Rumalaya forte
General Information about Rumalaya forte
The anti-inflammatory and analgesic results of Rumalaya forte make it a super choice for treating various musculoskeletal issues like arthritis, osteoarthritis, gout, frozen shoulder, and different joint and muscle pains. Its immunomodulatory action helps to strengthen the immune system and reduce the chance of developing autoimmune disorders. It is also useful in treating sports injuries and post-surgical ache.
One of the advantages of Rumalaya forte is its pure composition, making it secure for long-term use without the danger of unwanted effects. It is also non-addictive and doesn't cause any withdrawal symptoms. This makes it appropriate for all age groups, including the elderly.
Rumalaya forte works by inhibiting the production of prostaglandins, which are liable for inflammation and pain. It also helps to improve the blood supply to the joints, selling the healing of damaged tissues. In addition, its anti-oxidant properties help to guard the joints from oxidative damage and additional degradation.
Rumalaya forte is a powerful herbal supplement that has been used for centuries to deal with varied musculoskeletal disorders. This Ayurvedic medicine has gained recognition in current times due to its potent anti-inflammatory and analgesic properties. It is a protected and efficient different to non-steroidal anti-inflammatory drugs (NSAIDs) and is known for its minimal side effects. In this article, we will talk about what Rumalaya forte is, its mechanism of motion, and its varied well being advantages.
In conclusion, Rumalaya forte is a potent anti-inflammatory analgesic with immunomodulatory action. Its pure composition and minimal unwanted effects make it a preferred choice for managing various musculoskeletal issues. It is a safe and effective different to NSAIDs and is suitable for long-term use. However, you will need to consult a doctor before beginning this or some other complement to ensure its safety and effectiveness for particular person well being needs.
This natural complement is on the market within the type of tablets, and the beneficial dose is one or two tablets twice daily after meals. It is advised to consult a healthcare skilled before taking the complement, especially for pregnant and lactating girls and those with pre-existing medical conditions.
Rumalaya forte is a mix of natural elements corresponding to Boswellia, Guggulu, Gokshura, Shilajeet, and Yasthimadhu. These ingredients work synergistically to reduce irritation, relieve ache, and enhance joint mobility. Boswellia, also identified as Shallaki, is wealthy in boswellic acids which have been found to have anti-inflammatory, analgesic, and anti-arthritic properties. Guggulu, generally generally recognized as Indian bedellium, has been used in traditional medication to reduce swelling and pain. Gokshura, or tribulus, is a pure diuretic and has been confirmed to be helpful in treating joint disorders. Shilajeet, also called mineral pitch, is a potent antioxidant that helps to reduce inflammation and enhance joint perform. Yasthimadhu, or licorice root, has anti-inflammatory exercise and has been used to treat joint problems in traditional medicine.
In patients with more severe infections muscle relaxant powder buy 30 pills rumalaya forte visa, fever, chills, malaise, nausea, and vomiting may develop. Women with severe pelvic pain tend to walk in a slightly bent-over position, holding their lower abdomen and shuffling their feet. Abdominal examination reveals lower quadrant tenderness, sometimes with rebound, and occasionally, there will be right upper quadrant tenderness resulting from gonococcal perihepatitis (Fitz-HughCurtis syndrome). Pelvic examination demonstrates bilateral adnexal tenderness as well as uterine fundal and cervical motion tenderness. The examination should be thorough, yet performed as gently and briefly as possible to avoid exacerbating a very painful condition. A catheterized urine specimen will be required when a vaginal discharge or bleeding is present. Under ideal transport conditions, gonorrheal culture is inexpensive, excellent, and, in some cases, as sensitive as nucleic acid amplification testing. However, when the maintenance of appropriate transport