Vivanza
General Information about Vivanza
Vivanza is mostly well-tolerated, however like another treatment, it could cause some unwanted effects. Common unwanted effects embrace headache, flushing, nasal congestion, dizziness, and upset stomach. These side effects are usually mild and go away on their very own. Rare however serious unwanted aspect effects might happen, such as sudden imaginative and prescient or listening to loss, and an allergic reaction. If any of those severe unwanted effects happen, medical consideration must be sought immediately.
Vivanza is available in tablets of 2.5mg, 5mg, 10mg, and 20mg. The ordinary starting dose is 10mg, and it ought to be taken about an hour before sexual activity. The dose may be adjusted primarily based on individual response and tolerability. It just isn't recommended to take more than one tablet in a 24-hour interval. The effects of Vivanza can last for about four to five hours, giving sufficient time for sexual activity.
Vivanza, like different PDE5 inhibitors, works by inhibiting the enzyme that breaks down a chemical called cyclic guanosine monophosphate (cGMP). cGMP is answerable for stress-free the graceful muscles within the penis, permitting for increased blood flow and leading to an erection. By inhibiting the breakdown of cGMP, Vivanza helps to maintain a sustained erection.
ED is a common condition that affects millions of men worldwide. It is defined as the shortcoming to get or maintain an erection agency enough for sexual activity. While occasional issue with getting an erection isn't unusual, ED is taken into account a medical drawback if it occurs persistently and affects a man's high quality of life. It can be attributable to various factors, including underlying health conditions, sure drugs, psychological elements, and lifestyle decisions.
Vivanza, also known as Levitra, is a medication used to deal with sexual function issues in men, specifically impotence or erectile dysfunction (ED). It belongs to a class of drugs called phosphodiesterase kind 5 (PDE5) inhibitors, which work by rising blood flow to the penis throughout sexual stimulation, thus aiding in reaching and maintaining an erection.
In conclusion, Vivanza is an efficient medicine for the therapy of ED. It works by increasing blood circulate to the penis, serving to men obtain and maintain an erection. It is important to consult with a doctor earlier than taking Vivanza to determine if it's the proper therapy for you. With correct use and healthy way of life changes, Vivanza can improve sexual function and improve the overall quality of life for those affected by ED.
Vivanza should not be taken with sure medications, similar to nitrates or alpha-blockers, as this can cause a harmful drop in blood stress. It is also not recommended for men who've skilled a heart assault or stroke inside the final six months. It is all the time essential to tell your physician of any medicines you take before beginning Vivanza.
While Vivanza is effective in treating ED, it does not cure the underlying cause of the situation. Therefore, it is important to address any underlying well being issues, such as diabetes, heart illness, or high blood pressure, which can contribute to ED. It can be crucial to make wholesome lifestyle modifications, corresponding to quitting smoking, lowering alcohol consumption, and sustaining a wholesome weight. These changes can enhance general health and contribute to raised sexual function.
The outstanding pathologic features of the disease are the smallness of muscles and their constituent fibers and central nucleation erectile dysfunction medication and heart disease buy cheapest vivanza and vivanza. In one group of centronuclear myopathies, there is hypotrophy of type 1 fibers (Bethlem et al; Karpati et al). Surrounding most of the centrally placed nuclei is a clear zone, in which there is a lack of organization of contractile elements. Because of central nucleation, the disease has incorrectly been referred to as myotubular myopathy, implying an arrest in development of muscle at the myotubular stage. There is evidence from electron microscopic studies of changes in the central parts of the fibers (lack of enzy matic activity in the clear zones surrounding the nuclei), leading in all probability to fiber loss. However, tubular aggregates are also the defining feature of several rare and purely myopathic syndromes: (1) a slowly progressive muscular weakness, in a limb-girdle distribution, with onset in childhood or early adult life; inheritance is either autosomal dominant or recessive in type; (2) a childhood onset of proximal weakness, easy fatigability, and myasthenic features; heredity is autoso mal recessive. This syndrome may respond to pyridostig mine; and (3) muscle pain, cramps, and stiffness induced by exercise; the cases to date have been sporadic. All the striated skeletal muscles are involved to some degree, but distinctive features are ptosis and ocular palsies combined with weakness