Valsartan
General Information about Valsartan
Valsartan belongs to a group of medications generally known as ARBs, which work by blocking the motion of angiotensin II, a hormone that causes blood vessels to slim and blood pressure to extend. By blocking the results of this hormone, valsartan helps to dilate or widen the blood vessels, permitting for improved blood flow and decreased blood strain.
Valsartan is contraindicated in pregnant ladies, as it might harm the growing fetus. It is also not really helpful for people who have a historical past of angioedema, a situation characterized by swelling of the face, lips, tongue, or throat.
Valsartan can also work together with other drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs), sure antibiotics, and potassium supplements. It is essential to tell a healthcare skilled about all drugs, dietary supplements, and herbs being taken earlier than starting valsartan to avoid any potential interactions.
Valsartan, also known by its model name Diovan, is a commonly prescribed treatment used to deal with hypertension, also called hypertension. It is assessed as an angiotensin receptor blocker (ARB) and works by stress-free the blood vessels, permitting for higher blood flow and lowering blood pressure.
In abstract, valsartan is a broadly prescribed ARB that has been proven to be an efficient and safe treatment for high blood pressure. It works by enjoyable blood vessels, enhancing blood flow, and reducing blood pressure. As with any medication, it is important to comply with the prescribed dosage and inform a healthcare skilled of any current medical circumstances or medicines being taken. With correct use and monitoring, valsartan can successfully assist handle and management hypertension, main to better general well being and a lowered risk of problems.
High blood pressure is a serious health situation that affects millions of individuals worldwide. It can result in varied issues corresponding to coronary heart disease, stroke, and kidney failure. It is often called the 'silent killer' because it usually does not cause any symptoms until it has brought on vital injury to the physique.
Like any medicine, valsartan may cause side effects, though not everyone will experience them. Common side effects may include dizziness, complications, and nausea. In some instances, extra extreme unwanted effects may happen, including allergic reactions, liver issues, and low blood stress. It is crucial to hunt medical consideration if any of those symptoms happen.
Besides treating hypertension, valsartan can additionally be used to stop heart failure and to improve survival charges after a heart attack. It has additionally been discovered to be effective in stopping kidney damage in individuals with type 2 diabetes.
The typical dosage of valsartan is between 80-160 milligrams per day, taken orally. It is often taken as soon as a day, with or without food. It is necessary to take this treatment as prescribed by a healthcare skilled, and not to adjust the dosage or cease taking it with out consulting a physician. It could take a couple of weeks for valsartan to succeed in its full effectiveness, so it is important to proceed taking it even when there is no quick change in blood stress.
Both bromocriptine and cabergoline can be given vaginally if the patient does not tolerate the oral form prehypertension 30 years old purchase genuine valsartan online. Patients with hyperprolactinemia, with or without microadenoma, with adequate estrogen levels (> 40 pg/ mL) and who do not desire pregnancy should be treated with periodic progestin withdrawal. Patients who fail medical therapy may require surgery, which involves transsphenoidal microsurgical exploration of the sellaturcica with removal of the pituitary adenoma while preserving the functional capacity of the remaining gland. Complications of the surgery include transient diabetes insipidus (occurs in about one-third), hemorrhage, meningitis, cerebrospinal fluid leak, and panhypopituitarism. Cure rate is directly related to the pretreatment prolactin levels (prolactin level of 100 ng/ mL has an excellent prognosis, whereas 200 ng/ mL has a poor prognosis). It may be preferable to reduce the size of the macroadenoma with bromocriptine before surgical removal of these tumors. With uterine adhesions, the hormonal axis (hypothalamus, pituitary, ovary) is