Tadacip
General Information about Tadacip
Tadacip� is a medicine manufactured by Cipla, a leading pharmaceutical firm in India. It is an alternative to the well-known brand Cialis, which is also used to treat ED. Both Tadacip� and Cialis include the energetic ingredient tadalafil, which belongs to a class of medication known as phosphodiesterase sort 5 (PDE5) inhibitors. Tadalafil works by rising blood move to the penis, serving to to achieve and preserve an erection.
One of the main benefits of Tadacip� is its affordability. As a generic medicine, it is significantly cheaper than the model name model Cialis, making it accessible to a wider population. This has been a game-changer for many males who beforehand couldn't afford ED therapy.
In addition to its convenience, Tadacip� has been confirmed to be a secure and effective therapy for ED. In a examine revealed within the Journal of Sexual Medicine, tadalafil was discovered to significantly enhance erectile function, as properly as the overall sexual satisfaction of males with ED. Another research showed that tadalafil was well-tolerated and had a low incidence of unwanted side effects.
In conclusion, Tadacip� from Cipla is a highly effective and inexpensive therapy for male impotence. Its day by day dosing choice, low incidence of unwanted aspect effects, and skill to improve signs of BPH make it a well-liked alternative among men seeking ED treatment. With its benefits and proven outcomes, Tadacip� provides hope and a renewed sense of confidence to those battling erectile dysfunction.
For millions of males all over the world, erectile dysfunction is usually a serious and distressing concern. It is estimated that as much as 52% of males over the age of forty expertise a point of impotence, also referred to as erectile dysfunction or ED. Thankfully, medical science has evolved to supply effective treatments for this situation, making it potential for men to regain their sexual perform and confidence. One such therapy is Tadacip�.
As with any treatment, there are nonetheless some precautions to consider earlier than taking Tadacip�. It shouldn't be used in mixture with nitrate medications, as this can cause a harmful drop in blood stress. It is also not really helpful for men with severe liver or kidney disease, in addition to those with a history of cardiovascular disease.
While Tadacip� is primarily used for treating male impotence, it has also been proven to improve symptoms of benign prostatic hyperplasia (BPH). BPH is a standard condition in men over the age of fifty, the place the prostate gland becomes enlarged and causes problem with urination. Tadalafil might help to chill out the muscular tissues within the prostate and bladder, making it easier to urinate.
What units Tadacip� apart from different ED treatments is that it could be taken every day, regardless of sexual activity. This is particularly useful for males who have a extra lively sex life, as they do not have to worry about timing their treatment before sexual activity. Tadacip� is out there in 2.5mg and 5mg tablets, making it a suitable possibility for both day by day and as-needed use.
Additional cardiac anomalies include a right-sided aortic arch in up to 25% of patients natural erectile dysfunction pills reviews discount tadacip 20 mg without a prescription. An anomalous left anterior descending artery originating from the right coronary cusp and crossing over the right ventricular outflow tract is seen in 10% of cases. With pulmonary atresia, pulmonary blood flow occurs through aortic to pulmonary collaterals. Adequate pulmonary blood flow is ensured by reconstruction of the distal pulmonary artery bed. Complete repair in childhood yields a 90 to 95% 10-year survival rate with good functional results, and 30-year survival rates may be as high as 85%. Some degree of pulmonary insufficiency is common, particularly if a patch has been inserted at the level of the pulmonary valve or if a pulmonary valvotomy has been performed. Patients may be asymptomatic or may have symptoms related to long-term complications after surgical repair. Symptoms can reflect residual right ventricular pressure or volume overload or arrhythmias at rest or with exercise. Angina can occur in a young patient if surgical repair has damaged an anomalous left anterior descending artery as it courses across the right ventricular outflow tract. On physical