of facial, masticatory, lingual, pharyngeal, laryngeal, and cervical muscles in most of the infants with this disease, but not in adults. Motor development is secondarily slowed, though some improvement with maturation can occur. Later, however, motor functions that had been acquired may be lost as the disease slowly advances. Abundant spon taneous activity should suggest the diagnosis of centro nuclear myopathy (Griggs et al). Heckmatt and colleagues classified this disorder into three types, based on severity, mode of presentation, and affin sections. By electron microscopy, the bundles of tubular aggregates are sharply demarcated from myofibrils. In none of these additional types has the pattern of inheritance or the gene locus been identified. Some of these myopathies (multicore [min icore], of impulses across neuromuscular junctions-as occurs in myokymia, hypocalcemic tetany, and pseudohypo parathyroidism. In other states, the innervation of muscle is normal, but contraction persists despite attempts at relaxation (myotonia). Or, after one or a series of contrac tions, the muscle may be slow in decontracting, as occurs in paradoxical myotonia and hypothyroidism. In the contracture of McArdle phosphorylase deficiency and phosphofructokinase deficiency, muscle, once contracted, lacks the energy to relax. In yet another type of muscle stiffness, the muscle may ripple or respond to percus sion by mounding and rapidly contrasting and relaxing. Two other types, disproportion and congenital fiber type congenital fiber type predominance, origi nally designated as congenital myopathies, have proved to be nonspecific histochemical alterations observed in many infants and children with congenital developmen tal abnormalities, delays in motor development, and other conditions. Other putative congenital myopathies reducing body, trilaminar, and cap disease; zebra body; and familial myopathy with lysis in type 1 fibers, include so-called among others. They most likely also represent nonspe cific reactions in muscle or fixation artifacts; as yet there is no evidence that any one of them represents a clinico pathologic entity. Each of these conditions evokes the complaint of cramp or spasm, which is variably painful and interferes with free and effective voluntary activity. As stated in the introductory section, there is cur rently no treatment for any of the congenital myopathies. Cramps often occur during the night, after a day of unusually strenu ous activity; less frequently they occur during the day, either during a period of relaxation or occasionally after a strong voluntary contraction or postural adjustment. A random restless or stretching movement may induce a hard contraction of a single muscle (most frequently of the foot or leg) that cannot be voluntarily relaxed. The muscle is visibly and palpably taut and painful, and the condition is readily distinguished from an illusory cramp, in which the sensation of cramp is experienced with little or no contraction of muscle. The latter phenomenon may occur in normal persons as well as in those with periph eral nerve diseases. Massage and vigorous stretch of the cramped muscle will cause the spasm to yield, although for a time the muscle remains excitable and subject to recurrent cramps. Visible fasciculations may precede and follow the cramp, indicating excessive excitability of the terminal branches of motor neurons supplying the muscle. Sometimes the cramp is so intense that the muscle is injured; it remains sore to touch and painful upon use for a day or longer. Cramps of precordial chest muscles or diaphragm may arouse fear of heart or lung disease. Indeed, they represent the main problems faced by the clinician studying neuromuscular diseases of the infant. Their hereditary nature, their progression to fatal outcome or delayed motor attainments, and their tendency in certain instances to produce disabling con tractures are shared with the primary muscle diseases. The proper application of current laboratory techniques sets them apart in most instances. In deference to their neuronal origin, we have placed them with the other degenerative diseases in Chap. Muscles may go into spasm because of an unstable depolarization of motor axons, sending volleys of activity in motor units. Why cramps should be painful is not known; probably the demands of the overactive muscle exceed metabolic supply, causing a relative ischemia and accumulation of metabolites. Cramps are known to increase in frequency under certain conditions and with certain diseases. Dehydration and excessive sweating predispose to cramping and are a constant threat to athletes. Exertional cramps are elicited more easily than usual in motor sys tem disease, hypothyroidism, and in chronic polyneu ropathies. For example, the calf muscle on one side is subject to severe recurrent cramps after decompression of the Sl root for lumbar disc disease; in extreme cases, the muscle hypertrophies after long periods of intermittent cramping.