normal. Which of the following clinical presentations is consistent with a prolactinsecreting pituitary adenoma Medications are a common cause of hyperprolactinemia, especially psychotropic medications. The anterior, not posterior, pituitary secretes prolactin; an anterior pituitary adenoma is more likely to be a cause of hyperprolactinemia. Symptoms may include galactorrhea, headache, and peripheral vision defect (bitemporalhemianopsia). Pituitary adenomas impinge on the optic chiasm, causing deficits of the peripheral vision (bitemporalhemianopsia) and not the central visual field. The pituitary is located in the anterior half of the cerebrum; therefore, an occipital cerebral defect is unlikely to be a clinical presentation relating to a pituitary adenoma. Whereas prolactin acts on the breast to produce milk, oxytocin acts on the breast to stimulate ejection of the milk in a lactating woman. Bromocriptine therapy is indicated during pregnancy if symptoms (eg, headache or visual field abnormalities) arise. It is typically reserved for patients with a macroadenoma, who have failed medical treatment. Surgery would not be indicated for this patient who has a microadenoma and has not attempted medical therapy. Plus, any procedure that may induce hemorrhage in a patient would be considered risky in pregnancy. Tamoxifen is not indicated because it is a selective estrogen receptor modulator used in the treatment of breast cancer. It therefore binds to estrogen receptors to inhibit estrogen action, and does not affect the microadenoma or prolactin production and action. Expectant management would not be a good s option because a microadenoma can continue to grow during pregnancy from hormonal influences. The first evaluation in a woman with oligomenorrhea and galactorrhea should be a pregnancy test. Her delivery was complicated by postpartum hemorrhage requiring curettage of the uterus and a blood transfusion of four units of erythrocytes. Mechanism: Pregnancy-associated enlargement of the anterior pituitary gland and hypotension leading to hemorrhage into the anterior pituitary gland. Other complications that are likely with this condition: Anterior pituitary insufficiency, such as hypothyroidism or adrenocortical insufficiency. Know the other tropic hormones that may be affected by anterior pituitary necrosis. Considerations this patient developed amenorrhea from the time of her vaginal delivery that was complicated by postpartum hemorrhage. The patient also underwent a uterine curettage in the treatment of the postpartum bleeding. In this setting, there are two explanations: (1) Sheehan syndrome and (2) intrauterine adhesions (Asherman syndrome). Sheehan syndrome is caused by hypotension in the postpartum period, leading to hemorrhagic necrosis of the anterior pituitary gland. Asherman syndrome is caused by the uterine curettage, which damages the decidua basalis layer, rendering the endometrium unresponsive. The key to differentiating between Sheehan syndrome and intrauterine adhesions is to assess for whether or not the anterior pituitary is functioning, and whether the outflow tract (uterus) is responsive to hormonal therapy. H ad the patient been able to breastfeed, the most likely diagnosis would have been intrauterine synechiae. This patient was given a combination oral contraceptive agent, and if the endometrium were responsive to the hormonal therapy, then proliferation of the endometrium should occur followed by stabilization of the endometrium with the progestin component, and then finally bleeding when the placebo pills are taken (days 21 28). From a more pathophysiologic standpoint, it is the amount of bleeding that results in, or threatens to result in, hemodynamic instability if left unabated. H owever, in a nonlactating woman, when no menses resumes by 12 weeks after delivery, then pathology must be suspected. Overall, the most common cause of amenorrhea in the reproductive years is pregnancy. If the patient does not have a history of postpartum hemorrhage, evaluation of hypothalamic causes, such as hypothyroidism or hyperprolactinemia, is often fruitful. Polycystic ovarian syndrome is characterized by estrogen excess without progesterone, obesity, hirsutism, and glucose intolerance. Polycystic ovarian syndrome should be suspected in patients with obesity, hirsutism, and oligomenorrhea.
