Vantin
General Information about Vantin
Vantin is typically taken twice a day, with or without food. The dosage and period of treatment will differ relying on the type and severity of the infection, in addition to a person's age and medical history. It's essential to observe the prescribed remedy plan and complete the full course of antibiotics, even when symptoms enhance. Stopping medicine too early may end up in the micro organism not being totally eradicated, leading to a recurrence of the an infection.
Like any medication, Vantin may trigger unwanted aspect effects in some individuals. Common unwanted aspect effects may include nausea, diarrhea, upset stomach, and headache. If these signs persist or turn out to be extreme, it may be very important contact a well being care provider. Additionally, as with all antibiotic, there is a danger of growing an allergic reaction. Seek immediate medical attention if any signs of an allergic reaction happen, such as rash, itching, swelling of the face or throat, or difficulty breathing.
It is necessary to inform your physician of another drugs you take, together with over-the-counter medications and supplements, as they may work together with Vantin. In particular, you will want to keep away from taking Vantin with antacids or iron supplements, as they can lower the effectiveness of the antibiotic.
In conclusion, Vantin is a highly efficient and commonly prescribed antibiotic for the remedy of delicate to reasonable bacterial infections. It is important to observe the prescribed treatment plan and to take the full course of medicine to be able to guarantee complete eradication of the infection. If you expertise any unwanted effects or have any issues, it is important to seek the guidance of your physician. With correct use, Vantin may help alleviate signs and help in a swift recovery from bacterial infections.
Vantin is an oral antibiotic, obtainable in pill kind or as a suspension. It is usually used to deal with infections of the respiratory tract, together with pneumonia, bronchitis, and sinusitis. It can be used to deal with skin and soft tissue infections, in addition to certain forms of urinary tract infections. Vantin is also effective in treating some sexually transmitted infections, similar to gonorrhea.
Vantin, additionally identified by its generic name cefpodoxime, is a commonly prescribed antibiotic used to treat a wide selection of bacterial infections. It belongs to the category of antibiotics referred to as cephalosporins, and is commonly prescribed for the therapy of delicate to moderate infections. Let's take a more in-depth take a glance at what Vantin is, how it works, and what circumstances it might possibly effectively deal with.
It's important to notice that Vantin isn't efficient against all kinds of bacteria. It particularly targets sure types of micro organism, together with Streptococci, Staphylococci, and some strains of E. coli. Therefore, you will want to only take Vantin for infections that are brought on by these micro organism, as using it for other kinds of infections can contribute to the event of antibiotic resistance.
Vantin works by preventing the growth and replica of micro organism within the body. It does this by interfering with the manufacturing of the bacterial cell wall, which is essential for the bacteria’s survival. Without a cell wall, the micro organism are unable to take care of their form and eventually die off. This helps to cease the spread of an infection and permits the physique's immune system to struggle off the remaining micro organism.
Phototoxic tar dermatitis Coal tar infection transmission 100 mg vantin purchase with visa, creosote, crude coal tar, or pitch, in conjunction with sunlight exposure, may induce a sunburn reaction associated with a severe burning sensation. These volatile hydrocarbons may be airborne, so the patient may give no history of touching tar products. Coal tar or its derivatives may be found in cosmetics, drugs, dyes, insecticides, and disinfectants. Several hours after exposure, a burning erythema occurs, followed by edema and the development of vesicles or bullae. An intense residual hyperpigmentation results that may persist for weeks or months. The intensity of the initial phototoxic reaction may be mild and may not be recalled by the patient despite significant. Fragrance products containing bergapten, a component of oil of bergamot, will produce this reaction. If a fragrance containing this 5-methoxypsoralen or other furocoumarin