examination, a right ventricular impulse is often felt as a result of residual pulmonary insufficiency or stenosis. Ventricular arrhythmias are common after repair, with an incidence of sudden death as high as 5%. The most common finding after repair is complete right bundle branch block, which is seen in 80 to 90% of patients. The chest radiograph typically shows an upturned apex with a concave pulmonary artery segment giving the classic appearance of a boot-shaped heart. The apex is persistently upturned, although the pulmonary artery segment is no longer concave. Echocardiography can confirm the diagnosis and document intracardiac complications in repaired and unrepaired patients. Magnetic resonance imaging can accurately document stenosis in the distal pulmonary artery bed. Cardiac catheterization is reserved for patients in whom operative or reoperative treatment is contemplated or in whom the integrity of the coronary circulation needs to be verified. Patients with a change in exercise tolerance, angina, or evidence of rightsided heart failure and those with symptomatic arrhythmias or syncope should be referred for complete evaluation. Patients should be seen yearly by an adult congenital heart specialist for assessment of right ventricular function, pulmonary valve dysfunction, and arrhythmia. Sudden cardiac death can occur in 3 to 6% of patients observed between 20 and 30 years, sometimes despite favorable hemodynamics. In simple transposition of the great arteries, the atria and ventricles are in their normal positions, but the aorta arises from the right ventricle, and the pulmonary artery arises from the left ventricle. When the aorta is anterior and rightward with respect to the pulmonary artery, as is most common, D-transposition is present. The native anatomy has the pulmonary and systemic circulations in parallel, with deoxygenated blood recirculating between the right side of the heart and the systemic circulation, whereas oxygenated blood recirculates from the left side of the heart to the lungs. Subpulmonary obstruction of the left ventricular outflow tract occurs in 10 to 25% of cases. The arterial switch operation transects the aorta and pulmonary artery above their respective valves and switches them to become realigned with their physiologic outflow tracts and appropriate ventricles. The proximal coronary arteries are translocated from the sinuses of the native aorta to the neoaorta (native pulmonary artery). The 22-year survival rate of patients with transposition of the great arteries who underwent operation between 1990 and 2009 is 93%. Long-term complications include neoaortic regurgitation, supravalvular stenosis, and coronary artery complications. When patients of all ages are considered together, 10-year survival rates vary from 60 to 70%. Late deaths are due to reoperation, arrhythmia, ventricular failure, proteinlosing enteropathy, and liver dysfunction. In partial anomalous pulmonary venous return, one or more but not all four pulmonary veins are not connected to the left atrium. In total anomalous pulmonary venous return,8 all the pulmonary veins connect abnormally to either the right atrium or one of the systemic veins above or below the diaphragm. Concurrent obstruction of the pulmonary veins is present when drainage occurs below the diaphragm and variable when drainage occurs above it. In cor triatriatum, the pulmonary veins drain into an accessory chamber that is usually connected to the left atrium through an opening of variable size. The hemodynamic consequences are determined by the size of this opening and are similar to those of mitral stenosis. In dextrocardia, the heart is on the right side of the thorax with or without situs inversus. When the heart is right sided with inverted atria, the stomach is right sided, and the liver is left sided, the combination is dextrocardia with situs inversus. The heart sounds are louder on the right side of the chest, and the liver is palpable on the left. The chest radiograph shows a right-sided cardiac apex with a lower left hemidiaphragm and a right-sided stomach bubble. An echocardiogram should be performed to ensure that intracardiac anatomy is normal. When dextrocardia with situs solitus occurs, the ventricles are inverted but not the viscera and therefore not the atria. In mesocardia, the heart is centrally located in the chest with normal atrial and visceral anatomy.