The coagulopathy is secondary to hypofibrinogenemia blood pressure medication young age buy generic valsartan 80 mg line, and clinically evident bleeding is usually not encountered unless the fibrinogen level is below 100 to 150 mg/ dL. Although painful vaginal bleeding is the hallmark, preterm labor, stillbirth, and/ or fetal heart rate abnormalities may also be seen. A concealed abruption can occur when blood is trapped behind the placenta, so that external hemorrhage is not seen. Serial hemoglobin levels, following the fundal height and assessment of the fetal heart rate pattern, are often helpful. As compared to placenta previa, fetal-to-maternal hemorrhage is more common with placental abruption, and some practitioners recommend testing for fetal erythrocytes from the maternal blood. One such test of acid elution methodology is called the Kleihauer Betke test, which takes advantage of the different solubilities of maternal versus fetal hemoglobin. The management of placental abruption is dependent on the fetal gestational age, fetal status, and the hemodynamic status of the mother. H owever, in a woman with a premature fetus (< 34 weeks) and a diagnosis of "chronic abruption," expectant management may be exercised if the patient is stable with no active bleeding or signs of fetal compromise. Although there is no contraindication to vaginal delivery, cesarean section is often the chosen route of delivery for fetal indications. In cases of abruptions that are associated with fetal death and coagulopathy, the vaginal route is most often the safest for the mother. In the latter scenario, blood products and intravenous fluids are given to maintain the hematocrit above 25% to 30% and a urine output of at least 30 mL/ h. Many of these women will manifest hypertension or preeclampsia following volume replacement, and it may be necessary to start magnesium sulfate for eclampsia prophylaxis. Future Pregnancies There is a high recurrence risk of abruption, ranging from 5% to 10%. If a patient experiences abruptio placentae with two consecutive abruptions, the recurrence rate is as high as 25%. Smoking is the biggest modifiable risk factor (40-fold increased risk in smokers). Women with prior abruption is an indication for early delivery for future pregnancies. Among these causes, placental abruption is slightly more common than placenta previa, with vasa previa being more rare. The patient asks the physician about the accuracy of ultrasound in the diagnosis of abruption. Fetal ultrasound is more accurate in diagnosing placental abruption than placenta previa. Ultrasound is sensitive in diagnosing abruption that occurs in the lower aspect of the uterus. Placenta previa rarely results in consumptive coagulopathy, since there is usually a significantly less amount of bleeding involved in comparison with abruption. Gestational diabetes is more commonly associated with fetal macrosomia, and places the fetus at risk for shoulder dystocia at the time of delivery. A multifetal gestation puts a patient at a higher risk for a placenta previa due to the larger surface area required for the placenta(s), but as mentioned before, coagulopathy is not common in previa. Sonography is accurate in identifying previa, but not sensitive in diagnosing placental abruption. An ultrasound examination is a poor method for assessment of abruption because the freshly developed blood clot behind the placenta has the same sonographic texture as the placenta itself. A high index of suspicion for abruption must be exercised when evaluating the clinical picture as a whole. An extra challenging situation exists in the setting of a concealed abruption, in which the bleeding occurs behind the placenta and no external bleeding is noted. This is extremely dangerous since a greater amount of time will most likely pass before the abruption is diagnosed. Trauma is the most significant risk factor for abruption in comparison to the other answer choices. Marijuana, as opposed to cocaine, is not associated with abruption since it does not cause maternal hypertension and vasoconstriction like cocaine. A prior cesarean delivery may predispose a patient to placenta previa with an associated accreta in future pregnancies, but neither a prior cesarean delivery nor an accreta is a significant risk factor for abruption. The most significant fetal risk associated with breech presentation is cord prolapse, which can lead to significant oxygen deprivation to the fetus. Cocaine use is strongly associated with the development of placental abruption due to its effect on the vasculature (vasospasm). Whereas, the management of placental abruption with a live fetus many times includes cesarean, with a fetal demise, the management focuses on vaginal delivery. The diagnosis of abruptio placentae is a clinical one since it can present in many different ways. The major risk factors for abruptio placentae are hypertension, trauma, and cocaine use, with hypertension being most common. The most common cause of antepartum bleeding with coagulopathy is abruptio placentae. The risk of recurrence with abruption is significant, and may necessitate early delivery with subsequent pregnancies. She has a history of previous myomectomy and one prior low-transverse cesarean delivery. She was counseled about the risks, benefits, and alternatives of vaginal birth after cesarean, and elected a trial of labor. The placenta does not deliver after 30 minutes, and a manual extraction of the placenta is undertaken.
