Tranexamic Acid
General Information about Tranexamic Acid
While Tranexamic Acid is mostly well-tolerated, there are some potential side effects that should be thought of. These embody nausea, diarrhea, headache, and dizziness. In rare circumstances, allergic reactions can also occur. It is necessary to consult a healthcare professional if any opposed unwanted side effects are skilled.
In conclusion, Tranexamic Acid, or Cyklokapron, is a drugs generally used for the short-term management of bleeding in individuals with hemophilia. Its position in managing extreme bleeding throughout dental extraction procedures has proven to be notably beneficial. While it doesn't cure hemophilia, Tranexamic Acid is a useful tool in helping individuals with this condition reside regular, wholesome lives. If you or a loved one has hemophilia, communicate to a healthcare professional about the use of Tranexamic Acid as a half of a complete remedy plan.
Tranexamic Acid is on the market in the form of tablets, injections and mouthwashes. The dosage and technique of administration will depend upon the individual’s situation and the severity of their bleeding. It is necessary to notice that while this treatment can successfully control bleeding, it does not treat the underlying cause of hemophilia. Therefore, it's usually used in mixture with other remedies.
In addition to getting used for hemophilia, Tranexamic Acid is also commonly used within the field of dentistry. One of its major makes use of is throughout dental extraction procedures. These can be particularly challenging for individuals with hemophilia, as they're at a better threat of excessive bleeding. By administering Tranexamic Acid, dentists can successfully manage and management bleeding during and after the process, reducing the risk of issues.
Tranexamic Acid is classified as an antifibrinolytic agent, which means it works by inhibiting the exercise of plasmin - a substance that dissolves blood clots. By doing so, it helps to maintain the clot in place, stopping additional bleeding. In individuals with hemophilia, this can be extraordinarily helpful in controlling bleeding, as their blood is unable to kind clots by itself.
Tranexamic Acid, also called Cyklokapron, is a drugs commonly used for the short-term management of bleeding in people with hemophilia. This drug works by stopping the breakdown of blood clots and controlling excessive bleeding, particularly throughout dental extraction procedures.
Hemophilia is a genetic dysfunction in which an individual’s blood is unable to clot properly. This can result in severe and prolonged bleeding, especially in response to injury or surgery. While there's presently no remedy for hemophilia, medicines such as Tranexamic Acid can help manage its symptoms and forestall issues.
Ablation of perivascular hepatic malignant tumors with irreversible electroporation treatment lyme disease tranexamic 500mg without a prescription. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Percutaneous radiofrequency ablation versus repeat hepatectomy for recurrent hepatocellular carcinoma: a retrospective study. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Local radiotherapy as a complement to incomplete transcatheter arterial chemoembolization in locally advanced hepatocellular carcinoma. Stereotactic body radiotherapy for small hepatocellular carcinoma: a retrospective outcome analysis in 185 patients. Stereotactic body radiation therapy for hepatocellular carcinoma: prognostic factors of local control, overall survival, and toxicity. Treatment of unresectable hepatocellular carcinoma with use of 90Y microspheres (TheraSphere): safety, tumor response, and survival. Doxorubicin plus sorafenib vs doxorubicin alone in patients with advanced hepatocellular carcinoma: a randomized trial. Borad introduction the biliary tract or the biliary drainage system includes the intraand extrahepatic bile ducts and the gallbladder. Cancers associated with the biliary tract may be associated with biliary tract