is applied to the skin before exposure to the sun or tanning lights, berloque dermatitis may result. This hyperpigmentation, which may be preceded by redness and edema, occurs primarily on the neck and face. Artificial bergapten-free bergamot oil and laws limiting the use of furocoumarins in Europe and the United States have made this a rare condition. However, "Florida Water" and "Kananga Water" colognes, formerly popular in the Hispanic, African American, and Caribbean communities, contain this potent photosensitizer and can still be ordered online, as can other aromatherapy products containing furocoumarins. Most phototoxic plants are in the families Umbelliferae, Rutaceae (rue), Compositae, and Moraceae. Incriminated plants include agrimony, angelica, atrillal, bavachi, buttercup, common rice, cowslip, dill, fennel, fig, garden and wild carrot, garden and wild parsnip, gas plant, goose foot, zabon, lime and Persian lime, lime bergamot, masterwort, mustard, parsley, St. In Hawaii, the anise-scented mokihana berry (Pelea anisata) was known to natives for its phototoxic properties (mokihana burn). Exposure through limes used to flavor gin and tonics and Mexican beer may result in phototoxic reactions in outdoor bartenders and their customers. These conditions may be widespread and severe enough to require burn unit management. Occupational disability from exposure to the pink rot fungus (Sclerotinia sclerotiorum), present on celery roots, occurs in celery farmers. In addition, disease-resistant celery contains furocoumarins and may produce phytophotodermatitis in grocery workers. Usually, insufficient sensitizing furocoumarin is absorbed from dietary exposure; however, ingested herbal remedies may cause systemic phototoxicity. Dermatitis bullosa striata pratensis (grass or meadow dermatitis) is a phytophotodermatitis caused by contact not with grass, but with yellow-flowered meadow parsnip or a wild, yellow-flowered herb of the rose family. The eruption consists of streaks and bizarre configurations with vesicles and bullae that heal with residual hyperpigmentation. Similarly, tourists in the tropics may rinse their hair with lime juice outdoors, and streaky hyperpigmentation of the arms and back will result where the lime juice runs down. These disorders are not associated with external photosensitizers (except for some cases of chronic actinic dermatitis) or inborn errors of metabolism. It represents about one quarter of all photosensitive patients in referral centers. The onset is typically in the first four decades of life, and females outnumber males by 2: 1 or 3: 1. The pathogenesis is unknown, but a family history may be elicited in 1050% of patients. Clinically, the eruption may have several different morphologies, although in the individual patient, the morphology is usually constant. The papular (or erythematopapular) variant is the most common, but papulovesicular, eczematous, erythematous, and plaquelike lesions also occur. Plaquelike lesions are more common in elderly patients and may closely simulate lupus erythematosus, with indurated, erythematous, fixed lesions. In African Americans, a pinpoint papular variant has been observed, closely simulating lichen necessarily limited to the sun-exposed areas, and itching is the most prominent symptom. In phytophotodermatitis, the reaction is limited to sun-exposed sites, a burning pain appears within 48 h, and marked hyperpigmentation results. The asymmetry, atypical shapes, and streaking of the lesions are helpful in establishing the diagnosis. Treatment of a severe, acute reaction is similar to the management of a sunburn, with cool compresses, mild analgesics if required, and topical emollients. Use of topical steroids and strict sun avoidance immediately after the injury may protect against the hyperpigmentation. CarlsenK,etal: Phytophotodermatitis in 19 children admitted to hospital and their differential diagnosis. Scarring and atrophy do not occur; in darkly pigmented races, however, marked postinflammatory hyperpigmentation or hypopigmentation may be present. A change in the amount of sun exposure appears to be more critical than the absolute amount of radiation. Typically, however, areas protected during the winter, such as the extensor forearms, are particularly affected, whereas areas exposed all year (face and dorsa of hands) may be relatively spared. The eruption often improves with continued sun exposure (hardening), so patients may be clear of the condition in the summer or autumn.