conditions is not possible, nonculture nucleic acid amplified testing is superior. Testing for Chlamydia has been revolutionized by the emergence of these nucleic acid amplification techniques, which has improved the sensitivity of disease detection by 25% to 30% compared with cultures. Older nonculture techniques, such as direct fluorescent antibody, enzyme immunoassay, and nonamplified nucleic acid hybridization, are even less sensitive than a culture. Determine the pH of any vaginal discharge, and make wet-mount examinations and Gram stains of endocervical secretions, looking for Candida organisms, Trichomonas organisms, leukocytes, and clue cells (see Chapter 95). Gram stain of the cervical specimen is not adequate for diagnosing gonorrhea in women. Perform pelvic ultrasonography if there is a suspected mass, severe pain, or a positive pregnancy test. Subtle findings may include only a history of abnormal uterine bleeding, dyspareunia, vaginal discharge, or cervical purulence. Prevention of long-term sequelae has been linked directly with immediate administration of appropriate antibiotics. When selecting a treatment regimen, consider availability, cost, patient compliance, and antimicrobial susceptibility. Also hospitalize when there is severe illness with septicemia or other serious disease, high risk for poor compliance, failed follow-up, or failure after 48 hours of the outpatient therapy outlined later. Transition to oral therapy from parenteral can start after 24 hours, with demonstrated clinical improvement. Patients who do not improve within this period usually require hospitalization, additional diagnostic tests, and possible surgical intervention. Sex partners should be treated empirically with regimens that are effective against both of these infections, regardless of the pathogens isolated from the infected woman. Patient-delivered treatment of sex partners was associated with a reduced risk for recurrent gonorrhea and/or chlamydia in a University of Washington (Seattle) study. This can be done with consideration of your population and local pattern of prevalence of disease. In one study, 15% to 23% of patients had one or more new infections, and 66% were asymptomatic. What Not To Do: Do not miss the more unilateral disorders, such as ectopic pregnancy, appendicitis, ovarian cyst or torsion, and diverticulitis. Early consultation by both a general surgeon and an obstetrician/gynecologist is sometimes necessary. Do not ignore pelvic symptoms if the patient has gonococcal perihepatic inflammation. Do not talk above the educational/comprehension level of the preteen and teenage patient. It should be kept in mind that the diagnosis and management of other common causes of lower abdominal pain. Gonorrheal and chlamydial infections are thought to initiate conditions that allow organisms from the lower genital tract to ascend in to the upper genital tract. The resulting polymicrobial infection includes facultative and anaerobic organisms. A variety of gram-positive and gram-negative aerobic and anaerobic pathogens, such as aerobic streptococci, Escherichia coli, Bacteroides fragilis, Proteus spp. It is usually amenable to medical therapy but requires surgical intervention in up to 25% of cases. Although all of the gonorrheal isolates in the United States are susceptible to cephalosporins, resistance to quinolones has developed. Laparoscopy is indicated in severe cases, if diagnosis is uncertain or there is inadequate response to initial antibiotic therapy. Nasraty S: Infections of the female genital tract, Prim Care 30:193203, vii, 2003. Simms I, Wharburton F, Weström L: Diagnosis of pelvic inflammatory disease: time for a rethink, Sex Trans Infect 79:491494, 2003. Profuse bleeding is generally defined as soaking a large sanitary pad or tampon every hour or two and continuing for more than 2 hours. Excessive menstrual bleeding is quantified typically as greater than 80 mL, with normal menstrual losses over a 5- to 7-day cycle on average of 30 to 45 mL. If the patient is deemed hemodynamically unstable, arrange for rapid transport to an acute care setting, such as an emergency department by ambulance. Uterine curettage is first-line therapy for the unstable patient with acute or prolonged uterine bleeding.
