Valtrex
General Information about Valtrex
Valtrex is also commonly prescribed for the treatment of genital herpes, which is a sexually transmitted infection brought on by the herpes simplex virus (HSV). When taken throughout a herpes outbreak, it can assist reduce the severity of symptoms and speed up the healing process. It may also be used as a suppressive therapy to prevent recurrent outbreaks and reduce the danger of transmission to sexual partners.
In treating shingles, Valtrex helps to reduce the severity and length of the rash, as properly as alleviate the pain and itching associated with it. It is usually recommended for individuals over 50 years old, as they're at a better risk of growing shingles because of weakened immune methods. Despite being vaccinated towards chickenpox in childhood, the virus can reactivate within the body later in life, inflicting shingles.
Valtrex is on the market within the form of an oral pill, and it is typically taken twice a day for one to ten days, depending on the situation being treated. The dosage may differ based mostly on factors such because the severity of the infection, age, and other medical conditions.
Valtrex, also identified by its generic name valacyclovir, is an antiviral drug that's used to treat herpes zoster (shingles), genital herpes, and herpes cold sores on the face and lips. It belongs to a bunch of drugs known as nucleoside analogues, which work by interfering with the expansion and unfold of the herpes virus.
In addition to shingles and genital herpes, Valtrex can be efficient in treating recurrent herpes labialis (cold sores) on the face and lips. Cold sores are brought on by the herpes simplex virus kind 1 (HSV-1), and they typically seem as small, fluid-filled blisters on or around the lips. Valtrex may help to scale back the ache and discomfort associated with cold sores and velocity up the therapeutic course of.
Herpes is a standard virus that impacts tens of millions of individuals worldwide. It is a contagious an infection that may trigger painful blisters and sores in varied elements of the body. While there is not a remedy for herpes, there are medicines that may assist manage the symptoms and forestall outbreaks. One of these medicines is Valtrex.
Valtrex is usually well-tolerated, with frequent side effects including nausea, headache, and dizziness. In uncommon circumstances, it might trigger extra serious side effects similar to confusion, decreased urine manufacturing, and allergic reactions. It is necessary to tell a doctor if any of these unwanted effects are experienced.
In conclusion, Valtrex is a extensively used antiviral drug that is effective in treating shingles, genital herpes, and chilly sores. It helps to scale back symptoms and velocity up the therapeutic process, offering relief to those affected by these situations. If you've been identified with any of those infections, seek the advice of your physician to see if Valtrex is an acceptable treatment option for you.
It is value noting that Valtrex isn't a cure for herpes, and it doesn't stop the transmission of the virus to others. Therefore, it is essential to practice safe intercourse and avoid intimate contact during outbreaks to stop passing the infection to a partner.
For all stone types antiviral lubricant herpes discount valtrex 1000 mg with mastercard, consistently diluted urine reduces the likelihood of crystal formation. Because of differences in insensible fluid losses and fluid intake from food sources, the required total fluid intake will vary from person to person. Rather than specify how much to drink, it is more helpful to educate patients about how much more they need to drink in light of their 24-h urine volume. Individuals with higher urine calcium excretion tend to absorb a higher percentage of ingested calcium. Nevertheless, dietary calcium restriction is not beneficial and, in fact, is likely to be harmful (see "Dietary Risk Factors," above). In a randomized trial in men with high urine calcium and recurrent calcium oxalate stones, a diet containing 1200 mg of calcium and a low intake of sodium and animal protein significantly reduced subsequent stone formation from that with a low-calcium diet (400 mg/d). A thiazide diuretic, in doses higher than those used to treat hypertension, can substantially lower urine calcium excretion. Several randomized controlled trials have demonstrated that thiazide diuretics can reduce calcium oxalate stone recurrence by ~50%. When a thiazide is prescribed, dietary sodium restriction is essential to obtain the desired reduction in urinary calcium excretion. While bisphosphonates may reduce urine calcium excretion in some individuals, there are no data on whether this class of medication can reduce stone formation; therefore, bisphosphonates cannot