Intoxications with pyridoxine or metals account for a few chronic sensory neuropathies erectile dysfunction ed drugs 20 mg vivanza buy with visa. Despite all these consider ations, we still regularly encounter patients in whom the cause is not disclosed by any of the available tests. We have watched helplessly as some of these patients were reduced to a bed and wheelchair existence and others suf fered from pain until they became dependent on opiates. Table 46-7 lists the laboratory tests that are useful in the investigation of this group of neuropathies, with electrophysiology being most valuable. The observations of Dyck and coworkers (1981), referred to in the introduction to this chapter, are of interest in this respect. In a series of 205 patients who were referred to the Mayo Clinic with neuropathies of unknown cause, 86 were found to have an inherited form of disease. With appropriate genealogic data, the diagnoses of the peroneal muscular atrophy of Charcot-Marie-Tooth disease can usually be made on clinical grounds alone (high arches, distal foreleg atrophy, chronicity, etc. Additional runts are frequent sprained ankles and the need to tape the ankles dur ing adolescence in order to run or participate in sports. Sometimes, the absence of ankle reflexes or foot deformities in their relatives discloses the diagnosis. A comment has already been made regarding the utility of such testing and the small number of mutations that give rise to over one-third of cases of inherited sensorimotor neuropathy. Numerous easily accessible algorithms for genetic testing have been published, similar to the guidance in the article by Saporta and colleagues, that are based on inheritance, nerve conduction velocity, and clinical features and we have not reproduced them here. Slowly progressive polyneuropathy with features of central nervous system degeneration, particularly cer ebellar ataxia, most often has a genetic basis, but a small number are found to be the result of a genetic metabolic disorder such as a leukodystrophy. In contrast, a few young patients have come to our atten tion in whom a gradually progressive polyneuropathy that evolved over almost a decade turned out to be an acquired chronic inflammatory demyelinating condition rather than the expected genetic type. The absence of a family history of neuropathy and of high arches and heterogeneous slowing of both nerve conduction velocities and reductions in motor amplitudes on the nerve conduction studies provided runts to the acquired nature of the condition. Finally, it should be conceded again that even after the most assiduous clinical and laboratory investigation, a substantial proportion of chronic neuropathies remain unexplained. Some instances of mononeuritis multiplex, especially when associated with cryoglobulinemia, are also characterized by remissions and relapses over many years, although the remissions are incomplete. It is self-evident that patients who have recovered from an episode of alcoholic-nutritional or toxic polyneuropathy will develop a recurrence if they again subject themselves to intoxication or nutritional deficiency. Neuropathic symptoms that fluctuate in relation to environmental factors such as cold (cryoglobulinemia), heat (Fabry and Tangier diseases), or intermittent expo sure to heavy metal or other type of poisoning may simu late an inherently relapsing polyneuropathy. Certain neuropathies of this type-traceable mainly to polyarteritis nodosa or other vasculitides, leprosy, sarcoid, or diabetes-have already been discussed and are the main causes of the multiple mononeuropathy pattern. In addition to the signs of mononeuropathy multiplex, pain overlying the site of nerve infarction or distally is characteristic. In identifying a process as caused by single or mul tiple mononeuropathies, the reader can refer to Table 46-1, which lists the roots, nerves, and muscles that are involved in particular movements, and to Table 46-4, which gives the main etiologies of mononeuropathy multiplex. Some are a result of infiltration by tumor, compression, obscure infections (possibly viral), and the delayed effects of radiotherapy. Of obvious cause are those that result from trauma, in which the arm is hyperabducted or the shoulder violently separated from the neck. Difficult births are an impor tant source of such traction injuries to the plexus, but their nature is also evident. Rarely, the brachial plexus or other peripheral nerves may be damaged at the time of an electrical injury, either from lightning or from a household or industrial source (see "Electrical Injuries" in Chap. Direct compression of parts of the plexus by adjacent skeletal anomalies (cervical rib, fascial bands, narrowed thoracic outlet) represents another, still some what controversial, category of brachial plexus injury. A subcutaneous or intramuscular injection of vaccine or foreign serum was in the past sometimes followed by a brachial plexopathy, usually partial. There are also plexus lesions of presumed toxic nature, such as those following heroin injection. Granulomatous diseases such as sarcoid and secondary inflamm atory processes related to lym phoma may implicate a plexus and an ischemic condition resulting from thrombosis of the subclavian artery or vein (Paget-Schrotter syndrome) is known. More common, however, is an idiopathic brachial plexus neuritis of obscure origin, also called Parsonage Turner syndrome, discussed further on. It stands apart as a special clinical entity, often difficult to distinguish from other types of brachial and axillary pain. Some of these cases, surprisingly, are familial; others occur in small out breaks, but most are sporadic. In assessing the type and degree of plexus injury, electrophysiologic testing is of particular importance. Early after a traumatic injury or other acute disease of the plexus, the only electrophysiologic abnormality may be an absence of late responses (F wave). After 7 to 10 days or more, as the process of wallerian degeneration pro ceeds, sensory potentials are progressively lost and the amplitudes of compound muscle action potentials are variably reduced. Fibrillation potentials, indicative of denervation, then begin to appear in the corresponding muscles. In more chronic cases, all of these features are evident when the patient is first studied. The pattern of denervated muscles allows a dis tinction to be made between a plexopathy, radiculopathy, and mononeuritis multiplex based on the known pat terns of muscle innervation (see Table 46-1). If denerva tion changes are found in the paraspinal muscles, the source of weakness and pain is in the intraspinal roots, proximal to the plexus. We often resort to the illustrations of individual nerves and plexuses that are well demonstrated in the mono graph published by the Guarantors of Brain.