epithelia along the entire biliary tract from the intrahepatic ductules to the ampulla of Vater. Cholangiocarcinomas are cancers of the biliary tract that are associated with the intrahepatic or extrahepatic bile ducts. The term cholangiocarcinoma encompasses three distinct tumor types that vary in their risk factors, presentation, natural history, and management. In addition to cholangiocarcinomas, cancers such as gallbladder cancer and some ampullary cancers also arise from the biliary tract. The presentation, diagnosis, and management of intrahepatic, perihilar, and distal cholangiocarcinomas and of gallbladder cancer are separately described in this chapter. Periampullary tumors can arise from biliary as well as pancreatic, duodenal, or ampullary tissues. The presentation, evaluation, and management of periampullary tumors of biliary tract origin are identical to those of any of the other types of periampullary tumors, namely pancreatic, duodenal, or ampullary tumors. In most instances, the distinction between the tissue type of origin is obscure or may only be made on a histopathologic examination. They are often diagnosed at an advanced stage and are associated with a poor prognosis. Management of these patients requires a multidisciplinary approach by a team with experience in their management and which includes hepatobiliary surgeons, hepatologists, gastroenterologists, diagnostic and interventional radiologists, pathologists, medical oncologists, and radiation oncologists. If the relevant and necessary expertise is not available locally, an early referral to experienced centers should be considered. Development of bile ducts requires complex intercellular interactions and signaling. Notch signaling is a critical determinant of both biliary differentiation and morphogenesis leading to the formation of normal bile ducts. Activation of Notch in liver progenitor cells results in differentiation to biliary ductal cells, whereas activation of Notch signaling in the hepatic lobule promotes ectopic biliary differentiation and duct formation. Experimentally enforced Notch signaling in adult murine hepatocytes causes them to reprogram to a biliary phenotype and can result in cholangiocarcinoma formation. Within the liver, bile ducts along with branches of the hepatic artery and portal vein constitute the portal triad, which is directed to each lobule of the liver. The adult liver is divided into eight segments delineated by blood supply and venous drainage. The caudate lobe drains directly into the left main hepatic duct via numerous small branches. The porta hepatis consists of the bile duct, the portal vein, and the hepatic artery, from right to left. At the hilum, the portal vein is posterior; the right hepatic artery generally passes between the common bile duct and the portal vein; and the cystic artery passes anterior to the bile duct. Arterial anomalies are common, and if not recognized, could lead to inadvertent injury during dissection within the porta hepatis. The cystic duct may enter the common duct near the confluence of the right and left ducts, or distally near the duodenum. The distal bile duct travels posterior within the head of the pancreas and then joins the pancreatic duct in a common channel leading to the ampulla of Vater. The lymph node drainage of the bile ducts involves the superior pancreaticoduodenal, retroportal, or proper hepatic nodes first, then the peripancreatic, celiac, and interaortocaval lymph nodes. The location of the primary tumor within the gallbladder and the proximity of the portal vein, hepatic artery, and bile duct are all important factors in the surgical management of this tumor. The gallbladder has a thin mucosal wall, a narrow lamina propria, and only a single muscle layer. Once this is penetrated, the tumor can access major lymphatic and vascular channels leading to early lymphatic and hematogenous spread. Tumors of the infundibulum or cystic duct can also obstruct the common bile duct and may involve the portal vein.