be recommended solely for stone prevention at present. A reduction in urine oxalate will in turn reduce the supersaturation of calcium oxalate. In patients with the common form of nephrolithiasis, avoiding high-dose vitamin C supplements is the only known strategy that reduces endogenous oxalate production. Oxalate is a metabolic end product; therefore, any dietary oxalate that is absorbed will be excreted in the urine. First, the avoidance of foods that contain high amounts of oxalate, such as spinach, rhubarb, and potatoes, is prudent. However, extreme oxalate restriction has not been demonstrated to reduce stone recurrence and could be harmful to overall health, given other health benefits of many foods that are erroneously considered to be high in oxalate. Controversy exists regarding the most clinically relevant measure of the oxalate content of foods. Notably, the absorption of oxalate is reduced by higher calcium intake; therefore, individuals with higher-than-desired urinary oxalate should be counseled to consume adequate calcium. Oxalate absorption can be influenced by the intestinal microbiota, depending on the presence of oxalate-degrading bacteria. Currently, however, there are no available therapies to alter the microbiota that beneficially affect urinary oxalate excretion over the long term. For patients with lower urine citrate in whom dietary modification does not adequately increase urine citrate, the addition of supplemental alkali (typically potassium citrate) will lead to an increase in urinary citrate excretion. Sodium salts, such as sodium bicarbonate, while successful in raising urine citrate, are typically avoided due to the adverse effects of sodium on urine calcium excretion. Past reports suggested that higher levels of urine uric acid may increase the risk of calcium oxalate stones, but more recent studies do not support this association. However, allopurinol reduced stone recurrence in one randomized controlled trial in patients with calcium oxalate stones and high urine uric acid levels. The lack of association between urine uric acid level and calcium oxalate stones suggests that a different mechanism underlies the observed beneficial effect of allopurinol. Calcium Phosphate Calcium phosphate stones share risk factors with calcium oxalate stones, including higher concentrations of urine calcium and lower concentrations of urine citrate, but additional factors deserve attention. Calcium phosphate stones are more common in patients with distal renal tubular acidosis and primary hyperparathyroidism. There are no randomized trials on which to base preventive recommendations for calcium phosphate stone formers, so the interventions are focused on modification of the recognized risk factors. Thiazide diuretics (with sodium restriction) may be used to reduce urine calcium, as described above for calcium oxalate stones. However, the urine pH of these patients should be monitored carefully because supplemental alkali can raise urine pH, thereby potentially increasing the risk of stone formation. Reduction of dietary phosphate may be beneficial by reducing urine phosphate excretion. Urine pH is the predominant influence on uric acid solubility; therefore, the mainstay of prevention of uric acid stone formation entails increasing urine pH. While acidifying the urine is not easily done, alkalinizing the urine can be readily achieved by increasing the intake of foods rich in alkali. If necessary, supplementation with bicarbonate or citrate salts (preferably potassium citrate) can be used to reach the recommended pH goal of 6 to 7 throughout the day and night. Uric acid is the end product of purine metabolism; thus reduced consumption of purine-containing foods can lower urine uric acid excretion. For example, an individual with high uric acid generation and concurrent high fractional excretion of uric acid will have high urine uric acid excretion with a normal (or even low) serum uric acid level. If alkalinization of the urine alone is not successful and if dietary modifications do not reduce urine uric acid sufficiently, then the use of a xanthine oxidase inhibitor, such as allopurinol or febuxostat, can reduce urine uric acid excretion by 4050%. Long-term dietary cystine restriction is not feasible and is unlikely to be successful; thus the focus for cystine stone prevention is on increasing cystine solubility. This goal may be achieved by treatment with medication that covalently binds to cystine (tiopronin and penicillamine) and a medication that raises urine pH. The preferred alkalinizing agent is potassium citrate as sodium salts may increase cystine excretion. As with all stone types, and especially in patients with cystinuria, maintaining a high urine volume is an essential component of the preventive regimen.