Suggested Readings American Gastroenterological Association: American Gastroenterological Association medical position statement: diagnosis and care of patients with anal fissure spasms before falling asleep cheap rumalaya forte online master card, Gastroenterology 124:233234, 2003. Brisinda G, Cadeddu F, Brandara F, et al: Randomized clinical trial comparing botulinum toxin injections with 0. Slawson D: Topical nifedipine plus lidocaine gel effective for anal fissures, Am Fam Physician 67:1781, 2003. Often, it is not until they are asked that they will describe infrequent bowel movements, straining at stooling, incomplete evacuation, hard or small stools, a blockage in the anal region, or the need for digital manipulation to enable defecation. They will have constipation (fewer than three bowel movements per week), diarrhea (more than three bowel movements per day), or alternating constipation and diarrhea. At the age of 6 weeks, infants with colic will begin having episodes of inconsolable crying that last more than 3 hours per day for more than 3 days per week and that continue longer than 3 weeks. The physical examination is benign, with normal vital signs and no jaundice, tenderness, masses, organomegaly, rectal bleeding, or other abnormalities, and the patient does not appear ill between the episodes of abdominal pain. A careful medication history should be obtained, because many commonly used drugs may cause constipation. Perform a complete physical examination, including rectal and/or pelvic examination, and a repeat abdominal examination after an interval. The rectal examination includes careful inspection and palpation for masses, anal fissures, inflammation, and hard stool in the ampulla. If the presentation is not clear or there is any concern about significant underlying disease, consider using diagnostic tests, such as urinalysis ( to help rule out renal colic or urinary tract infection), an erythrocyte sedimentation rate (a clue to infection or inflammation), abdominal radiographs ( to show free peritoneal air, bowel obstruction, or fecal impaction), and ultrasonography (for pyloric stenosis, malrotation and intussusception in children, or gallbladder and pelvic disorders in adults). Adult patients with a change in bowel habits or hemoccult positive stool should be referred for colonoscopy to assess for malignancy. If simple constipation is the problem and there is obstructing stool on rectal examination, disimpact the rectum by pulling out hard stool (scybala), and follow with one oil retention enema. For dry, obstipated feces, repeated tap-water enemas or phosphate enemas should be administered once or twice daily until clear. Disimpaction by the oral route, using medication, is noninvasive and more easily accepted by adolescents, who will often be reluctant to receive enemas. If there is no mechanically obstructing fecal impaction, this can also be done for adults. Magnesium citrate (Citro-Mag), 150 to 300 mL given once or divided doses for those 7 to 12 years old. For pediatric patients younger than 6 years, 2 to 4 mL/kg given once or in divided doses. Disimpaction by means of a combination of the rectal route and the oral route has been shown to be effective. Instruct the patient to return if symptoms do not resolve over the next 12 to 24 hours or to return immediately if the pain worsens. Instruct the patient that the recommended amount of dietary fiber is 20 to 35 g per day. Suggest adding bulk fiber, 20 to 35 g total fiber intake per day, in the form of bran, psyllium (Metamucil), methylcellulose (Citrucel), or calcium polycarbophil (FiberCon tablets) for prophylaxis. In general, patients with inadequate fiber intake should be advised (with the help of a dietitian) to increase their intake of natural fiber with fruit and vegetable servings. When possible, medications that may be constipating should be discontinued or replaced. These medications include narcotic analgesics, antacids containing aluminum and calcium, antidepressants, diuretics, nutritional supplements such as iron and calcium, anticonvulsants, antispasmodics, antiparkinson drugs, antihypertensive agents such as calcium channel blockers, and sedatives. In recent years, the use of over-the-counter polyethylene glycol 3350 without electrolytes (MiraLax), (17 g [1 heaping tablespoonful] of powder dissolved in 8 oz of water, juice, soda, coffee, or tea once daily, titrated to effect with a maximum of 34 g per day) has become increasingly popular. Because it is virtually tasteless, it has led to better compliance with treatment. Additionally, bisacodyl (Dulcolax), 5 to 15 mg as single adult dose, or senna (Senokot), 15 mg once daily, are stimulant laxatives that can be given at bedtime and are available over the counter. Both sorbitol and senna are less costly than lactulose and have been shown to be at least as efficacious, if not better. Functional constipation in infants and toddlers is defined as at least 2 weeks of scybalous, pebble-like, hard stools-or firm stools two or fewer times per week-in the absence of structural, endocrine, or metabolic disease. Constipation in infants and preschool children is usually treated first with sorbitolcontaining juices, such as prune, pear, and apple juice; the addition of pureed fruits and vegetables; formula changes; or treatment with a food product with a high sugar content, such as barley malt extract or corn syrup. If, despite these dietary changes, the stool is still hard and painful to evacuate, osmotic laxatives, such as milk of magnesia, 0. In addition, avoid enemas and stimulant laxatives, such as senna or bisacodyl, in infants. Dietary interventions such as a lactose-free diet, restriction of carbohydrates, avoidance of gluten, and avoidance of foods that produce gas may be undertaken. If there is weight loss, anemia, occult blood in the stool, abdominal distension or mass, or a family history of colon cancer, refer the patient for colonoscopy and gastroenterology consultation. For infant colic (defined as crying for a minimum of 3 hours daily 3 days per week for the previous 3 weeks, without weight loss, vomiting, or diarrhea), there is no "magic bullet. You may instruct the parents to administer for infants, 2 mL of 24% solution of sucrose in distilled water and for neonates, 0. If this is not successful, a higher concentration of sucrose may be more effective.