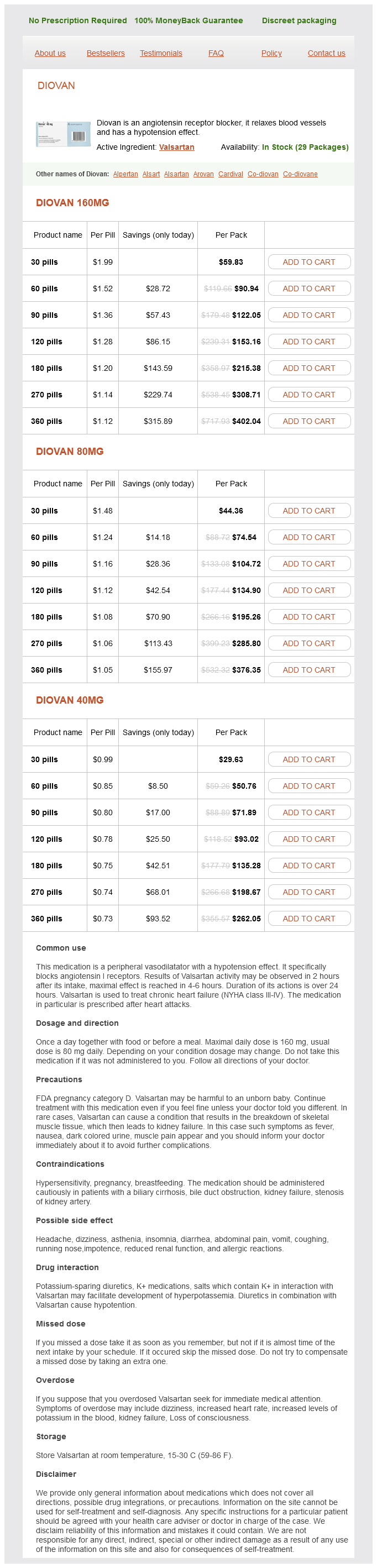
Valsartan Dosage and Price
Diovan 160mg
- 30 pills - $59.83
- 60 pills - $90.94
- 90 pills - $122.05
- 120 pills - $153.16
- 180 pills - $215.38
- 270 pills - $308.71
- 360 pills - $402.04
Diovan 80mg
- 30 pills - $44.36
- 60 pills - $74.54
- 90 pills - $104.72
- 120 pills - $134.90
- 180 pills - $195.26
- 270 pills - $285.80
- 360 pills - $376.35
Diovan 40mg
- 30 pills - $29.63
- 60 pills - $50.76
- 90 pills - $71.89
- 120 pills - $93.02
- 180 pills - $135.28
- 270 pills - $198.67
- 360 pills - $262.05
Pseudothrombi IgM Immunofluorescence (Left) IgM highlights prominent paraprotein deposition along capillary walls ("wire loop" deposits) and in the capillary lumina (hyaline "thrombi") arrhythmia consultants of connecticut discount valsartan 160 mg on-line, which correlates with the light microscopic findings. Scattered interstitial inflammatory cells with plasma cells are present, which can represent renal involvement by plasma cell dyscrasia. Giant Cell Cast Reaction Myeloma Casts (Left) Strong fuchsinophilic staining highlights light chain casts in several tubules on Masson trichome stain. The red, intense staining may be diminished when the casts are admixed with cellular debris and variable amounts of Tamm-Horsfall protein. Many tubules in the cortex are dilated and show flattening or vacuolization of the epithelium, which are features of acute tubular injury. These casts can be mistaken for intratubular cellular debris, which can be observed in the setting of acute tubular injury/necrosis. Atypical Myeloma Casts Myeloma Casts (Left) Hypereosinophilic casts in the distal nephron segments are admixed with a few inflammatory cells. Prominent neutrophilic reaction surrounding casts can occasionally be present (not shown). Myeloma Casts Kappa Light Chain (Left) Atypical casts are strongly positive for kappa light chain. There is also confluent glomerular and tubular basement membrane staining (in this case dim) for kappa light chain but not for lambda light chain. This may be the earliest evidence of light chain deposition disease, which often occurs concurrently with myeloma cast nephropathy. Scattered inflammatory cells are noted in the interstitium along with a few eosinophils in the tubular lumen. Kappa Light Chain Lambda Light Chain (Left) Immunohistochemistry on the paraffin section for kappa light chain shows strong staining in this tubular cast and a blush of interstitial staining. Lambda light chain immunohistochemistry reveals no significant staining of this intratubular cast. This finding, in conjunction with strong kappa light chain staining (not shown), supports the diagnosis of myeloma cast nephropathy. Atypical Myeloma Casts Myeloma Cast (Left) these casts are atypical, but they do not have the hypereosinophilic appearance of usual light chain casts on H&E. No amyloid was present in