Antibiotics modestly shorten the duration of the exacerbation impotence jelly best tadacip 20 mg, with no significant increase in toxicity, compared with placebo; the impact of antibiotics on the subsequent emergence of resistant organisms is not known. If patients with early acute lung injury can be identified prior to the need for positive-pressure ventilation, they can be treated with strategies, such as high-flow nasal oxygen, that might reduce the progression of their acute respiratory failure. The organisms vary widely, ranging from gram-negative and gram-positive bacteria and viruses. It can be difficult to determine whether pneumonia is diffuse, with endobronchial spread involving most of the lungs, or whether localized pneumonia has precipitated a sepsis syndrome, with secondary injury to other parts of the lung. Pulmonary thromboembolism must also be considered, particularly if no other cause of acute respiratory failure is identified. In general, if the patient is alert and is able to cooperate with treatment, mechanical ventilation often is not necessary. The severity of the underlying disease and the severity of the acute precipitating illness are important determinants of hospital survival. Hospital mortality is higher if the respiratory failure is associated with a pH lower than 7. These oxygenation categories require positive-pressure ventilation with at least 5 cm H2O positive end-expiratory pressure. Such early acute lung injury can be diagnosed in spontaneously breathing patients who have bilateral pulmonary infiltrates and in whom the inspired Fio2 can be estimated and the Pao2 measured. Ultrastructural studies with electron microscopy usually show endothelial and alveolar epithelial injury. Routine histology shows acute inflammation, usually with neutrophils predominating in the alveolar edema fluid. Hyaline membranes are present in some but not all patients, similar to those seen in premature infants with infant respiratory distress syndrome, presumably related to a procoagulant environment in the injured alveoli. Large-molecular-weight plasma proteins, including fibrinogen, accumulate, and inflammatory factors lead to fibrin deposition. The result is microatelectasis, which may be associated with impaired immune function. Initially, the Paco2 is low or normal, usually associated with increased minute ventilation. The initial abnormalities in oxygenation are thought to be related to alveolar flooding and collapse, which create a physiologic shunt. As the lung injury progresses, especially in patients who require ventilatory support, fibroproliferation may develop; the lungs (including alveoli, blood vessels, and small airways) remodel and scar, with a loss of microvasculature. In some patients, these changes may lead to pulmonary hypertension and increased pulmonary dead space; marked elevations in minute ventilation are sometimes required to achieve a normal Paco2, even as oxygenation abnormalities are improving. The presenting clinical picture is dominated by respiratory distress and the accompanying laboratory findings of severe hypoxemia, tachypnea, an increase in minute ventilation, and generalized alveolar infiltrates or opacities on the chest radiograph. The clinical presentation may also reflect manifestations of the underlying disease process, such as severe sepsis with hypotension and other manifestations of systemic infection. Although the findings are more commonly associated with the type of pulmonary edema as listed, they do not have high positive or negative predictive value. The differential diagnosis of pneumonia (Chapter 91) should be carefully considered, including determining whether the patient is immunosuppressed and, as a result, susceptible to a wider variety of infectious agents. Viral pneumonia from influenza (Chapter 340), respiratory syncytial virus (Chapter 338), or other viruses should be considered. If the patient has an abdominal source of infection, then appropriate diagnostic, radiologic, and surgical approaches are needed to establish a diagnosis and drain the infection. Any coexisting left heart failure or intravascular volume overload should be treated promptly (Chapter 53). On the basis of one clinical trial, the early use of cisatracurium besylate (15 mg rapid infusion followed by 37. The primary principle of a conservative fluid strategy is to achieve a daily net negative fluid balance of 0. Measurement of pulmonary artery or central venous pressure is not of major value for guiding fluid balance in most cases. Cardiomegaly Central or basilar infiltrates; peribronchial and vascular congestion Septal lines (Kerley lines), air bronchograms (25%), pleural effusion Pulmonary capillary wedge pressure > 18 mm Hg, cardiac index < 3. Management of acute respiratory failure from acute lung injury and acute respiratory distress syndrome. Case-fatality rates are 30 to 50% and are highly dependent on disease severity, the underlying predisposing condition, and the presence of comorbid diseases. Based on the degree of hypoxemia (mild, 200 mm Hg < Pao2/Fio2 < 300 mm Hg; moderate, 100 mm Hg < Pao2/Fio2 < 200 mm Hg; and severe, Pao2/ Fio2 < 100 mm Hg), inpatient mortality rates are about 27%, 32%, and 45%, respectively, not including patients with severe underlying conditions, such as end-stage cancer. Acute Respiratory Failure without Lung Disease Acute respiratory failure without pulmonary abnormalities (see Table 96-2) develops in patients with depressed ventilatory drive secondary to central nervous system dysfunction and in patients with severe neuromuscular disease. The prototypical patient with suppressed ventilatory drive has taken an overdose of a sedative or tranquilizing medication (Chapter 102). The prototypical patient with neuromuscular disease has Guillain-Barré syndrome (Chapter 392). In the case of a patient with a sedative overdose, the threshold for intubation with mechanical ventilatory support should be low because this temporary condition is quickly reversible when the responsible drug is eliminated. In addition, such a patient may require intubation for airway protection against aspiration of gastric contents regardless of whether acute respiratory failure has developed.