The apparent volume into which a drug distributes in the body at equilibrium in called the volume of distribution (Vd) medications 1 gram cheap tranexamic line, and may or may not correspond to an actual physiologic compartment. The rate and extent to which a drug distributes into various tissues depend on a number of factors, including hydrophobicity, tissue permeability, tissue-binding constants, binding to serum proteins, and local organ blood flow. It is, however, more common to refer to the half-life than to the elimination rate constant of a drug. The half-life of a drug is a useful parameter to estimate the time required to reach steady state on a multidose schedule or during a continuous intravenous drug infusion. Dose Proportionality When drug concentrations change in strict proportionality to the dose of drug administered, then the condition of dose proportionality (or linear pharmacokinetics) holds. Dose proportionality is clinically important because it means that dose adjustments will generate predictable changes in systemic drug exposure. Factors that can contribute to a lack of dose proportional pharmacokinetics include saturable oral absorption,15 capacity-limited distribution or protein binding,16 and/or saturable metabolism. An alternative, more robust study design is a crossover study in which each patient receives a low dose, an intermediate dose, and a high dose over consecutive cycles of treatment. In oncology, pharmacodynamic variability may account for substantial differences in clinical outcomes, even when systemic exposures are uniform. Variability in pharmacodynamic response may be heavily influenced by clinical covariates such as age, gender, prior chemotherapy, prior radiotherapy, concomitant medications, or other variables. In general, the specific parameter used as the independent variable in a pharmacodynamic analysis depends on the particular characteristics of the study drug. In oncology, pharmacodynamic studies of drug effects have most often focused on toxicity endpoints. Dose-limiting neutropenia has been frequently analyzed using a sigmoid maximum effect model described by the modified Hill equation. The pharmacodynamic analysis of subjectively graded clinical endpoints, such as common toxicity criteria scores on a 4-point scale, may require more sophisticated statistical methods. Physiologic pharmacodynamic models describing the severity and time course of drug-related myelosuppression have been derived using population mixed-effect methods for several agents, including paclitaxel23,24 and pemetrexed. For such drugs, the dose fractionated over several days can produce a different antitumor response or toxicity profile compared with the same dose given over a shorter period. For example, the efficacy of etoposide in the treatment of small-cell lung cancer is markedly increased when an identical total dose of etoposide is administered by a 5-day divided-dose schedule rather than a 24-hour infusion. This finding has led to the use of prolonged oral administration of etoposide to treat patients with cancer. The principal underlying sources of this interindividual pharmacokinetic/pharmacodynamic variability are discussed in the following paragraphs. Flat-fixed dosing versus body surface area based dosing of anticancer drugs in adults: does it make a difference? Although pediatric cancers remain rare compared with cancers in adults and the elderly population, in particular, optimizing treatment in a patient group with a high cure rate and a long expected survival becomes critical to minimize the incidence of preventable late complications while maintaining efficacy. Pathophysiologic changes associated with particular malignancies may cause dramatic alterations in drug disposition. The best known example of this a priori dose adjustment of an anticancer agent remains carboplatin, which is excreted renally almost entirely by glomerular filtration. Various strategies have been developed to estimate carboplatin doses based on renal function among patients, either using creatinine clearance51 or glomerular filtration rates as measured by a radioisotope method. The survey results indicated that 41% of the applications that included renal impairment study data resulted in a recommendation of dose adjustment in renal impairment. A striking example of a drug in the former category is imatinib, an agent that is predominantly eliminated by hepatic pathways but where predialysis renal impairment is associated with dramatically reduced drug clearance,55 presumably due to a transportermediated process. Because only the unbound (or free) drug in plasma water is available for distribution, the therapeutic response will correlate with free drug concentration rather than total drug concentration. Several clinical situations, including liver and renal disease, can significantly decrease the extent of serum binding and may lead to higher free drug concentrations and a possible risk of unexpected toxicity, although the total (free plus bound forms) plasma drug concentrations are unaltered. For some anticancer agents, including etoposide62 and paclitaxel,63 however, protein binding is highly dependent on dose and schedule. Sex Dependence A number of pharmacokinetic analyses have suggested that male gender is positively correlated with the maximum elimination capacity of various anticancer drugs. These observations have added to a growing body of evidence that the pharmacokinetic profile of various anticancer drugs exhibits significant sexual dimorphism, which is rarely considered in the design of clinical trials during oncology drug development. Drug Interactions Effects of Hepatic Impairment In contrast to the predictable decline in renal clearance of drugs when glomerular filtration is impaired, it is difficult to make general predictions on the effect of impaired liver function on drug clearance. The major problem is that commonly applied criteria to establish hepatic impairment are typically not good indicators of drug-metabolizing enzyme activity and that several alternative hepatic function tests, such as indocyanine green and antipyrine, have relatively limited value in predicting anticancer drug pharmacokinetics. These interactions may influence the effectiveness of each of the components of the combination, and typically occur when the pharmacokinetic profile of one drug is altered by the other. Such interactions are important in the design of trials evaluating drug combinations because, occasionally, the outcome of concurrent drug administration is diminished therapeutic efficacy or increased toxicity of one or more of the administered agents. Although a recent survey indicated that clinically significant pharmacokinetic interactions are relatively rare in Phase I trials of oncology drug combinations,65 interactions appear to be more common for combinations of tyrosine kinase inhibitors with cytotoxic chemotherapeutics. For example, anticonvulsant drugs such as phenytoin, phenobarbital, and carbamazepine can induce drug-metabolizing enzymes and thereby increase the clearance of various anticancer agents. It should be borne in mind that several pharmacokinetic parameters could be altered simultaneously. Especially in the development of anticancer agents given by the oral route, Effects of Serum Proteins the binding of drugs to serum proteins, particularly those that are highly bound, may also have significant clinical implications for a therapeutic outcome. Recommended without food to achieve consistent drug exposure; was taken without food in clinical trials.