Peginterferon-alpha-2b and ribavirin for hepatitis C recurrence postorthotopic liver transplantation infection control guidelines buy vantin with mastercard. Intravenous N-acetylcysteine improves transplant-free survival in early stage nonacetaminophen acute liver failure. Simultaneous liver-kidney transplantation summit: current state and future directions. Entecavir and hepatitis B immune globulin in patients undergoing liver transplantation for chronic hepatitis B. Cholestatic hepatitis C following liver transplantation: an outcome-based histological definition, clinical predictors, and prognosis. However, it is important to know the other possible causes of ascites, because the treatment and prognosis may be quite different. In general, the most common causes of ascites are cirrhosis, heart failure, peritoneal carcinomatosis, alcoholic hepatitis, and fulminant liver failure. The differential diagnosis of ascites can be categorized according to its pathophysiology (Table 29-1). Should a diagnostic tap be performed routinely on all patients with ascites at the time of admission to the hospital Ascites is diagnosed when large amounts of fluid are present in the peritoneal cavity. If clinical examination is not definitive in detecting or excluding ascites, ultrasonography may be helpful, and may provide information about the cause of ascites. Ascites in heart failure can mimic ascites in cirrhosis, and the distinction between the two entities can be challenging. However, this does not forego the need for paracentesis, as patients may have ascites in the setting of both heart failure and cirrhosis. The diagnostic paracentesis is an essential and irreplaceable step in the evaluation of new-onset ascites. Delays in diagnostic abdominal paracentesis lead to serious delays in diagnosis and appropriate treatment. Although paracentesis is simple and safe, precautions should be taken to avoid complications. The abdomen should be disinfected with an iodine or similar solution, and the physician should wear sterile gloves during the entire procedure. A site in the left lower quadrant two finger-breadths cephalad from the anterior superior iliac spine and two finger-breadths medial to this landmark appears to be the best site for needle insertion. Because the panniculus is less thick in this area, the needle traverses less tissue. Patients on lactulose tend to have a distended cecum, and therefore the left lower quadrant is chosen over the right lower quadrant. Scars should be avoided, as they are often sites of collateral vessels and adherent bowel. The cell count with differential is the single most important test performed on ascitic fluid, because it provides immediate information about possible bacterial infection. An elevated white blood cell count with a predominance of lymphocytes suggests peritoneal carcinomatosis or tuberculous peritonitis. Ascitic fluid should be cultured by inoculating blood culture bottles at the bedside. The sensitivity of this method is higher than that of sending a tube or syringe of fluid to the laboratory in detecting bacterial growth. Specific culture for tuberculosis should be ordered when tuberculous peritonitis is clinically suspected and the ascitic fluid white cell count is elevated with a lymphocytic predominance. Amylase activity of ascitic fluid is markedly elevated in pancreatic ascites and gut perforation into ascites and may be considered when there is clinical suspicion of such situations. Cytologic examination of ascitic fluid is useful in detecting malignant ascites when the peritoneum is involved with the malignant process. Unfortunately, ascitic fluid cytologic examination is not useful in detecting hepatocellular carcinoma, which seldom metastasizes to the peritoneum. Patients with refractory ascites are currently submitted to repeated large-volume paracentesis in the outpatient clinic. The incidence of ascitic fluid infection or bacterascites is very low in these patients. Therefore it is reasonable to obtain a cell count and differential on all samples of ascitic fluid in the paracentesis clinic setting and culture only samples of ascitic fluid of symptomatic outpatients. Should a diagnostic thoracentesis be performed in patients with cirrhosis and pleural hydrothorax Hepatic hydrothorax is defined as the accumulation of ascitic fluid in the pleural space in a patient with cirrhosis, in whom a cardiac, pulmonary, or pleural cause has been excluded. Approximately 5% to 10% of patients with cirrhosis and ascites develop hepatic hydrothorax, mainly in the right side (almost 70% of the cases), but it can also be in the left side or bilateral. In consequence, a diagnostic thoracentesis in patients with cirrhosis with ascites could be useful to evaluate other causes of pleural effusion in selected situations and to diagnose spontaneous bacterial empyema in patients with cirrhosis with a suspected bacterial infection and negative studies of ascitic fluid, blood, and urine specimens. Chest tube insertion is contraindicated in patients with hepatic hydrothorax, and can lead to rapid clinical deterioration. This gradient is physiologically based on oncotic-hydrostatic balance and is related directly to portal pressure. Mixed ascites is due to multiple concurrent causes, including at least one that causes portal hypertension. Low-gradient ascites is found in the absence of portal hypertension and is usually due to peritoneal disease (see Table 29-2). Ascitic fluid infection can be spontaneous or secondary to an intraabdominal, surgically treatable source of infection. More than 90% of ascitic fluid infections in patients with cirrhosis are spontaneous. This condition can be caused by gut puncture by the needle during attempted paracentesis. When combined with the presence of a polymicrobial ascitic fluid culture, specificity improved to 95.
