers are happy with the enema procedure, the child can be discharged with the indwelling catheter, to return 4 weeks later to learn intermittent catheterization, which seldom takes longer than 48 hours. Occasionally, stoma revision is required, and this usually takes the form of a YV plasty. As patients will spend a considerable time sitting on the toilet, the use of padded seat covers is recommended to reduce the risk of pressure sores. If colic is persistent, the administration of mebeverine hydrochloride 30 minutes before the enema can help. If the enema does not produce a rapid result, the concentration of the phosphate can be increased in steps up to a full-strength enema, and in some patients this is used without a following washout. Phosphate toxicity has been encountered, particularly in younger patients, and it is of vital importance that if there is no response from the enema after 6 hours, no further phosphate is administered until a result is obtained. New techniques for construction of efferent conduits based on the Mitrofanoff principle. Despite our increased knowledge of the disease, significant complications continue to be associated with this process. Failure to pass meconium within the first 48 hours of life, complaints of constipation and, finally, symptoms of enterocolitis should always be followed by a complete clinical examination for Hirschsprung disease. Use of laparoscopy to facilitate both the diagnosis and the pull-through procedure has also become common. Full-thIckness rectal bIoPsy Suction rectal biopsy, because of its relative ease and low morbidity, has become the most established diagnostic tool for Hirschsprung disease. A sponge is placed in to the proximal rectal vault to prevent stool from entering the operative field. The child is placed in Trendelenburg to prevent spillage of stool in to the operative field. The feet are placed together (plantar surfaces adjoined) with a cotton roll, and both legs are suspended on an ether screen, or similar device. The superior aspect of the dentate line is identified and marked with a polyglactin suture (3/0), which is used for traction. Two additional polyglactin sutures are placed on the posterior wall of the rectum at 1 and 2 cm proximal to the dentate line. Bleeding can slightly obstruct the view at this point; however, by maintaining traction on the middle suture, the upper half of the rectum is incised with two smooth cuts of the scissors, each sweeping around one-half of the tissue suspended by the middle suture. The rectal defect is closed in a single, full thickness running or interrupted layer with an absorbable suture. Although a right transverse colostomy has been advocated by some surgeons as the initial procedure, the authors prefer a leveling colostomy. This allows for the determination of the aganglionic level at the time of the colostomy, facilitating the subsequent pullthrough. Use of laparoscopy, with serial seromuscular biopsies, has greatly facilitated the determination of the level of aganglionosis. Most diagnoses can be suspected based on the history alone, but confirmation is required by histopathologic examination of a suction rectal biopsy. The bowel proximal to the transition zone is normally dilated and has a diffuse hypertrophy of the muscular layer with no clearly distinguishable tenea. Each biopsy specimen is sent for frozen section, progressively moving more proximally until both ganglion cells, as well as a loss of hypertrophied nerve bundles, are seen. It is extremely important to begin the colostomy by placing numerous fine polyglactin sutures both to the peritoneum as well as to the fascia. It is occasionally helpful to perform intermittent dilatations of the proximal ostomy. The operation is generally performed when the child is 612 months of age with a weight of 10 kg. With the use of smaller endostapling devices, the procedure may also be performed primarily in the newborn period. It is necessary to do a rectal examination on the child before the pull-through to ensure that no residual stool is present. Preoperative broad spectrum antibiotics should be given just prior to the skin incision. Stockinettes are placed around each foot and a Foley catheter is inserted in the bladder after the patient has been prepared and draped. A hockey-stick or oblique incision is made incorporating the colostomy (if present). The bowel is mobilized proximal to the former colostomy and the splenic flexure is brought down, if necessary, to ensure adequate length for the pull-through. The distal end of the ganglionic bowel is labeled mesenteric and antimesenteric with a separate polypropylene and polyglactin suture.