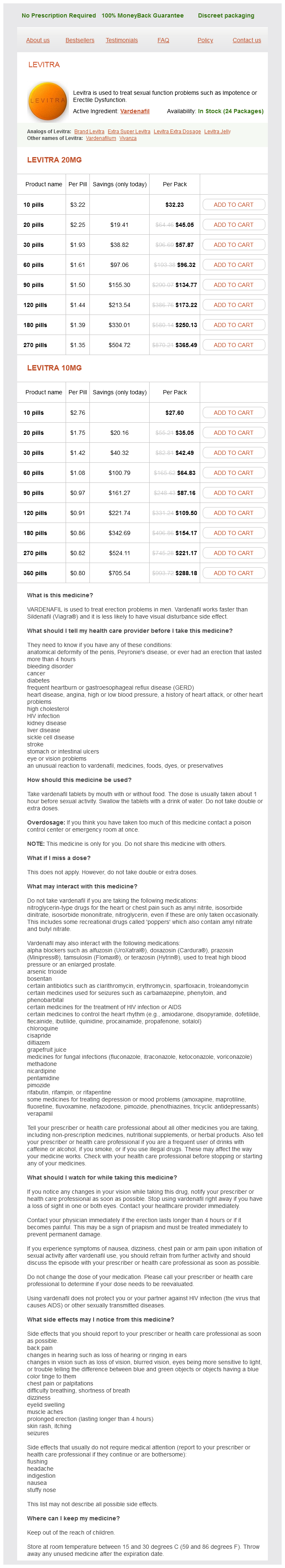
Vivanza Dosage and Price
Levitra 20mg
- 10 pills - $32.23
- 20 pills - $45.05
- 30 pills - $57.87
- 60 pills - $96.32
- 90 pills - $134.77
- 120 pills - $173.22
- 180 pills - $250.13
- 270 pills - $365.49
Levitra 10mg
- 10 pills - $27.60
- 20 pills - $35.05
- 30 pills - $42.49
- 60 pills - $64.83
- 90 pills - $87.16
- 120 pills - $109.50
- 180 pills - $154.17
- 270 pills - $221.17
- 360 pills - $288.18
In patients who recover erectile dysfunction rates discount vivanza generic, improvement begins within a few weeks, first in ocular movement, then in other cranial nerve functions. The three types of botulinum toxins-A, B, and E cannot be distinguished by their clinical effects alone, so that the patient should receive the trivalent antiserum as soon as the clinical diagnosis is made. This antitoxin can be obtained from the Centers for Disease Control and Prevention, Atlanta, Georgia. An initial dose of 10,000 U is given intravenously after intradermal testing for sensitivity to horse serum, followed by daily doses of 50,000 U intramuscularly until improvement begins. Penicillin or metronidazole are given to eradicate the organism in a wound (but are not as useful if the exogenous preformed toxin has been ingested). Guanidine hydrochloride (50 mg/kg) has been somewhat useful in reversing the weakness of limb and extraocular muscles. The therapeutic injection of small quantities of botulinum toxm into a muscle affected by dystonia or spasticity will weaken or paralyze it for weeks to months (see Chap. Mild symptoms of botulism can occur with relatively large doses, mainly affecting the oropharyngeal and ciliary muscles. Ergot is used therapeutically to control postpartum hemorrhage caused by uterine atony; one of its alkaloids, ergotamine, is used in the treatment of migraine (see Chap. Chronic and repeated use of the drug is the usual cause of ergotism; acute overdosage in the postpartum state or in the treatment of migraine may cause an alarming rise in blood pressure. Two types of ergotism are recognized: gangrenous, which is caused by a vasospastic, occlusive process in the small arteries of the extremities, and convulsive, or neurogenic, ergotism. The latter is characterized by fasciculations, myoclonus, and spasms of muscles, followed by seizures. In nonfatal cases, a tabes-like neurologic syndrome may develop, with loss of knee and ankle jerks, ataxia, and impairment of deep and superficial sensation. The pathologic changes consist of degeneration of the posterior columns, dorsal roots, and peripheral nerves, but they have been poorly described. The relation of these changes to ergot poisoning is not clear, because most of the cases occurred in areas where malnutrition was endemic. Lathyrism Lathyrism is a neurologic syndrome characterized by the relatively acute onset of pain, paresthesia, and weakness in the lower extremities, progressing to a permanent spastic paraplegia. It is a serious medical problem in India and in some North African countries and is prob ably caused by a toxm contained in the chickling vetch pea, Lathyrus, a legume that is consumed in excess quan tities during periods of famine. Most of them cause