Ramipril
General Information about Ramipril
Altace ought to be taken frequently for it to be efficient in controlling blood strain. If a dose is missed, you will want to take it as quickly as remembered. However, if it is nearly time for the following scheduled dose, don't take an extra dose to make up for the missed one.
Some common unwanted side effects that may happen while taking ramipril embody dizziness, tiredness, cough, and headache. These unwanted effects are typically mild and should subside as the physique adjusts to the medicine. However, in the event that they persist or turn into bothersome, you will need to seek the guidance of a health care provider. Rare however extra serious unwanted aspect effects could include issue respiration, swelling of the face, lips, tongue, or throat, and chest pain. If any of these happen, seek medical consideration immediately.
Unlike different drugs for hypertension, ramipril not solely helps to decrease blood pressure, but it additionally has further advantages. It has been shown to decrease the danger of heart assault, stroke, and demise in sufferers with a history of heart illness or those at excessive threat for it. This makes ramipril a priceless and commonly prescribed medicine for treating hypertension.
It is also necessary to watch your blood stress regularly while taking ramipril, as it might take a few weeks for the treatment to succeed in its full impact. It is not uncommon for medical doctors to additionally recommend way of life changes alongside medicine to handle hypertension, corresponding to common exercise, a nutritious diet, and limiting alcohol and salt intake.
Before starting ramipril, it is necessary to inform your doctor of any pre-existing circumstances or medications you could be taking. It is especially essential to discuss any historical past of liver or kidney illness, diabetes, coronary heart illness, or any allergy symptoms. This will help the doctor determine if ramipril is a safe and appropriate medicine for you.
In conclusion, ramipril, offered as Altace, is a generally prescribed medicine for treating high blood pressure, but it also has further benefits in decreasing the chance of coronary heart disease. It is necessary to comply with the beneficial dosage and seek the assistance of together with your physician to ensure its effectiveness and to handle any potential side effects. By working together with life-style adjustments, ramipril could be an effective tool in controlling blood pressure and minimizing the danger of significant health complications.
Ramipril, sold beneath the brand name Altace, is a medication used to treat hypertension (hypertension). It belongs to a class of drugs generally identified as ACE inhibitors, and works by enjoyable blood vessels and bettering blood move, which helps to lower blood pressure.
Ramipril can interact with other drugs, together with over-the-counter medicine and herbal supplements. It is important to tell your physician of all the medications you're taking to keep away from any potential complications.
High blood pressure, if left untreated, can lead to serious health consequences such as coronary heart disease, stroke, and kidney failure. Therefore, it is very important control it with the help of medications like ramipril.
Ramipril is available in tablet kind and is normally taken as quickly as a day, with or without food. The dosage will rely upon the individual's blood strain levels and response to the medicine, and it could be adjusted by a well being care provider over time.
If small blood pressure categories chart discount 2.5 mg ramipril overnight delivery, they usually regress postpartum, but they may also fibrose and require excision. Vascular lesions may bleed excessively when traumatized and are readily excised or ablated with a laser. Sturge-Weber syndrome (encephalofacial angiomatosis) is a rare congenital neurocutaneous condition characterized by a port-wine stain of the skin, typically in the ophthalmic and maxillary distributions of the trigeminal nerve. Patients present with bluish-purple plaques on the buccal mucosa and gingiva on the same side as the skin lesions. Abnormal vessels in the leptomeninges of the brain and choroid are the cause of seizures. The treatment is symptomatic and includes laser therapy to remove or lighten the skin and mucosal lesions, anticonvulsants for seizure control, symptomatic and prophylactic therapy for headache, and treatments to reduce intraocular pressure. Hereditary hemochromatosis results from an inherited autosomal-recessive disorder, while hemosiderosis may occur from multiple transfusions. Hereditary hemochromatosis is caused by increased absorption of dietary iron in the gut leading to iron