other areas of the kidney biopsy, and the patient did not have systemic amyloidosis. Atypical Myeloma Cast With Amyloid Myeloma Cast (Left) the light chain casts in the tubules stain strongly blue with a granular and coarse appearance in the toluidine blue section submitted for electron microscopy. Some casts have substructural organization with a lattice framework (not shown), but the absence of this finding is not unusual. Atypical Myeloma Cast Ultrastructure of Cast (Left) At higher magnification, this tubular cast is composed of numerous randomly arranged fibrils, which can be observed in myeloma cast nephropathy whether or not the casts have amyloid. Casts, Tubulopathy, and Histiocytosis Cryocrystalglobulinemia (Left) An unusual case with 3 diagnoses related to a lambda paraprotein shows light chain cast nephropathy, light chain proximal tubulopathy, and crystal-storing histiocytosis. By immunofluorescence, these structures stained for kappa but not lambda light chain. Escape into the cytoplasm may be due to lysosomal rupture, which would be expected to injure the cell. Intracytoplasmic Crystals Intracytoplasmic Crystals (Left) Intracytoplasmic crystals are seen on a silver stain. Lack of high-magnification electron micrographs of tubules may result in the diagnosis of light chain proximal tubulopathy being overlooked. Note the absence of finely granular deposits along the basement membrane, which if present would indicate concurrent light chain deposition disease. The difference in localization of the monoclonal protein is probably related to its physiochemical properties. In this field, the tubular epithelium shows reactive nuclei and cytoplasmic thinning. Mottled Lysosomes Positive Lambda in Tubular Cytoplasm (Left) Light chain proximal tubulopathy without organized inclusions is shown. Basnayake K et al: the biology of immunoglobulin free light chains and kidney injury. Proximal tubules have scattered cytoplasmic inclusions that stain blue on Masson trichrome stain. This patient did not have amyloidosis deposition outside of the proximal tubule cytoplasm. Positive Congo Red Staining Congo Red Staining Under Red Fluorescence (Left) Amyloid proximal tubulopathy is shown. Congo red-positive cytoplasmic inclusions are easily appreciated under red fluorescence. Fibrillary Aggregates in Tubular Cytoplasm Inclusions Positive for Lambda (Left) Amyloid proximal tubulopathy is shown. Cytoplasmic inclusions stain positive for lambda by direct immunofluorescence on fresh tissue. Eosinophilic Inclusions in Silver Stain Kappa Restriction in Proximal Tubules (Left) Light chain proximal tubulopathy with fibrillary aggregates is shown. The fibrillar inclusions stain eosinophilic and silver negative on Jones methenamine silver. Bundles of Large Fibrils Bundles of Large Fibrils (Left) Light chain proximal tubulopathy with fibrillary aggregates is shown.