only transient gastrointestinal symptoms but some elaborate toxins that can be fatal. The most important of these toxins are the cyclopeptides, which are contained in several species of Amanita phalloides and m uscaria and account for more than 90 percent of fatal mushroom poisonings. Symptoms of poisoning with Amanita usually appear between 10 and 14 h after ingestion and consist of nausea, vomiting, colicky pain, and diarrhea, followed by irritability, restlessness, ataxia, hallucinations, con vulsions, and coma. Other important mushroom toxins are methylhydra zine (contained in the Gyromitra species) and muscarine (Inocybe and Clitocybe species). The former gives rise to a clinical picture much like that caused by the cyclo peptides. The symptoms of muscarine poisoning, which appear within 30 to 60 min of ingestion, are essentially those of parasympathetic stimulation-miosis, lacrima tion, salivation, nausea, vomiting, diarrhea, perspiration, bradycardia, and hypotension. If vomiting has not occurred, it should be induced with ipecac, following which activated charcoal should be administered orally in order to bind what toxm remains in the gastrointestinal tract. A local poison control center may help identify the poisonous mushroom and its toxin. Even more important, the gathering and ingestion of field varieties of mushrooms should be left to those absolutely certain of their identity. The responsible toxm causes a predominantly motor poly neuropathy, probably of axonal type. Except for a normal spinal fluid protein concentration, the disorder closely resembles Guillain-Barre syndrome and tick paralysis (see later), and its recognition depends on awareness of ingestion of the fruit in endemic areas. It results from eating fish that have fed on toxin-containing microscopic dinoflagel lates. Reef fish and shellfish ingest high concentrations of these organisms during periodic upswings in the popula tion of the dinoflagellates. Although the toxms differ (tetrodotoxin-puffer fish; ciguatoxm-snails; saxitoxm and brevetoxm-shellfish), the neurologic and gastrointestinal symptoms that follow the ingestion of poisoned fish are similar. These are followed by paresthesias that begin periorally and then involve the limbs distally. In puffer fish poisoning, and in advanced stages of poisoning from other fish, weakness occurs, and there have been a few reports of coma and of respiratory failure. The recognition of this type of fish poisoning is straightforward in endemic areas, in some of which there is a seasonal clustering of cases. In tourists returning home from endemic areas, and in persons consuming imported fish, the illness may be mistaken for Guillain Barre syndrome. Supportive treatment is all that is required but treatment with intravenous mannitol is said to hasten recovery. Pearn has reviewed the biochemistry and physiologic and clinical effects of the various marine toxins and points out a form of chronic intoxication that is apparently endemic in certain island communities. The problem of distinguishing this syndrome from depression is acknowledged by the author and the cases on which we have consulted locally almost always fall into the psychiatric category.