accumulation in parenchymal organs and end-organ damage. Iron deposition in the form of hemosiderin and ferritin leads to skin bronzing, cirrhosis, hypopituitarism, diabetes mellitus, nephrogenic diabetes insipidus, and cardiomyopathy. Brown to gray diffuse macules of the palatal mucosa and gingiva occur in approximately 15% to 20% of patients. Poorly Healing or Nonhealing Extraction Sockets and Osteonecrosis After dental extractions, a blood clot is formed within 24 to 48 hours. The clot is replaced with granulation tissue, and bone formation is well established by 6 to 8 weeks and completed by 6 months. Local factors such as infection or cemento-osseous dysplasia that leads to bone sclerosis and poor vascularity may lead to a poorly healing or nonhealing socket, but several systemic conditions must also be considered. Diabetes mellitus Patients with poorly controlled type 1 diabetes mellitus are at risk for poorly healing sockets because these patients are prone to infections and more severe periodontal disease, which in itself may impair glycemic control. Conversely, treatment for severe periodontitis has shown to improve glycemic control. Studies in diabetic animals have shown that the formation of the collagenous framework in the tooth extraction socket is inhibited and that aberrant endothelial activation and impaired angiogenic response result in delayed socket healing and the development of dry socket. Paget disease usually occurs after the age of 55 years and typically affects the axial skeleton, especially the pelvis. The skull is involved in about 40% of patients, and involved bones enlarge over time. Enlargement of the maxilla and mandible may result in the development of diastemas of teeth and malocclusion. Later, cortical thickening develops and radiopacities form, resulting in a cotton woollike appearance. Patients with Paget disease are at higher risk of developing osteosarcoma (less than 1% of cases). Dentists should recognize the symptoms and signs of Paget disease and be aware that a dental extraction may be associated with postextraction bleeding and secondary osteomyelitis. Mild cases of Paget disease do not require treatment whereas patients with pain and severe involvement are treated with antiresorptive therapy. Osteopetrosis is a genetic heterogeneous group of heritable diseases of the bone characterized by osteoclastic dysfunction and osteosclerosis. Infection, osteonecrosis, and osteomyelitis may ensue after extractions due to the reduced blood supply. Bisphosphonates are potent inhibitors of osteoclast-mediated bone resorption and have been used in the management of multiple myeloma, bone metastases, and osteoporosis. Patients with osteoporosis who are prescribed intravenous bisphosphonates generally receive a single annual 5-mg infusion of zoledronic acid, compared with patients with myeloma or metastatic cancer to the bones who receive a 4-mg infusion monthly, usually for 24 months. Other risk factors include dental extractions, other dentoalveolar surgery, physiologic trauma, and odontogenic infections, although some cases are idiopathic. Radiographic findings are variable and may include altered bony trabeculae with mottled osteosclerotic changes, bone sequestra and osteolytic changes, thickening of the lamina dura and narrowed periodontal ligament space, and persistent rarefaction at the site of dental extractions (at least 6 months after extraction). Patients present with either painful or painless areas of exposed bone often on the mylohyoid ridge, tori, or nonhealing extraction sockets with exposed bone. Stages 2 and 3 are treated with antibiotics (amoxicillin with or without clavulanic acid, clindamycin, or metronidazole) for a 2to 4-week or 1- to 2-month course of therapy. Chlorhexidine or other antimicrobial oral rinses should be prescribed for all patients at any stage. If the patient has had substantial exposure to bisphosphonate therapy, endodontic therapy is preferable to extraction for nonmobile teeth that have good bone support; nonrestorable teeth can be decoronated. Contrary to earlier findings, current data show that surgical resection may lead to durable remission of disease. Denosumab binds to a molecule on the osteoclast, inhibiting its activity and thereby causing inhibition of bone resorption. A common scenario when such involved mobile teeth are extracted is that the socket fails to heal but is instead filled with fleshy soft tissue. Therefore, patients with hyposalivation are at risk of developing erythematous areas from friction; experience difficulty with eating, swallowing, taste, and speech; and are at a greater risk of caries and candidiasis. It is only a symptom and may or may not be associated with reduced saliva in the mouth.