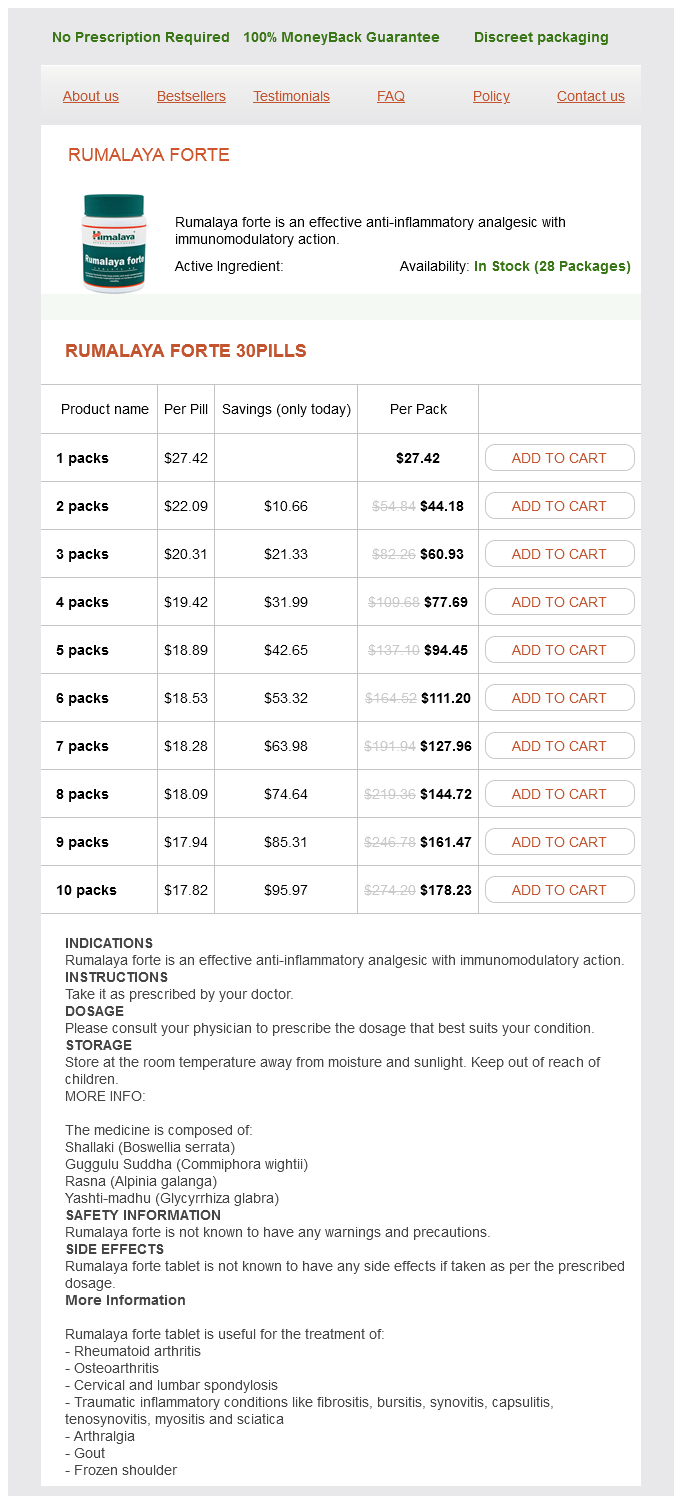
Rumalaya forte Dosage and Price
Rumalaya forte 30pills
- 1 packs - $27.42
- 2 packs - $44.18
- 3 packs - $60.93
- 4 packs - $77.69
- 5 packs - $94.45
- 6 packs - $111.20
- 7 packs - $127.96
- 8 packs - $144.72
- 9 packs - $161.47
- 10 packs - $178.23
Either azithromycin iphone 5 spasms generic 30 pills rumalaya forte fast delivery, 500 mg/d, or levofloxacin, 750 mg/d, are effective and welltolerated agents. This toxin-mediated diarrheal disease of the colon is almost invariably associated with recent or concurrent use of antimicrobial therapy. The spread of this strain may be owing to resistance to newer fluoroquinolones, whereas the apparent increase in virulence may result from dysregulation of toxin production. Tissue culture cytotoxin assay for toxin B is appreciably more sensitive but is not a rapid test, is expensive, and is not widely available. If the diarrhea is trivial and the offending antimicrobial agent can be stopped, resolution of diarrhea occurs in approximately 90% of patients without significant risk of relapse or recurrence. If the illness is mild to moderate (high fever, marked leukocytosis, and abdominal pain or tenderness are absent), then treatment with metronidazole is appropriate. Intravenously administered metronidazole penetrates the colonic lumen poorly and has not been established as reliably effective therapy for C. Fidaxomicin was not found to be superior to oral vancomycin but did have a somewhat lower relapse rate. Surgical consultation for consideration for colectomy is indicated with clinical evidence of progressive toxicity, radiographic evidence of progressive colonic dilation, or concern regarding loss of bowel wall integrity. Generally, retreatment is effective, although multiple relapses are not uncommon and may require a tapering schedule of drug. The profoundly immunosuppressed host, particularly if there is prolonged neutropenia, is at risk for infection by a variety of fungi, many of which rarely cause infection in healthy hosts. Some fungi cause infection in humans so rarely that identification of genus and species by a clinical microbiology laboratory may not be possible, and if identified by the laboratory, they may not be familiar, even to many clinically astute infectious diseases clinicians. In this section is a review of the more common fungal pathogens, rather than an encyclopedic review of the literature. Recovery of "nonpathogenic" fungi (or members of other classes of "nonpathogenic" microorganisms) from normally sterile body fluids, such as spinal fluid or blood, or from biopsy samples should prompt the clinician to consider that "nonpathogenic" organism might be a pathogen. Unfortunately, the greatest problem faced by clinicians is the inability to detect fungal infection in neutropenic patients. Infection by molds (generally a phenomenon that occurs after a more prolonged period of neutropenia) is far more difficult to diagnose, cultures are typically negative, and empiric therapeutic regimens simply cannot cover all possibilities without incurring unacceptable toxicity. The three major classes of antifungal agents that are useful