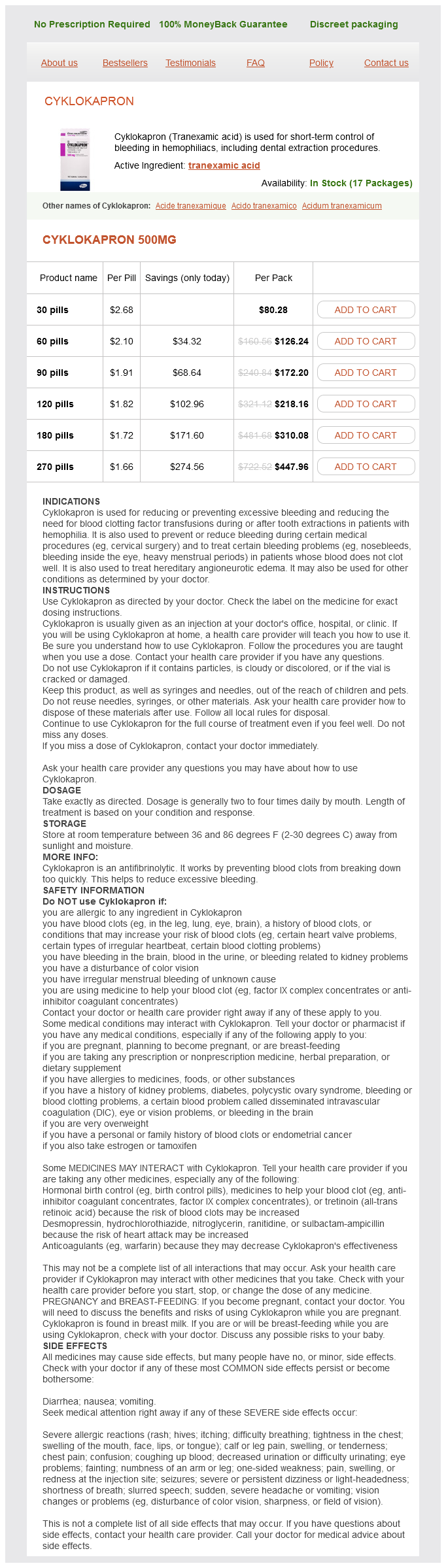
Tranexamic Acid Dosage and Price
Cyklokapron 500mg
- 30 pills - $80.28
- 60 pills - $126.24
- 90 pills - $172.20
- 120 pills - $218.16
- 180 pills - $310.08
- 270 pills - $447.96
The activity of paclitaxel and docetaxel in head and neck cancer has fostered the development and evaluation of taxane and cisplatin combinations medicine in the civil war order tranexamic uk. No significant difference in response rate or survival was found between the arms. The reported quality of life was better on the paclitaxel arm over the first 16 weeks of treatment. There is great interest in the combination of standard chemotherapy with newer targeted agents. The arm including the cetuximab had a significantly higher response rate (10% versus 26%, p = 0. Subsequent maintenance with cetuximab alone was allowed on the investigational arm, but there was no crossover to cetuximab on the standard arm. Quality of life outcomes were reported to not be significantly different between the treatment arms. Whether allowing patients to crossover to cetuximab on the doublet arm at progression would have decreased or eliminated the observed survival difference is of interest for future research. The operation should be undertaken only if it is believed to be highly likely that all gross disease will be removed and margins will be negative. A matched-pair analysis was performed using a series of patients treated with surgery alone; 56 matched pairs of patients were identified. For patients with close (<5 mm) or positive margins, we recommend 70 Gy in 7 weeks or 74. There are reports of a small proportion of patients with recurrent or metastatic disease being controlled long term with chemotherapy alone. An analysis of available data suggests there is no compelling difference in survival rates comparing the two sequences42; localÂregional control may be improved with postoperative treatment. The increased morbidity from combined treatment is not associated with a significantly improved control rate, and many patients with local or regional failure can be salvaged by secondary procedures. These include the therapy of unresectable disease, for organ preservation, and for patients with poor risk pathologic features after surgery. In certain circumstances, response to chemotherapy has been used to triage patients to different localÂregional treatments. In this section, general principles for the integration chemotherapy with localÂregional treatment will be discussed with a focus on the results of randomized trials. However, the significant improvement appeared limited to those patients who received concomitant treatment (absolute difference of 8% at 5 years, p <0. Survival benefit diminished with patient age and, on subset analysis, was not significant in patients over 70 years of age. Many of the included studies had significant methodologic limitations by more contemporary trial standards. As localÂregional control improves, the rate of clinically apparent distant metastases is increasing,153 and induction chemotherapy