Patients presenting with scleroderma renal crisis should be immediately hospitalized hiv infection rate nepal buy discount valtrex 1000 mg on-line. Anecdotal evidence indicates responses to endothelin-1 receptor blockers and prostacyclins. Substantial renal recovery can occur following scleroderma renal crisis, and dialysis can be discontinued, in 3050% of the patients. Kidney transplantation is appropriate for those unable to discontinue dialysis after 2 years. The inflammatory symptoms of early skin involvement can be controlled with antihistamines and cautious short-term use of low-dose glucocorticoids (<5 mg/d of prednisone). Because the skin is dry, the use of hydrophilic ointments and bath oils is encouraged. Ischemic digital ulcers should be protected by occlusive dressing to promote healing and prevent infection. No therapy has been shown to be effective in preventing the formation of calcific soft tissue deposits or promoting their dissolution. Short courses of nonsteroidal anti-inflammatory agents, weekly methotrexate, and cautious use of low-dose corticosteroids may alleviate these symptoms. Physical and occupational therapy can be effective for maintaining musculoskeletal function and improving long-term outcomes. Skin regression characteristically occurs in an order that is the reverse of initial involvement, with softening on the trunks followed by proximal and finally distal extremities; however, sclerodactyly and finger contractures generally persist. Approximately one-third of patients present with systemic manifestations; a small but significant number of patients develop malignant lymphoma. The major infiltrating cells in the affected exocrine glands are activated T and B lymphocytes. Othersymptomsincludeburning,accumulationofsecretions in thick strands at the inner canthi, decreased tearing, redness, itching, eye fatigue, and increased photosensitivity. Antimitochondrial antibodies may connote liver involvement in the form of primary biliary cirrhosis (Chap. Autoantibodies to 21-hydroxylate have recently been described in almost 20% of patients; their presence is associated with a blunted adrenalresponse. Most lymphomas are extranodal, low-grade marginal-zone B cell lymphomas and are usually detected incidentally during evaluation of thelabialbiopsy. To replace deficient tears, several ophthalmic preparations are readily available (hydroxypropyl methylcellulose; polyvinyl alcohol; 0. If corneal ulcerations are present, eye patching and boric acid ointments are recommended. Certain drugs that may decrease lacrimal and salivary secretions, such as diuretics, antihypertensive drugs, anticholinergics, and antidepressants, should be avoided. To stimulate secretions, orally administered pilocarpine (5 mg thrice daily) or cevimeline (30 mg thrice daily) appears to improve sicca manifestations, and both are well tolerated. Patients with renal tubular acidosis should receive sodium bicarbonate by mouth (0. Knowledgeofits pathology comes from both biopsy and autopsy studies that cover a range of disease durations. Synovitis and myxoid marrow represent the earliest changes, followed by pannus and subchondral granulation tissue. Inflammatory arthritis of the apophyseal (facet) joints is common, with synovitis, inflammation at the bony attachment of the joint capsule, and subchondral bonemarrowgranulationtissue. Lining layer hyperplasia, lymphoid infiltration, and pannus formationarealsofound. Enthesitis is associated with prominent edema of the adjacent bone marrow and is often characterized by erosive lesions that eventually undergoossification. Subclinical intestinal inflammation has been found in the colon or distal ileum in a majority of patients with SpA. Indirectevidenceanddatafrom animal models also implicate bone morphogenic proteins, hedgehog proteins, and prostaglandin E2. Neck pain and stiffness from involvement of the cervical spine are usually relatively late manifestations but are occasionally dominant symptoms. Peripheral arthritis and enthesitis usually predominate, with axial symptoms superveninginlateadolescence. Disease progression can be estimated clinically from loss of height, limitation of chest expansion and spinal flexion, and occiput-to-wall distance. Occasionally, fracture through a diskovertebral junction and adjacent neural arch, termed pseudoarthrosis, most common in the thoracolumbar spine, can be an unrecognized source of persistent localized pain and/or neurologicdysfunction. The most common extraarticular manifestation is acute anterior uveitis, which occurs in up to 40% of patients and can antedate the spondylitis. They are applicable to individuals with 3 months of backpainwithageofonset<45yearsold. The response tends to be stable over time, and partial or full remissions are common. Predictors of the best responses include younger age, shorter disease duration, higher baseline inflammatory markers, and lower baseline functional disability. Nonetheless, some patients with long-standing disease and even spinal ankylosis can obtain significant benefit. Increased bone mineral density is found as early as 24 weeks after onset of therapy. Infliximab is given intravenously, 35 mg/kg body weight, and then repeated 2 weeks later, again 6 weeks later, and then at 8-week intervals.