The volume of radiation is usually minimized to include the recurrent disease bed while maximally sparing normal tissue thereby sparing morbidity arteria radicularis magna order ramipril 10 mg with visa. More modern and technologically advanced radiation delivery may offset the morbidity noted historically. In general, reactive feeding tube placement is preferred to prophylactic placement before therapy begins. These devices have been shown to be beneficial for patients who are thin, or have lost significant weight. They are not necessary for all patients, but if not placed, such patients must be assessed every 1 to 2 weeks for toxicity and weight loss. Hydration Radiation and chemoradiation leads to increased fluid loss, especially with severe mucositis, and/or with loss of normal taste or appetite. Patients should be assessed every 1 to 2 weeks for skin turgor, orthostatic blood pressure changes, lightheadedness on standing, or renal dysfunction (especially when platinum-based chemotherapy is used). Mucositis A significant number of patients receiving chemoradiation therapy will develop severe mucositis that impairs nutrition and causes severe pain. At the first sign of candidiasis, antifungal therapy should be instituted, topically and/or orally. A preparation containing an antifungal, anesthetic, and calcium carbonate suspension is useful. Narcotic pain control should be aggressive and patients should be taught to track pain severity and self-administer their narcotics before the peak of pain occurs. It is useful to use a transdermal administration route, using careful dose calculation based on the total use of short acting narcotic, plus a short-acting (liquid) narcotic to control pain. Radiation Dermatitis and Rash Mild radiation dermatitis is managed with a moisturizer during and after radiation. Cetuximab may cause an acneiform rash in the upper torso and face, which may become infected if not treated. Steroid-containing topical creams and minocycline are also helpful for a more severe rash (confluent in more than one body area). The rash often improves after the first few weeks, and may not be present in the radiation fields. Infusion of these agents should only be done when appropriate emergency equipment and trained personnel are available. Initial management typically includes saliva substitutes, oral mucosal lubricants, and frequent sips of water. Systemic cholinergic agonists can be considered for xerostomia that persists for more than 1 year after treatment completion. Late Dysphagia A minority of patients will have swallowing difficulties for several years or permanently, with attendant risk of aspiration and pneumonia. Swallowing therapy and potentially continued enteral nutrition with a percutaneous tube may be necessary for these patients. Serial dilatations of the oropharyngeal inlet and esophagus might be needed to deal with radiation- /surgery-related strictures. Dental Caries An increased risk of developing dental caries accompanies any change in salivary flow or composition. For this reason, any patient who has had head and neck radiation should have regular, frequent dental evaluations. Sequestrectomy coupled with longterm pentoxifylline has been reported to result in healing in most patients within 1 year. Hyperbaric oxygen has been used for many years, but was not found to be of benefit in a randomized clinical trial. Mobility Impairment Both surgery and radiation can cause fibrosis of soft tissues of the neck, impacting cosmesis and/or neck mobility. Treatment often includes physical therapy for neck stretching and strengthening and massage. Follow-Up Curative treatment of patients with head and neck cancer should be followed by a comprehensive head and neck physical examination every 1 to 3 months during the first year after treatment, every 2 to 4 months during the second year, every 3 to 6 months from years 3 to 5, and every 6 to 12 months after year 5. In patients treated nonoperatively, restaging imaging studies should be done approximately 12 weeks after completion of radiation therapy and then as needed for any symptoms or signs suggesting recurrence or second primary cancer. Neck dissection is warranted for incomplete response and equivocal findings on imaging. This approach resulted in equally good survival and was cost effective compared with planned neck dissections. After 3 years, a second primary tumor in the lung or head and neck is the most important cause of morbidity or mortality. Because of this risk, annual chest imaging, particularly in smokers, is recommended. Food and Drug administration for prevention of cervical cancer (bivalent or quadrivalent vaccines) in females and genital warts in males (quadrivalent vaccine), as well as for prevention of anal precancers (quadrivalent vaccine). Premalignant lesions occurring in the oral cavity, pharynx, and larynx may manifest as leukoplakia (a white patch that does not scrape off and that has no other obvious cause) or erythroplakia (friable reddish or speckled lesions). Presently, there is no effective chemoprevention for patients at risk for head and neck squamous cancer and chemoprevention outside a clinical trial is not recommended. Frequency and therapeutic implications of "skip metastases" in the neck from squamous carcinoma of the oral tongue. Intensity-modulated radiotherapy for locally advanced cancers of the larynx and hypopharynx. Occult primary head and neck squamous cell carcinoma: utility of discovering primary lesions. Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. Randomized trial of postoperative reirradiation combined with chemotherapy after salvage surgery compared with salvage surgery alone in head and neck carcinoma.