is, on average, better tolerated than maintenance therapy as a way to give additional systemic therapy. Resectability was assessed pretreatment, not after chemotherapy, and was a stratification criteria. Overall, there was no significant difference between the arms with regard to overall survival or localÂregional control, although the incidence of distant metastases was lower among patients treated with chemotherapy. On a subset analysis, however, patients with unresectable disease benefitted from the incorporation of induction chemotherapy for all outcomes, including localÂregional control, distant control, and overall survival (3-year survival 24% versus 10%, p = 0. Among resectable patients, improvement in distant control was offset by a decrement in localÂregional control with the integration of induction chemotherapy, and reported survival rates in this subgroup were similar on both treatment arms. However, with the incorporation of taxanes into induction regimens containing cisplatin and 5-fluororuacil, newer data suggest that the indications for induction chemotherapy may further evolve. Three randomized trials have compared the relative efficacies of induction chemotherapy with standard cisplatin and 5-fluorouracil versus a triplet including a taxane and these same two drugs with one or both being dose adjusted. In general, the taxanecontaining triplet was associated with a higher response rate to induction chemotherapy, and improved both progression-free and overall survival. More neutropenia was observed with triplet therapy but, overall, it was as well-tolerated as standard cisplatin and 5-fluorouracil. These studies were designed to determine which induction chemotherapy was more efficacious, and provide convincing evidence that the triplet of a taxane with cisplatin and 5-flurouracil is superior to standard cisplatin and 5-fluorouracil alone as induction therapy. However, an alternative design is necessary to define the role of induction with such triplets in standard practice. To date, available randomized trials have failed to demonstrate a clear overall survival benefit with the incorporation of induction chemotherapy. The combination of docetaxel, cisplatin, and 5-fluorouracil has been the focus of these investigations. One study available only in abstract form was confounded by the lack of an intention to treat an analysis with unequal exclusions among treatment arms. Even with those methodologic limitations, it failed to demonstrate a significant improvement in overall survival with the incorporation of induction docetaxel, cisplatin, and 5-fluorouracil or cisplatin, and 5-fluorouracil. Patients could have unresectable disease or be resectable, with the intent of therapy being organ preservation. The study was closed early because of slower than expected accrual, so it was somewhat underpowered. There was no difference in overall or progression-free survival between the arms with a median follow-up of 49 months; the 3-year overall survival rates were 73% on the induction arm and 78% on the concurrent arm (p = 0.