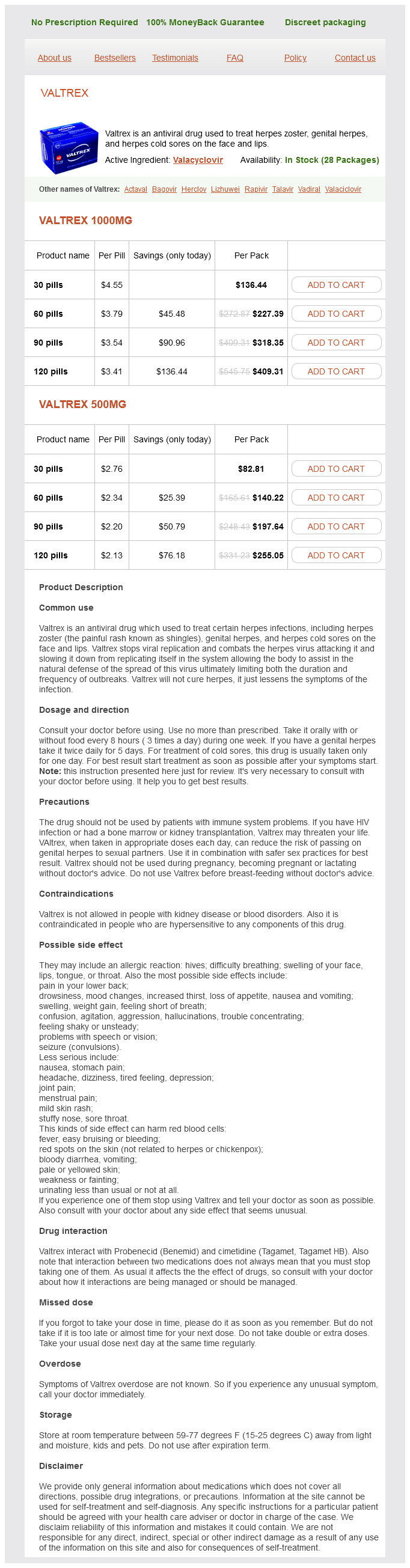
Valtrex Dosage and Price
Valtrex 1000mg
- 30 pills - $136.44
- 60 pills - $227.39
- 90 pills - $318.35
- 120 pills - $409.31
Valtrex 500mg
- 30 pills - $82.81
- 60 pills - $140.22
- 90 pills - $197.64
- 120 pills - $255.05
An abdominal ultrasound is recommended in the emergency ward as the initial diagnostic imaging modality and is most useful to evaluate for gallstone disease and the pancreatic head anti viral anti fungal herbs order discount valtrex on line. Radiologic studies useful in the diagnosis of acute pancreatitis are discussed in Chap. Hypocalcemia occurs in ~25% of patients, and its pathogenesis is incompletely understood. Intraperitoneal saponification of calcium by fatty acids in areas of fat necrosis occurs occasionally, with large amounts (up to 6. The diagnosis is established by two of the following three criteria: (1) typical abdominal pain in the epigastrium that may radiate to the back, (2) threefold or greater elevation in serum lipase and/or amylase, and (3) confirmatory findings of acute pancreatitis on cross-sectional abdominal imaging. Patients also have associated nausea, emesis, fever, tachycardia, and abnormal findings on abdominal examination. The differential diagnosis should include the following disorders: (1) perforated viscus, especially peptic ulcer; (2) acute cholecystitis and biliary colic; (3) acute intestinal obstruction; (4) mesenteric vascular occlusion; (5) renal colic; (6) inferior myocardial infarction; (7) dissecting aortic aneurysm; (8) connective tissue disorders with vasculitis; (9) pneumonia; and (10) diabetic ketoacidosis. It may be difficult to differentiate acute cholecystitis from acute pancreatitis, because an elevated serum amylase may be found in both disorders. Pain of biliary tract origin is more right sided or epigastric than periumbilical or left upper quadrant and can be more severe; ileus is usually absent. Ultrasound is helpful in establishing the diagnosis of cholelithiasis and cholecystitis. Vasculitides secondary to systemic lupus erythematosus and polyarteritis nodosa may be confused with pancreatitis, especially because pancreatitis may develop as a complication of these diseases. Note the abnormal enhancement of the pancreatic parenchyma (arrow) suggestive of interstitial pancreatitis. In the early phase of acute pancreatitis, which lasts 12 weeks, severity is defined by clinical parameters rather than morphologic findings. Three organ systems should be assessed to define organ failure: respiratory, cardiovascular, and renal. Organ failure is defined as a score of 2 or more for one of these three organ systems using the modified Marshall scoring system. Organ failure that affects more than one organ is considered multisystem organ failure. The late phase is characterized by a protracted course of illness and may require imaging to evaluate for local complications. The important clinical parameter of severity, as in the early phase, is persistent organ failure. These patients may require supportive measures such as renal