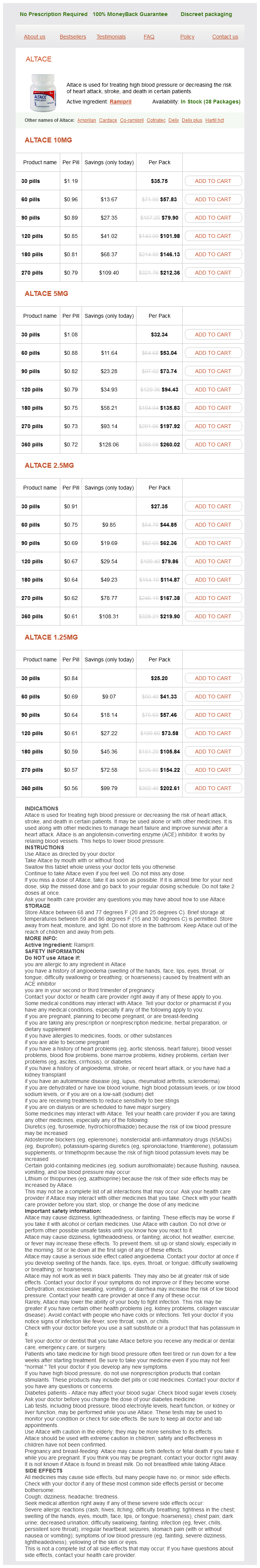
Ramipril Dosage and Price
Altace 10mg
- 30 pills - $35.75
- 60 pills - $57.83
- 90 pills - $79.90
- 120 pills - $101.98
- 180 pills - $146.13
- 270 pills - $212.36
Altace 5mg
- 30 pills - $32.34
- 60 pills - $53.04
- 90 pills - $73.74
- 120 pills - $94.43
- 180 pills - $135.83
- 270 pills - $197.92
- 360 pills - $260.02
Altace 2.5mg
- 30 pills - $27.35
- 60 pills - $44.85
- 90 pills - $62.36
- 120 pills - $79.86
- 180 pills - $114.87
- 270 pills - $167.38
- 360 pills - $219.90
Altace 1.25mg
- 30 pills - $25.20
- 60 pills - $41.33
- 90 pills - $57.46
- 120 pills - $73.58
- 180 pills - $105.84
- 270 pills - $154.22
- 360 pills - $202.61
Biopsy should be pursued depending on the suspected lesion with stereotactic or endoscopic approach in germinoma or tectal glioma and microsurgical techniques for open biopsy in other cases hypertension canada generic ramipril 2.5 mg buy on-line. Brain Metastases Brain metastases occur in 15% to 40% of patients with systemic cancer. Although the true incidence of metastatic brain tumors remains unknown, it is following an increasing trend likely due to better control of systemic cancer and prolonged survival. Aging is a factor risk and the most frequent primary tumor origin is lung, breast, melanoma, and colorectal. Hematological tumors constitute 10% of brain metastases and primarily affect the leptomeninges. Presentation is usually with focal neurologic deficits related to mass compression, edema, and increased intracranial pressure. From a neuroimaging point of view lesions are characteristically localized at the grey/white matter junction and are surrounded by significant edema with higher edema/tumor size ratio. Medical management usually comprise the use of oral steroids to decrease the edema at common dose range of dexamethasone 4 to 8 mg/day and up to 16mg/day for severe symptoms. One quarter of patients do present with seizure and antiepileptic treatment is indicated. There is no evidence based role for seizure prophylactic treatment, although short prophylactic treatment with a one week course and rapid tapering off scheme has been adopted for the perioperative period. Often there is an increased risk of venous thromboembolism partly due to chemotherapeutic agents use, and in high-risk patients, perioperative prophylaxis with heparin has reduced the related mortality without increasing the risk of intracranial haemorrhage. Depending on the primary tumor staging and grading, brain metastases treatment may encompass surgery, radiotherapy and in certain cases chemotherapy for chemosensitive tumors as small cell lung carcinoma, germ cell tumors, and lymphoid neoplasms. Interestingly, there is now evidence that brain metastases can be prevented by targeted therapy of the primary brain tumor. In patients with good prognosis, emphasis is placed on balancing treatment effectiveness against neurotoxicity and the goal of therapy has shifted from shortterm palliation to long-term survival and quality of life (QoL). Surgical treatment with removal of brain parenchyma adjacent to the metastatic lesion confers better local control than gross total resection. The pathologic confirmation of tumor-free resection margins provides rate of local recurrence comparable to standard gross total resection and adjuvant radiotherapy. Spinal Metastases Metastases of the spine most frequently involve vertebral elements and epidural space and arise from lung, breast, liver, skeletal, and prostate primary tumors. Management includes tailored approach depending on individual localization, clinical