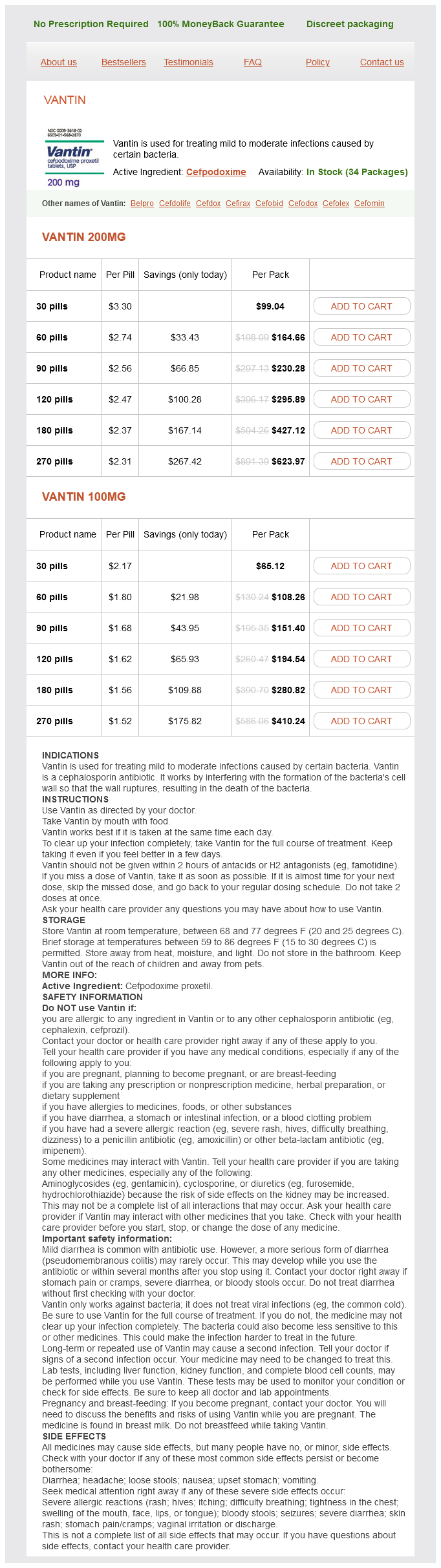
Vantin Dosage and Price
Vantin 200mg
- 30 pills - $99.04
- 60 pills - $164.66
- 90 pills - $230.28
- 120 pills - $295.89
- 180 pills - $427.12
- 270 pills - $623.97
Vantin 100mg
- 30 pills - $65.12
- 60 pills - $108.26
- 90 pills - $151.40
- 120 pills - $194.54
- 180 pills - $280.82
- 270 pills - $410.24
Some patients may require extended therapy antibiotic with metallic taste buy discount vantin, continuous courses, or rotating antibiotic regimens. Prebiotics are nondigestable, fermentable feeds that stimulate the growth and activity of endogenous colonic bacteria, preferentially lactobacillus and bifidobacteria. Saccharomyces boulardi is a probiotic that has stated efficacy for bacterial overgrowth in children; however, it failed to show efficacy in adults. Lactobacillus fermentum failed to show an advantage over placebo in a double-blind crossover study. Rifaximin dose-finding study for the treatment of small intestinal bacterial overgrowth. Methane production and bowel function parameters in healthy subjects on low and high fiber diets. Eradication of small bowel bacterial overgrowth reduces symptoms of irritable bowel syndrome. Small intestinal bacterial overgrowth: roles of antibiotics, prebiotics, and probiotics. Proton pump inhibitor use does not predispose to small intestinal bacterial overgrowth. Effect of octreotide on intestinal motility and bacterial overgrowth in scleroderma. The projected number of new cases in 2013 is 142,820 with 50,830 anticipated deaths occurring, accounting for 9% of estimated new cancer cases and deaths in men and women. Three distinct forms of genomic instability have been recognized and constitute three different molecular pathways to colon carcinogenesis: · Chromosomal instability is the most common pathway to colon cancer, accounting for 80% of cases. Left-sided colonic tumors are more likely to present with obstructive symptoms than right-sided colonic tumors. Right-sided colon cancers are more likely to present at an advanced stage because of the large capacity of the cecum and ascending colon. Nx: Lymph node cannot be assessed N0: No lymph node involvement N1: Metastasis in 1 to 3 regional lymph nodes N2: Metastasis in 4 or more regional lymph nodes Mx: Distant metastasis cannot be assessed M0: No distant metastasis M1: Presence of distant metastasis Of note, involvement of nonregional lymph nodes. T1-2, N0, M0 T3, N0, M0 T4, N0, M0 T1-2, N1, M0 T3-4, N1, M0 T1-4, N2, M0 any T, any N, M1 93. If it is high before surgery, it is expected normalize following successful surgery to remove all of the cancer. Because pericolic mesenteric lymph nodes are the initial site of metastatic spread, an en bloc resection of the primary tumor with adequate margins and removal of the regional lymph nodes is recommended. The resection should include the tumor and 5 cm of normal tissue margins on each side of the tumor. At what interval of time should a follow-up colonoscopy be done after curative surgical resection of the colon cancer In the case of an obstructive cancer, the colonoscopy should be performed 3 to 6 months after surgery if no unresectable metastasis was found during surgery. Subsequent