dialysis, ventilator support, or need for supplemental nutrition via the nasojejunal or parenteral route. Necrosis generally prolongs hospitalization and, if infected, may require operative, endoscopic, or percutaneous intervention. Severity of Acute Pancreatitis Three severity classifications have also been defined: mild, moderately severe, and severe. In mild acute pancreatitis, the disease is self-limited and subsides spontaneously, usually within 37 days after treatment is instituted. Oral intake can be resumed if the patient is hungry, has normal bowel function, and is without nausea and vomiting. Typically, a clear or full liquid diet has been recommended for the initial meal; however, a low-fat solid diet is a reasonable choice following recovery from mild acute pancreatitis. Moderately severe acute pancreatitis is characterized by transient organ failure (resolves in <48 h) or local or systemic complications in the absence of persistent organ failure. These patients may or may not have necrosis, but may develop a local complication such as a fluid collection that requires a prolonged hospitalization greater than 1 week. If a local complication is encountered, management is dictated by clinical symptoms, evidence of infection, maturity of fluid collection, and clinical stability of the patient. Imaging in Acute Pancreatitis Two types of pancreatitis are recognized on imaging as interstitial or necrotizing based on pancreatic perfusion. Interstitial pancreatitis occurs in 9095% of admissions for acute pancreatitis and is characterized by diffuse gland enlargement, homogenous contrast enhancement, and mild inflammatory changes or peripancreatic stranding. Necrotizing pancreatitis occurs in 510% of acute pancreatitis admissions and does not evolve until several days of hospitalization. It is characterized by lack of pancreatic parenchymal enhancement by intravenous contrast agent and/ or presence of findings of peripancreatic necrosis. According to the revised Atlanta criteria, the natural history of pancreatic and peripancreatic necrosis is variable because it may remain solid or liquefy, remain sterile or become infected, and persist or disappear over time. With single-organ system failure, the mortality is 310% but increases to 47% with multisystem organ failure. It is important to note that 8590% of cases of acute pancreatitis are self-limited and subside spontaneously, usually within 37 days after initiation of treatment, and do not exhibit organ failure or local complications. Arrow shows partially enhancing body/tail of pancreas surrounded by fluid with decreased enhancement in the neck/body of the pancreas. Note the demonstration of the main pancreatic duct (big arrow), even though this duct is minimally dilated by endoscopic retrograde cholangiopancreatography. Pancreaticopleural fistula: pancreatic duct leak on endoscopic retrograde cholangiopancreatography. Pancreatic duct leak (arrow) demonstrated at the time of retrograde pancreatogram in a patient with acute exacerbation of alcohol-induced acute or chronic pancreatitis.