in the patient with neutropenia and persistent fever are echinocandins, triazoles, and amphotericin B (AmB) preparations. Although the greatest clinical experience is with caspofungin, many experts believe these three agents have similar antifungal activities and toxicities. The echinocandins have excellent in vitro activity against most species of Candida (including fluconazole-resistant C. Triazoles are clinically useful antifungal agents that have substantially differing spectra of activity, adverse effects, and potential for drugdrug interactions. In the past, fluconazole had been considered an acceptable alternative to AmB at institutions in which infections with certain Candida species (C. The main value of fluconazole in neutropenic patients is for treatment of mucocutaneous Candida infection and systemic infection documented to be caused by C. Its main clinical utility is against the agents of histoplasmosis and blastomycosis. It is the most useful of the triazoles for empiric and pathogen-specific treatment of fungal infection in neutropenic patients. The potential for drugdrug interactions can be a problem with the use of voriconazole. The most common adverse reactions are several different types of visual disturbances that usually do not require discontinuation of therapy and skin reactions. In selected patients with appreciably impaired renal function, a change to oral therapy with voriconazole may be feasible. Additional study of this agent is needed to define its role in treatment of fungal infections in cancer patients. Of importance, a number of important drugdrug interactions involve voriconazole and the other triazoles. Most of these interactions involve cytochrome P450 isoforms and may result in significantly increased or decreased concentrations of voriconazole or of the interacting drug, resulting in either potential toxicity or lack of efficacy, respectively. In neutropenic patients, this concern is heightened by the frequent concomitant use of nephrotoxic chemotherapeutic agents and antimicrobial agents. Their major drawbacks have been other potential side effects and their much greater cost. Reasonably clear guidelines have been developed for antifungal therapy early in the course of neutropenia, largely because the greatest concern is for disseminated candidiasis. With prolonged broad-spectrum antibacterial therapy and empiric antifungal therapy, increasing opportunity and selective pressure tend to result in unusual infections. This makes microbiologic diagnosis of infection imperative and may require invasive procedures to procure biopsy material for culture and fungal staining. The strategy for providing empiric antifungal therapy in cancer patients with neutropenia is based on the following principles: 1. During the first several days of neutropenic fever, the likely pathogens are bacteria; diagnostic approaches and empiric treatment, therefore, are not focused primarily on fungal pathogens. During the first 4 to 7 days of neutropenic fever, the fungal pathogens most likely to be encountered are Candida spp. The echinocandins and newer triazoles have excellent in vitro activity against most Candida spp.