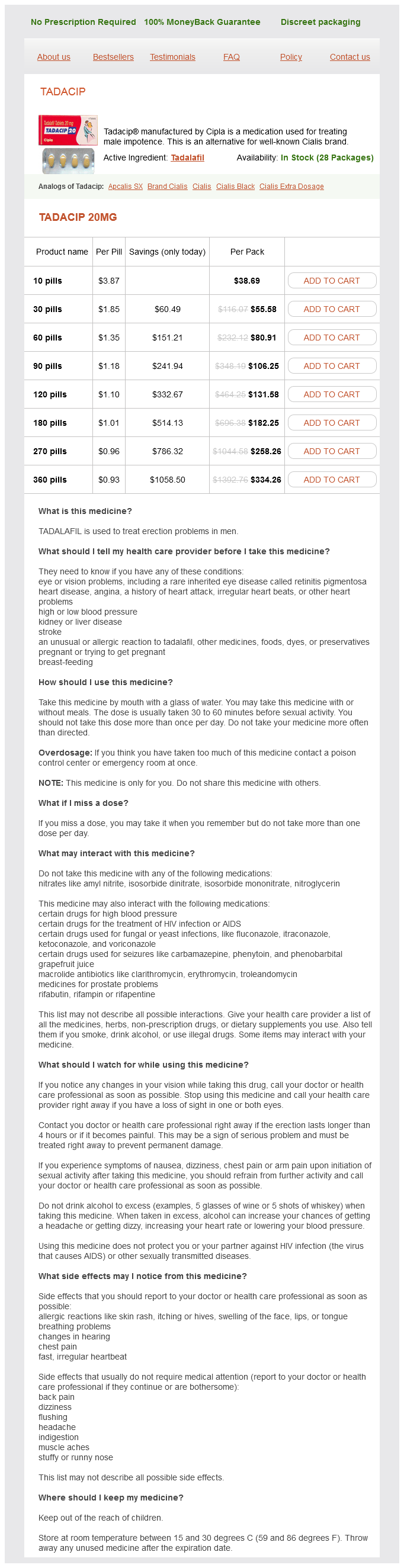
Tadacip Dosage and Price
Tadacip 20mg
- 10 pills - $38.69
- 30 pills - $55.58
- 60 pills - $80.91
- 90 pills - $106.25
- 120 pills - $131.58
- 180 pills - $182.25
- 270 pills - $258.26
- 360 pills - $334.26
Hydralazine and isosorbide dinitrate can also be used as additional treatment in non-African Americans who remain symptomatic with other proven therapies erectile dysfunction doctors in orlando order cheap tadacip on-line. The main dose-limiting adverse effects of hydralazine and isosorbide dinitrate are headache and dizziness. A rare adverse effect of higher doses of hydralazine, especially in slow acetylators, is a systemic lupus erythematosuslike syndrome (Chapter 250). Although this agent may have beneficial anti-inflammatory and antiarrhythmic effects, its current role in the treatment of heart failure is uncertain, especially because trials in survivors of acute myocardial infarction have not shown benefit (Chapter 64). In addition, digoxin is thought to enhance parasympathetic and reduce sympathetic nervous activity as well as to inhibit renin release. Clinical Benefits Other treatments have been tested in randomized trials and have been shown to have a neutral. A11 Some therapies that are of proven value for cardiovascular conditions that underlie or are associated with heart failure are of uncertain benefit (antiplatelet treatment, Chapter 76) or do not improve outcomes (statins, Chapter 195) in patients with persistent, symptomatic heart failure. Newer direct-acting oral anticoagulants or warfarin are indicated in patients with atrial fibrillation to reduce the risk for thromboembolism, unless patients have contraindications to their use (Chapter 58). Anticoagulants may also be used in patients with evidence of intracardiac thrombus. A12 the many interactions of warfarin with other drugs, including some statins and amiodarone (Chapter 76), must always be considered. The nonvitamin K oral anticoagulants are contraindicated in patients with severe renal impairment and should be given at a reduced dose in patients with less severe impairment (Chapter 76). Vaccination against influenza and pneumococcal infection is advised (Chapter 15) in all patients with heart failure because these infections can lead to severe clinical deterioration. In patients in sinus rhythm, the addition of digoxin can be considered if heart failure remains symptomatic despite standard treatment with a diuretic and three diseasemodifying drugs. However, digoxin has not been as well studied and may not be as safe as ivabradine when used in conjunction with contemporary therapies. In patients with atrial fibrillation, digoxin may be used at an earlier stage if a -blocker fails to control the ventricular rate during exercise (Chapter 58). Digoxin can also be used to control the ventricular rate when -blocker treatment is being initiated or up-titrated. If the effect of digoxin is needed urgently, loading with 10 to 15 µg/kg lean body weight, given in three divided doses 6 hours apart, may be used. Monitoring of the serum digoxin concentration is recommended because of the narrow therapeutic window. A steady state is reached 7 to 10 days after treatment is started; blood should be collected at least 6 hours (and ideally 8 to 24 hours) after the last dose. Digoxin can cause anorexia, nausea, arrhythmias, confusion, and visual disturbances, especially if the serum concentration is above 