symptomatology, and previous treatments, and may include combination of steroids, surgery, radiation, and chemotherapies. Spinal cord compression because of these metastases to the spine with extension into the spinal canal represents a true oncologic emergency as neurologic deficits may not improve particularly if the compression results in vascular compromise to the spinal cord. Intradural metastases are far less common but are typically referred to as drop metastases as they are extramedullary and either compress the cord or invade into the spinal cord parenchyma. Neoplastic Meningitis Meningeal involvement can occur by local infiltration or by dissemination of tumor cells by the cerebrospinal flow. Treatment with focal radiation to areas of bulk disease or neurologic symptoms from involvement of cranial or spinal nerves may improve function. Radiation and chemotherapy regimens have been developed for most primary brain tumors and are being increasing refined by tumor type and recently molecular subtypes, underscoring the importance of accurate histologic and molecular classification. In all patients, realistic appraisal of treatment outcomes in the context of both short- and long-term toxicities highlights the need for systematic evaluation of patient outcomes to provide patients with cancer information necessary for informed decision making. Treatment of meningioma, including in cases with no further surgical or radiotherapy options. Integrated analysis of pediatric glioblastoma reveals a subset of biologically favorable tumors with associated molecular prognostic markers. Use of ifosfamide, carboplatin, and etoposide chemotherapy in choroid plexus carcinoma. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Inverse association between Prediagnostic IgE Levels and the risk of brain tumors: A systematic review and metaanalysis. Chromosome 17 alterations identify good-risk and poor-risk tumors independently of clinical factors in medulloblastoma. The potential impact of tumour biology on improved clinical practice for medulloblastoma: progress towards biologically driven clinical trials. Chromosomal alterations, prognostic factors, and targeted molecular therapies for malignant meningiomas. With the exception of thyroid cancer, endocrine tumors are often difficult to diagnose and treat effectively. They may cause morbidity and mortality through local and distant metastasis or through systemic effects caused by hormones produced by tumor cells. While relatively uncommon as a group, thyroid cancer has increased in incidence over the last decade more than any other malignancy. The National Cancer Institute has estimated that 62,450 new cases of thyroid carcinoma are diagnosed in the United States annually, accounting for approximately 1950 deaths. The incidence of thyroid carcinoma is now about 9 per 100,000, with approximately 2. Risk Factors the best-established risk factor for thyroid cancer is head and neck radiation exposure during childhood for diseases such as Hodgkin lymphoma; hereditary factors, family history of thyroid cancer and history of goiter or thyroid nodule, and/or preceding autoimmune thyroid disease are implicated in some patients as the cause of the increased risk of thyroid cancer. Autoimmune thyroid disease is more prevalent in women and this may explain why thyroid cancer is more common in women that in men. Thyroid cancer has been observed 20 to 25 years after radiation exposure among atomic bomb survivors, and in some regions of Japan the incidence of thyroid cancer in screened populations is as high as 0.