surveillance colonoscopy should be performed 1 year after surgical resection or after the initial colonoscopy done to clear the colon of synchronous lesions. If normal colonoscopy is repeated at 3 years and if that colonoscopy is normal, then repeat in 5 years thereafter. What are the most frequent sites of relapse after surgical resection of colon cancer After surgical resection, the most frequent sites of relapse are: · Liver (33%) · Lungs (22%) · Local (colon, anastomosis) or regional (21%) · Intraabdominal sites (18%) Rectal cancers have more local recurrences and less retroperitoneal node involvement when compared to colon cancer. The United States Preventative Services Task Force recommends screening not be continued after age 85 as risk exceeds the benefit (grade D). In patients age 75 to 85 years, screening is not recommended (grade C), but should be individualized based on benefits, risks, comorbidities, and life expectancy. Only limited randomized data are available to date in screening patients with inconsistent findings. No randomized clinical trial proving that screening colonoscopy reduces cancer mortality has been published. It is not until 10 years later that the mortality benefit of colonoscopy polypectomy was proven. A recent study using a pooled dataset from eight large prospective North American studies found 0. Missed lesions (52%) and incompletely resected lesions (19%) seem to account for 70% of interval cancers in this series. Are there any chemopreventive agents that have been reported to decrease the risk of adenoma recurrence List the inherited polyposis syndromes with their respective gene mutation and mode of inheritance. It is characterized by the presence of serrated polyps admixed with adenomas throughout the colon, with larger polyps in the proximal colon. Patients with Lynch syndrome are at increased risk of colon cancer but also endometrial, ovarian, gastric, urothelial, small bowel, biliary and pancreatic, sebaceous gland neoplasm, and brain cancers (usually glioblastoma). Recent analysis on the causes of deaths in Lynch syndrome show that a large proportion (61%) of the cancer deaths are now associated with noncolorectal, nonendometrial cancer. Unfortunately, there is no data to support a benefit for screening extracolonic cancers. A number of guidelines recommended screening for Lynch syndrome by site of cancer. Benign extracolonic manifestations are the following: · Skin lesions: sebaceous or epidermoid cysts, lipomas, fibromas · Osteomas · Dental abnormalities: unerupted teeth or supernumerary teeth · Congenital hypertrophy of the retinal pigment epithelium · Nasopharyngeal angiofibroma Extracolonic malignancies are the following: · Desmoid tumors (15%) · Duodenum (3%-5%) · Thyroid cancer (2%) · Brain tumor (usually medulloblastoma) (2%) · Pancreas (1. The overall burden of adenoma at the end of the treatment phase was unchanged between the two arms. Screening for colorectal neoplasms with new fecal occult blood tests: update on performance characteristics. Effect of aspirin or resistant starch on colorectal neoplasia in the lynch syndrome. Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology Practice Guideline.