2. The dose of digoxin should be reduced in elderly patients and in patients with renal dysfunction. Other Pharmacologic Issues Refractory Heart Failure and Pulmonary Edema Hydralazine and Isosorbide Dinitrate Mechanism of Action Hydralazine is a powerful direct-acting arterial vasodilator. Its mechanism of action is not understood, although it may inhibit enzymatic production of superoxide, which neutralizes nitric oxide and may induce nitrate tolerance. Nitrates dilate both veins and arteries, thereby reducing preload and afterload by stimulating the nitric oxide pathway and increasing cyclic guanosine Patients presenting with acute heart failure include those who develop heart failure de novo as a consequence of another cardiac event, usually a myocardial infarction,6 and those who present for the first time with decompensation of previously asymptomatic and often unrecognized cardiac dysfunction (patients previously in stage B, a transition with profound prognostic implications). However, because of frequent recurrences, most episodes of decompensation occur in patients with established, chronic heart failure that has worsened as a result of the unavoidable natural progression of the syndrome, with an intercurrent cardiac. Although it is not always identified, searching for a reversible precipitant is an important aspect of the initial therapy plan (Table 53-6). Many patients with decompensated heart failure experience worsening over a period of days or weeks before presenting to their doctor. Most patients with decompensated heart failure require admission to the hospital, especially if pulmonary edema is present. The principal goals of management of this heterogeneous group of patients are to relieve symptoms, the most important of which is extreme dyspnea, and to maintain or to restore vital organ perfusion. A13 An intravenous opiate may also be used cautiously in selected patients to relieve anxiety and distress. Noninvasive ventilation using a tight-fitting mask to provide positive-pressure ventilation reduces respiratory distress and metabolic disturbances more rapidly than standard oxygen therapy but has not reduced short-term mortality. It can be difficult to determine whether atrial fibrillation is a primary cause of acute pulmonary edema or secondary to it. Acute mechanical problems include ventricular septal rupture and mitral valve papillary muscle rupture. An echocardiogram should be performed as soon as possible, especially in a patient without a prior diagnosis of heart failure/other relevant heart disease. Endotracheal intubation and invasive mechanical ventilation should be considered in patients with persisting hypoxemia and physical ventilatory exhaustion. Start at a dose of 10 µg/min and double every 10 minutes according to response and tolerability (usually dose up-titration is limited by hypotension). Percutaneous coronary intervention or coronary artery bypass grafting (Chapter 65), as appropriate, is indicated for relief of angina. The extent of ischemia and residual myocardial viability can be determined by noninvasive assessments such as dobutamine echocardiography (Chapter 49), magnetic resonance imaging (Chapter 50), and positron emission tomographic scanning (Chapter 50) in patients with impaired left ventricular ejection fraction. A19 the net benefit was not apparent until approximately 2 years after randomization because of the perioperative mortality related to surgery.